Mobility of oculomotor system and lability of visual analyzer in patients with primary open-angle glaucoma
V.A. Putienko
V.S. Ponomarchuk, Dr. Sc. (Med), Prof.
Filatov Institute of Eye Disease and Tissue Therapy
Odessa, Ukraine
E-mail: alputienko@yandex.ru
Purpose: to perform a comparative assessment of oculomotor system mobility and visual system lability in patients with primary open-angle glaucoma (POAG) of stages II and III with compensated IOP.
Material and Methods: A total of 38 patients (38 eyes) with POAG were examined. II stage was in 20 eyes and III stage was in 18 eyes. Oculomotor system mobility was studied according to impulse move frequency index, and visual system lability was assessed according to indices of critical flicker fusion and appearance frequency using an ophthalmic photomyostimulator unit (FMS-1).
Results: Both in stage II and III of POAG, functional mobility of the oculomotor system was significantly lower as compared to the norm (р<0.05). Herewith, that was significantly lower in stage III than in stage II (р<0.05). Functional lability of the visual system in patients with stage POAG does not differ significantly from the norm. However, there is a significant reduction in visual system functional lability in stage III POAG as compared with the norm (р<0.01) and stage II of the disease (р<0.05).
Conclusions: Obtained data indicate the need of searching the methods of stimulations of oculomotor system functional mobility and visual system lability in patients suffering from glaucoma, which can bring a vast improvement in the quality of life of these patients.
Key words: primary open-angle glaucoma, oculomotor system, visual system lability, ophthalmic photomyostimulator
Introduction
The oculomotor system is a part of the sensory system of the eye which transmits and process the information about the outer environment. The main functions of the oculomotor system are eye movements towards a visual object, maintenance of binocular vision function and visual spatial localization [2, 3, 6].
Disorders in sensory function have been shown to be accompanied by oculomotor disorders as unstable fixation, an increase in frequency of saccades with a parallel decrease in their accuracy and velocity, disorders of the accuracy and velocity of smooth pursuit eye movements, reading speed, and visual object recognition rates in comparison with persons with normal vision [1-6].
Kefi Naissan has investigated that functional activity of the oculomotor system is significantly decreased and lability of the visual system is reduced in myopia patients; herewith, high myopia patients have oculomotor function significantly decreased as compared with mild myopia patients. Central vision loss caused by degenerative changes in the macular area also decreases functional parameters of the oculomotor system [1].
Visual fields loss at initial stages of glaucoma, and, thereafter, central visual loss in progression of the latter, can significantly increase the load on the the oculomotor system of the eye and decrease its functional activity. To our best knowledge, no investigations of oculomotor functions in patients with different glaucoma progression stages have been performed, which was the background for our study.
The purpose of the present paper was a comparative assessment of the mobility of the oculomotor system and the lability of the visual system in patients with primary open-angle glaucoma (POAG) of stages II and III with compensated intraocular pressure.
Material and Methods
A total of 38 patients (38 eyes) with POAG with drug-compensated IOP were observed. Glaucoma was diagnosed according to the data of ophthalmoscopy, gonioscopy, tonogrophy, computed static perimetry and optical coherence tomography (OCT). OCT was performed using Carl Zeiss (CIRRUS Photo 800) and a mean thickness of retinal nerve fiber layer (RNFL) was considered. POAG II and III stages were noted in 20 patients (20 eyes) and in 18 patients (18 eyes), respectively.
In a group of stage II POAG patients, mean age was 68 SD (4.93) y/o, mean visual acuity was 0.78 SD (0.13). A mean value of Maklakov tonometry IOP was 17.26 SD (1.0) mm. A mean thickness of RNFL according to OCT was 67.3 SD (2.9) mm and cup-to-disc ratio was 0.74 SD (0.035).
In patients with POAG stage III, mean age was 71 SD (4.67) y/o, mean visual acuity was 0.32 SD (0.15). The mean value of Maklakov tonometry IOP was 17.98 SD (1.1) mm. The mean thickness of RNFL according to OCT was 54.9 SD (4.4) mm and cup-to-disc ratio was 0.86 SD (0.031).
Mobility of the oculomotor system and lability of the visual system were assessed using an ophthalmic photomyostimulator unit (FMS-1). Functional mobility of the oculomotor system was determined according to impulse move frequency (IMF, Hz) in three kinetic modes: horizontal (H-mode), vertical (V-mode), and chaotic (C-mode) and lability of the visual system was defined by critical flicker fusion frequency (CFFF, Hz) and critical flicker appearance frequency (CFF, Hz) in three kinetic modes and a static (motionless) mode with a central fixation point. Data from literature served as normal values for IMF, CFFF, and CFAF parameters [1].
STATISTICA 7.0 software package was used for statistic data processing. Data analysis was performed using pairwise Student (t) criterion and nonparametric ?2 criterion. Critical p-level when testing statistical hypothesis was equal to 0.05.
Results
A mean value for impulse move frequency (IMF) in patients with stage II POAG in H-mode was 2.28±0.08 Hz with minimal and maximal values of 1.6 Hz and 2.9 Hz, respectively; coefficient of variation was equal to 12.8%.
V-mode IMF index averaged 2.22±0.08 Hz with 1.5 Hz and 2.8 Hz as maximal and minimum values, respectively; coefficient of variation was 14.2%.
C-mode was characterized with random appearance of stimuli in a certain part of the visual field; in this mode, IMF index in stage II POAG patients averaged (2.05±0.08) Hz with 1.5 Hz as minimum and 2.9 Hz as maximum; coefficient of variation was 15.1% (Table 1).
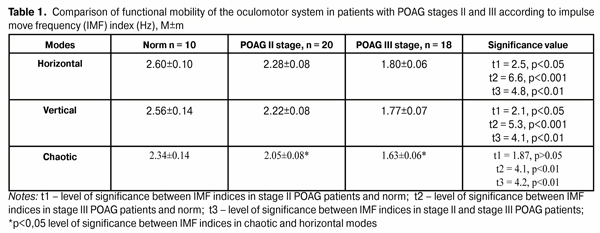
In patients with stage III POAG, a mean value of IMF in H-mode was 1.80±0.06 Hz with minimal and maximal values of 1.4 Hz and 2.4 Hz, respectively; coefficient of variation was equal to 13.9%.
V-mode IMF index averaged 1.77±0.07 Hz with 1.4 Hz and 2.5 Hz as maximal and minimum values, respectively; coefficient of variation was 15.3%.
In C-mode, IMF index in stage II POAG patients averaged 1.63±0.06 Hz with 1.2 Hz as minimum and 2.2 Hz as maximum; coefficient of variation was 15.7% (Table 1).
Statistic analysis showed that IMF indices in stage II POAG patients did not differ significantly in H- and V-modes. Herewith, IMF index was significantly higher, by 10.1%, in H-mode (p<0.05) and not significantly higher, by 7.7%, in V-mode as compared with C-mode (p>0.05).
In stage III POAG patients, no significant difference was noted in IMF values in horizontal and vertical modes; and H-mode IMF index was by 9.4% higher than that in C-mode (p<0.05). Also, likewise in stage II POAG patients, IMF indices in V- and C-modes did not differ significantly (p>0.05) (Table 1).
In stage II POAG, IMF indices in H- and V-modes was significantly lower by 0.32 Hz (12.3%) and by 0.34 Hz (13.3%), respectively, as compared with the norm; herewith, a decrease of IMF index by 0.29 Hz (12.4%) in C-mode was not significant compared with norm.
In patients with stage III POAG, there was a significant decrease in IMF indices in H-, V-, and C-modes, as compared with norm, by 0.8 Hz (30.7%), 0.79 (30.9%) Hz, and 0.67 (29.1%) Hz, respectively.
Comparison of IMF indices in glaucoma patients with stages II and III revealed significant differences in the three modes studied. Thus, mean IMF index of stage III glaucoma patients in horizontal, vertical, and chaotic modes was lower than that in stage II glaucoma patients by 0.48 Hz (21.1%), by 0.45 (20.3%) Hz and by 0.42 (20.5%) Hz, respectively (Table 1).
Thus, functional mobility of the oculomotor system is significantly reduced in patients with stage II POAG compared to norm. With the glaucoma progression as far as stage III, a further decrease in functional mobility of the system is observed compared both to the norm and POAG stage II.
Functional lability of the visual system was defined according to two parameters: critical flicker fusion frequency (CFFF) and critical flicker appearance frequency (CFAF) in a static (motionless) mode in the central point (cp) of fixation (CFFFcp, CFAFcp) and in kinetic horizontal, vertical, and chaotic modes.
Static CFFFcp index of visual system lability in stage II POAG averaged 43.4±0.6 Hz and did not differ significantly from the norm (р>0.05). CFFF in the kinetic horizontal, vertical, and chaotic modes was 38.6±0.8Hz, 38.8±0.9Hz, and 38.9±0.9Hz, respectively. All the values in the kinetic modes did not differ significantly between each other and were significantly lower than that in the static mode (p<0.05). Thereby, no significant difference was noted between the CFFF values in the three kinetic modes and the norm (Table 2).
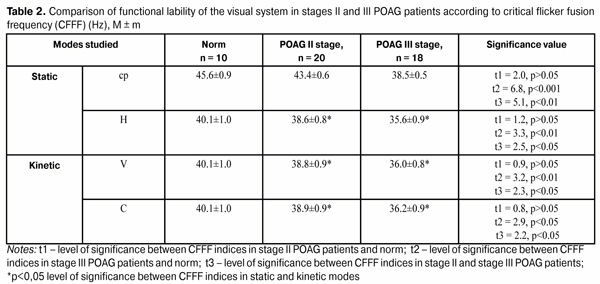
In stage III POAG patients, a mean value of CFFF in the static mode was 38.5±0.5 Hz while kinetic horizontal, vertical, and chaotic CFFF values were 35.6±0.9 Hz, 36.0±0.8 Hz, and 36.2±0.9 Hz, respectively. Likewise in stage II POAG patients, all indices in the kinetic mode did not differ from each other and, thereby, were significantly lower than that in the static mode (p<0.05). It is necessary to highlight a significant decrease in CFFF indices in stage III POAG both in the static (р<0.001) and the three kinetic (р<0.01) modes as compared with the norm (Table 2).
A comparison of visual system lability indices in patients with POAG stages II and III according to CFFF showed a significant decrease both in the static mode (р<0.01) and the three kinetic modes (р<0.05) in patients with POAG stage III as compared to stage II glaucoma patients (Table 2).
Hereafter, functional lability of the visual system was studied according to critical flicker appearance frequency. In stage II POAG patients, a CFAFcp value averaged 39.7±0.7 Hz in the static mode and that was 36.9±1.3 Hz, 36.9±1.2 Hz, and 37.1±1.2 Hz in the kinetic horizontal, vertical, and chaotic modes, respectively. All CFAF values did not differ significantly from the norm (р>0.05). Herewith, mean CFAF values in the kinetic modes were significantly lower than those in the static mode (Table 3).
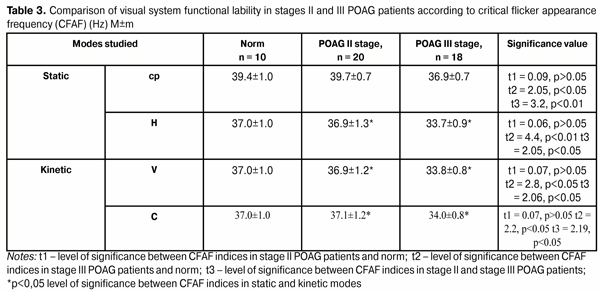
In patients with POAG stage III, a mean CFAFcp value in the static mode was equal to 36.9±0.7 Hz and significantly lower comparing with the norm (р<0.05) and with stage II POAG patients (р<0.01). All kinetic mode values were also significantly lower than normal ones and than those in stage II POAG patients (р<0.05).
Likewise in patients with POAG stage II, all kinetic indices were lower than static ones (р<0.05) (Table 3).
In patients with POAG stage II, CFAF index was significantly lower by 2.8 Hz (6.6%) (р<0.05) compared to CFFF index. CFFF and CFAF indices in the kinetic modes did not differ significantly in stage II POAG patients (p>0.05).
In patients with POAG stage III, no statistically significant differences were noted between CFFF and CFAF indices both in the static and kinetic modes (p>0.05).
Thus, visual system functional lability of stage II POAG patients does not differ significantly from the norm by every index. In stage III POAG patients, a significant decrease in functional lability of the visual system is noted in all indices studied comparing both with the norm and with stage II glaucoma patients.
The study performed allow us to conclude that glaucoma progressing to stage II so far leads to a significant reduction in functional mobility of the oculomotor system as compared with the norm. Glaucoma progressing to stage III is accompanied by the further apparent reduction in oculomotor system functional mobility. All indices of oculomotor system mobility are significantly lower in stage III POAG patients than those in stage II.
Functional lability of the visual system in glaucoma patients is affected in a less degree. Thus, in stage II glaucoma, visual system lability does not differ from the norm. A significant reduction in functional lability of the visual system is observed in stage III POAG as compared with stage II.
Thus, obtained data indicate the need of searching the methods of stimulations of oculomotor system functional mobility and visual system lability in patients suffering from glaucoma, which can bring a vast improvement in the quality of life of these patients.
References
1. Kefi Naissan. diagnostic significance of the improved method for detection of oculomotor system mobility and visual system lability in patients with myopia and macular dystrophy: thesis for Cand. Sc. (Med.). Odessa; 2013. 162p. Russian.
2. Levin LA, Nilsson SFE, Ver Hoeve J, Wu SM. Adler’s physiology of the eye.11th ed. Elsevier Inc.; 2011. 796p.
3. Bucci MP, Kapoula Z. Binocular coordination of saccades in 7 years old children in single word reading and target fixation. Vision Research. 2006;46 (4): 457–466. http://dx.doi.org/10.1016/j.visres.2005.05.004
Crossref Pubmed
4. Bullimore MA, Bailey IL. Reading and eye movements in age–related maculopathy. Optom. Vis. Sci. 1995;72:125–138.
Crossref Pubmed
5. Land MF. Vision, eye movements, and natural behavior. Vis Neurosci. 2009;26(1):51–62. DOI: 10.1017/S0952523808080899
Crossref Pubmed
6. Leigh RJ, Zee DS. The Neurology of Eye Movements. 4th ed. New York: Oxford University Press; 2006. 54p.