J.ophthalmol.(Ukraine).2018;4:44-48.
|
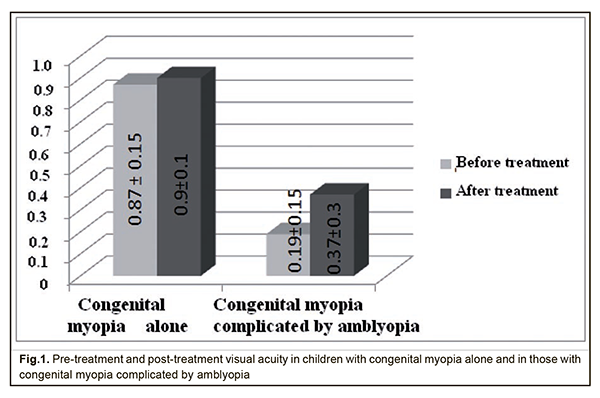
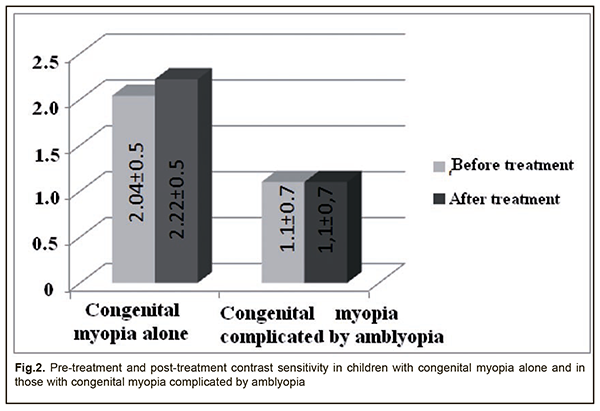
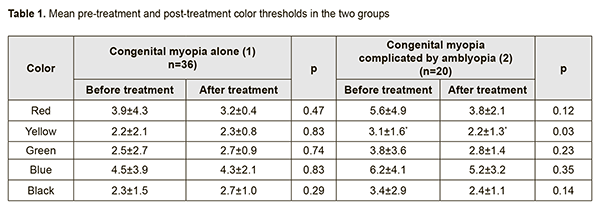
https://doi.org/10.31288/oftalmolzh201844448 Received: 13 June 2018; Published on-line: 31 August 2018 Pre-treatment and post-treatment visual functions in congenital myopia alone versus congenital myopia complicated by amblyopia A.Iu. Mukhina1, Post-grad Student, I.M. Boichuk2, Dr Sc (Med), L.D. Zhuravliova1, MD 1 Regional Pediatric Clinical Hospital; Ivano-Frankivsk (Ukraine) 2 Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine; Odessa (Ukraine) E-mail: iryna.ods@gmail.com TO CITE THIS ARTICLE: Mukhina AIu, Boichuk IM, Zhuravliova LD. Pre-treatment and post-treatment visual functions in congenital myopia alone versus congenital myopia complicated by amblyopia. J.ophthalmol.(Ukraine).2018;4:44-48. https://doi.org/10.31288/oftalmolzh201844448 Background: Congenital myopia is a particular form of refractive error which develops prenatally. The reported incidence of myopia in newborns has varied widely, ranging from 6–15% to 25–50%. In the vast majority of cases, myopia in newborns is a transient refractive myopia due to an increased refractive power of the lens, low effect of cycloplegics on the immature ciliary muscle, and some mismatch between some anatomical and optical parameters of refraction. In congenital myopia, there are the blurred out-of-focus images of fixated objects on the foveal and macular regions of the retina, which disrupts normal development both of visual acuity and all central vision functions and structures. Congenital myopia is often associated with amblyopia, which requires specific and durable treatment options. Therefore, timely diagnosis is required to differentiate between the two conditions. Purpose: To compare visual function parameters before and after pleoptic and orthoptic treatment in congenital myopia alone without versus congenital myopia complicated by amblyopia. Materials and Methods: Eighteen children (36 eyes; Group 1) with congenital myopia alone and 11 children (20 eyes; Group 2) with congenital myopia complicated by amblyopia, aged 5 to 12 years underwent an eye examination before and after treatment. Contrast sensitivity was measured using the advanced Bausch & Lomb charts (2013), and color thresholds were measured using the charts we have developed previously (Patent of Ukraine for the Utility Model №114,858 issued 01.2017, “Method for measuring color thresholds in young children”). Treatments used included appropriate optical correction of the refractive error, training of accommodation, pleoptic treatment (illumination of the macula with or without the use of color filters; phosphene stimulation; magnetic stimulation using ATOS apparatus; laser stimulation using LAST and RADUGA apparatuses); computer-assisted treatment; light and color stimulation using ASO and Rucheiok apparatuses; CAM stimulation; and physical therapy (electrophoresis using Aloe vera extract with ascorbic acid; massage of the cervical spine). Results: After treatment, mean visual acuity improved significantly from 0.87±0.15 to 0.9±0.1 in Group 1, and from 0.19±0.15 to 0.37±0.3 in Group 2 (p < 0.05). In addition, Lang II random-dot test and Titmus stereo fly test demonstrated that the stereovision improved in children with amblyopia (Group 2). Moreover, the time till the occurrence of stereo effect improved from 6.6±3.0 sec to 5.33±3.2 sec in Group 1 (p < 0.05). Furthermore, contrast sensitivity increased from 2.04±0.5 points to 2.22±0.5 points in Group 1, and did not change from baseline (1.1±0.7 points) in Group 2. Improvements in red, yellow, blue and green thresholds in Group 2 were more substantial than those in Group 1, and improvement in yellow threshold in Group 2 (p = 0.03) and those in red and blue thresholds in Group 1 were statistically significant. Conclusion: Our pleoptic and orthoptic treatment substantially improved visual acuity and improved stereovision both in patients with congenital myopia and in those with congenital myopia complicated by amblyopia. The two groups, however, demonstrated different changes in contrast sensitivity and color perception. The findings indicate that administration of any concomitant therapy for myopia should depend on the presence of amblyopia, and warrant further research on this subject. Keywords: congenital myopia, amblyopia in the presence of myopic refractive error, visual function parameters, treatment Introduction Congenital myopia is a particular form of refractive error which develops prenatally. The reported incidence of myopia in newborns has varied widely, ranging from 6–15% [1, 2] to 25–50% [3]. In the vast majority of cases, myopia in newborns is a transient refractive myopia due to an increased refractive power of the lens, low effect of cycloplegics on the immature ciliary muscle, and some mismatch between some anatomical and optical parameters of refraction [4]. Congenital myopia accounts for a rather low percentage of the total pediatric eye disease burden, affecting 0.2 to 0.5 percent of infants annually, and is accompanied by astigmatism in 42-50% of cases. A reduction of congenital astigmatism takes place in the first years of life, whereas myopic astigmatism increases with age [5, 6]. In addition, congenital myopia is important both from a public health and social perspective, since it is a major cause of poor vision and visual incapacity in children. Moreover, high myopia is a major clinical and/or anatomical cause of blindness and visual impairment in those attending boarding schools for the blind and visually impaired children, accounting for 7.4-18.2%; of the individuals with myopia-induced visual incapacity, 56% have been found to have congenital myopia [7, 8]. Inheritance plays an important role in the etiology of congenital myopia, and 54.6–65% of cases with congenital myopia are those with congenital hereditary myopia [4, 9, 10]. However, Paramei and Sidorenko have reported that congenital myopia was not hereditary in 70% of cases. They believe that “congenital myopia is a type of perinatal injury to the visual system” which develops due to the following factors: pregnancy toxemia, threatened miscarriage, intranatal disorders (like mismatch between the size of the fetus and the maternal pelvis, preterm labor, or nuchal cord), and neonatal disorders (like anemia, congenital hip dislocation, hemolytic disease of newborn, pneumonia, pylorostenosis, perinatal encephalopathy, etc.) [5, 7, 10]. In congenital myopia, there are the blurred out-of-focus images of fixated objects on the foveal and macular regions of the retina, which disrupts normal development both of visual acuity and all central vision functions and structures. Besides a high myopic refraction, the immature visual system is a major cause of low vision in children with congenital myopia. In amblyopia, the reduction in visual functions (like best-corrected visual acuity and color vision) depends on the type of amblyopia [11-13], and stereopsis is also impaired [14]. Anomaloscope studies have reported high green and red color thresholds for an amblyopic eye in myopic refraction [15]. Decreased contrast sensitivity at high spatial frequencies has been observed in eyes with a decrease in central vision that was uncorrectable with glasses or lenses due to impaired optic nerve pathways (amblyopia and myopia) [16-18]. A comprehensive stepwise approach to managing amblyopia is the most common today, and includes (a) appropriate optical correction of the refractive error, (b) pleoptic treatment with common techniques like light stimulation, electric stimulation, phosphene stimulation, magnetic stimulation, reflex therapy, spectral biorhythmic stimulation, computer-assisted treatment, techniques for improving binocular vision, physical therapy (like electrophoresis or massage), and treatments with drugs aimed at improving hemodynamics, metabolism, blood supply and neurotransmission in the retina, optic nerve and structures of the superior visual system [19-21]. The efficacy of treating amblyopia in myopes is still to be improved. A search is underway for a differential approach to administering various procedures for this type of amblyopia [15, 21, 22]. The purpose of the study was to compare visual function parameters before and after pleoptic-and-orthoptic treatment in congenital myopia alone without versus congenital myopia complicated by amblyopia.. Materials and Methods Eighteen children (36 eyes; Group 1) with congenital myopia alone and 11 children (20 eyes; Group 2) with congenital myopia complicated by amblyopia, aged 5 to 12 years underwent an eye examination before and after treatment. Mean myopia was of 7.01±4.2D in Group 1 and 6.5±4.0D in Group 2. In addition, astigmatism was ≤1.5 D in all children, and 2 children in Group 2 had anisometropia >2.0 D. In Group 2, 11, 6 and 3 eyes had low, moderate and high amblyopia, respectively. An eye examination included near and far uncorrected and best-corrected visual acuity, refractometry, cycloplegic retinoscopy, ultrasonic biometry (anterior-posterior axis), ophthalmoscopy, and biomicroscopy. In addition, the children had the type of their binocular vision determined with the color test, and had their stereopsis thresholds measured. Contrast sensitivity was measured using the advanced Bausch & Lomb charts (2013), and color thresholds were measured using the charts we have developed previously (Patent of Ukraine for the Utility Model №114,858 issued 01.2017, “Method for measuring color thresholds in young children”). A comprehensive treatment included appropriate optical correction of the refractive error, training of accommodation, pleoptic treatment (illumination of the macula with or without the use of color filters; phosphene stimulation; magnetic stimulation using ATOS apparatus; laser stimulation using LAST and RADUGA apparatuses); special computer software; light and color stimulation using ASO and Rucheiok apparatuses; CAM stimulation; physical therapy (electrophoresis using Aloe vera extract with ascorbic acid; massage of the cervical spine). Results After treatment, mean visual acuity improved significantly from 0.87±0.15 to 0.9±0.1 in Group 1, and from 0.19±0.15 to 0.37±0.3 in Group 2 (p < 0.05; Fig.1). In addition, Lang II random-dot test and Titmus stereo fly test demonstrated that the stereovision improved in children with amblyopia (Group 2). Moreover, the time till the occurrence of stereo effect improved from 6.6±3.0 sec to 5.33±3.2 sec in Group 1 (p < 0.05). Furthermore, contrast sensitivity increased from 2.04±0.5 points to 2.22±0.5 points in Group 1, and did not change from baseline (1.1±0.7 points) in Group 2 (Fig. 2). Therefore, our treatment resulted in an improvement of contrast sensitivity in patients with congenital myopia, but did not improve contrast sensitivity patients with myopia associated with amblyopia. Table 1 presents color perception data for patients of both groups at baseline and after treatment.
Color thresholds tended to improve and decreased in both groups after treatment. However, improvements in red, yellow, blue and green thresholds in Group 2 were more substantial than those in Group 1, and the improvement in yellow threshold in Group 2 was statistically significant (p = 0.03), although improvements in yellow and green thresholds in Group 1 were not statistically significant (Table 1). Conclusion
Our pleoptic and orthoptic treatment substantially improved visual acuity and improved stereovision both in patients with congenital myopia alone and in those with congenital myopia complicated by amblyopia. The two groups, however, demonstrated different changes in contrast sensitivity and color perception, which confirmed the fact that amblyopia is first of all related to an impairment in contrast sensitivity. The findings indicate that administration of any concomitant therapy for myopia should depend on the presence of amblyopia, and warrant further research on this subject. References
|