J.ophthalmol.(Ukraine).2019;2:44-49.
|
http://doi.org/10.31288/oftalmolzh201924449 Received: 20 March 2019; Published-online: 24 April 2019 Study of etiologic factors for optic atrophy V.A. Vasyuta,1 Dr Sc (Med); Yu.E. Pedachenko,2 Dr Sc (Med), Ass Prof 1 Romodanov Neurosurgery Institute, National Academy of Medical Science of Ukraine; Kyiv (Ukraine) 2 Shupik National Medical Academy of Postgraduate Education; Kyiv (Ukraine) E-mail: Vasyuta.v@ukr.net TO CITE THIS ARTICLE: Vasyuta VA, Pedachenko YuE. Study of etiologic factors for optic atrophy. J.ophthalmol.(Ukraine).2019;2:44-9. http://doi.org/10.31288/oftalmolzh201924449 Background: Optic atrophy (OA) is a disease of multiple etiologies and is a consequence of various pathological changes along the optic pathway. Central nervous system (CNS) disorders, vascular impairments and retinal and optic nerve diseases are important in the etiology of this condition. Purpose: To investigate various etiologic factors for OA. Materials and Methods: Patients were retrospectively divided into three groups: Group 1 (primary descending OA; 2,046 patients); Group 2 (primary ascending OA; 430 patients); and Group 3 (secondary OA; 190 patients). Results: Supratentorial tumors prevailed (78.0-79.4%) among the neurosurgical disease causing optic atrophy. Vascular factor was the most common cause (27.6-28.5%) of ascending OA, followed by inflammatory (25.5-30.1%). We found the presence of essential hypertension, diabetes mellitus type 2, and atherosclerosis to be significant medical risk factors for OA, with odds ratios of 2.46 (95% CI = 1.69 to 3.58), 2.32 (95% CI = 1.22 to 4.41), and 2.11 (95% CI = 1.41 to 3.15), respectively. Keywords: optic nerve, atrophy, etiology
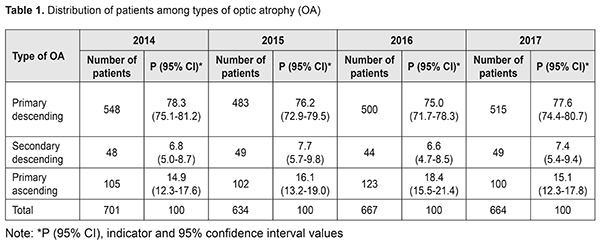
Introduction Optic atrophy (OA) holds a special place among eye disorders due to its severity and frequently leads to substantial loss of vision. OA (with the ICD-10 code of Н47.2) is an optic nerve disorder with a stable loss of visual function due to organic destruction of retinal ganglion cell axons and their myelin sheath, which results in blocking the conduction of nerve impulses. Optic atrophies show histologic changes such as nerve filber destruction, retinal ganglion cell degeneration, demyelination and vascular obliteration [1-3]. In addition, OA is a disease of multiple etiologies and is a consequence of various pathological changes along the optic pathway. Atrophic changes may result from degeneration, edema, impaired circulation, and compression of or traumatic damage to the optic nerve and its supplying vessels. A wide variety of etiologic factors may cause the disease, with the largest group of factors related to central nervous system (CNS) pathology. Brain neoplasms such as tumors in cerebral hemispheres, chiasmal and sellar region, posterior fossa, and cerebellum may have a pathologic influence on the optic pathway even in early stages of development. In direct optic nerve compression (most commonly, at the chiasm), compression of nerve fibers and primary descending OA develop. In tumors in cerebral hemispheres and/or hydrocephalus, the intracranial pressure rises, and papilledema develops, with subsequent transformation to secondary optic nerve atrophy. OA may also develop in subarachnoid hemorrhage, cerebral aneurysm, severe craniocerebral injury, and inflammation of the brain or its tunics. Demyelinating disorders (multiple sclerosis, multiple encephalomyelitis, and Devic's disease) cause retrobulbar optic nerve sheath inflammation which may also lead to OA. Ascending OA develops in acute and chronic vascular impairments, optic nerve inflammation, and central and peripheral retinal degeneration. Identification of the etiology of OA is important in the clinical practice to select the pathogenetic treatment, since management strategy for patients with OA varies depending on the presence of brain neoplasms, demyelination process, intoxication or vascular ocular disorders [4-8]. Systemic diseases (essential hypertension, atherosclerosis, diabetes mellitus, temporal arteritis, obliterative endarteritis, vertebrobasilar impairments in discopathy of the cervical spine, etc.) also play an important role in the development and progression of OA. In such cases, hemodynamics abnormalities, neuronal hypoxia, microcirculatory and metabolic abnormalities substantially aggravate the course of OA [4]. The purpose of the study was to investigate various etiologic factors for OA and prognostic significance of individual risk factors for OA. Materials and Methods Medical records of patients attending ophthalmologists of Neuroophthalmology Department of the Romodanov Neurosurgery Institute during 2014 to 2017 were subjected to analysis in order to investigate etiologic factors for OA. Given that OA is a consequence of various ocular and CNS disorders, patients were retrospectively divided into three groups: Group 1 (primary descending OA; 2,046 patients); Group 2 (primary ascending OA; 430 patients); and Group 3 (secondary OA; 190 patients). 95% confidence intervals (CI) reflecting the expected range for counts related to individual OA types were used to determine assessment accuracy. To investigate risk factors for OA, we used a case-control study (with comparison between groups with and without OA for prevalence of individual factors) and relative risk assessment. Medical records of 160 patients with OA and 400 patients without OA but with any other eye pathology who were consulted at the Neuroophthalmology Department were retrospectively examined. The assessment of results was based on odds ratios (OR) and 95% CI due to retrospective analysis of risk factors. Results Most (75.0%-78.3%) study cohort patients demonstrated descending OA associated with neurosurgical and/or neurological disorders during 2014 to 2017. This can be explained both by the prevalence of the pathology and by the specialty of the medical facility. The percentage of patients demonstrating ascending OA (due to eye pathology) varied from 14.9% in 2014 to 18.4% in 2017. Secondary OA was found in 6.6%-7.7% of study cohort patients. They had a history of papilledema of various etiologies (neoplasms, trauma, or benign intracranial hypertension) (Table 1). Here it is neurosurgical pathology in the context of which we consider secondary OA (i.e., due to raised intracranial pressure caused by tumors or other factors). Secondary OA, if present, is an unfavorable sign for visual prognosis and sometimes even for survival, and evidences late diagnosis of underlying disease. Visual functions are commonly substantially impaired and cannot be restored in such patients. In the presence of cerebral tumors, the goal of the ophthalmologist is early diagnosis of fundus signs of intracranial hypertension for prevention of secondary optic atrophy.
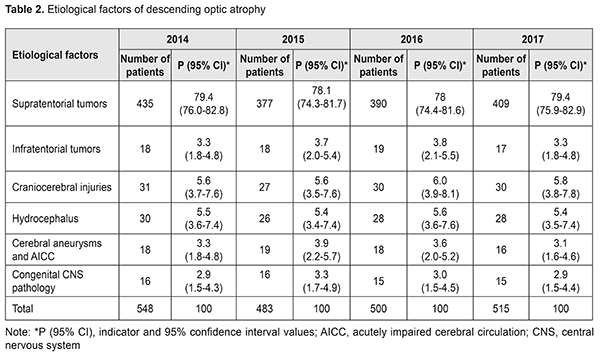
We conducted in-depth analysis of the causes of descending OA in study patients for the period of 2014 to 2017. The vast majority (up to 82.7%) of cases of descending OA were associated with brain neoplasms (Table 2). It should be noted that brain neoplasms were classified by location into infratentorial and supratentorial. Supratentorial tumors were found to be the most common cause of descending OA. Most commonly, these were pituitary adenomas, craniopharyngiomas and tuberculum sella meningiomas. This can be explained by close proximity of these neoplasms to the chiasm, optic nerves and optic tracts. The tumor may compress the optic nerve directly at the sella turcica and result in chiasmal syndrome and subsequent OA. Of the tumors that caused OA in study cases, 90.0% to 96% were supratentorial. Thus, of the 483 cases of descending OA registered in 2014, 435 (90.0±1.3%) were caused by supratentorial tumors. In addition, of the 426 cases of descending OA registered in 2017, 409 (96.0±0.0%) were caused by supratentorial tumors. Therefore, percentage of descending OA caused by supratentorial tumors statistically significantly increased with time, which requires attention.
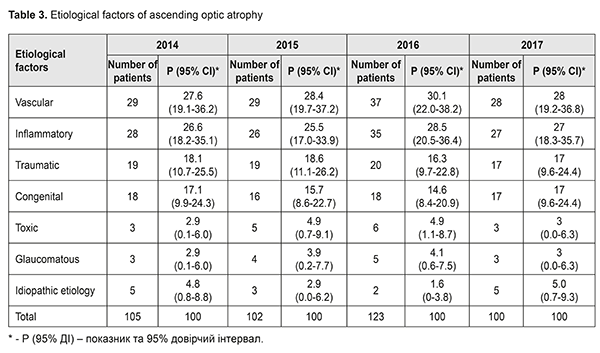
On the other hand, percentage of descending OA caused by infratentorial tumors was found to decrease from 10.0±1.3% in 2014 to 4.0±0.9% in 2017. The pathology is manifested as sequelae of the remote pathological process. Compression of the optic nerves and tracts take place due to expansion of the ventricular system or dislocation of brain structures. The identified features can be explained by the fact that, the diagnosis, especially, early diagnosis of raised intracranial pressure has become simpler and more accurate in recent years. In addition, descending OA is accompanied by the prominent general symptoms (headache and neurological impairments). Craniocerebral injury (≤6.0%) and hydrocephalus (≤5.6%) were the second and third most common causes of descending OA, with no significant difference between them or between years of assessment. The same can be said with regard to the least common causes, cerebral aneurysm and acutely impaired cerebral circulation (≤4.0%) and congenital CNS pathology (≤3.0%). Etiologic factors of ascending OA were subjected to analysis (Table 3). The number of patients with ascending OA (430) was substantially less than that of patients with descending OA. The former patients were referred to the institute for exclusion of neurosurgical pathology and differential diagnosis. In these patients, vascular factor (a consequence of acutely or chronically impaired optic nerve circulation, retinal vein or arterial occlusion) was the most common (27.6%-30.1%) etiologic factor, followed by optic nerve inflammation (papillitis or neuritis; 25.5%-28.5%). Retrobulbar neuritis is closely associated with demyelinating disorders of the nervous system. That is, more than half (54% to 58.6%) of cases with OA were attributed to the two above causes. In addition, traumatic (16.3-18.6%) and congenital (14.6-17.1%) factors were the third and fourth most common etiological factors in patients with ascending OA. Toxic (2.9%-4.9%) and glaucomatous (2.9%-4.1%) factors were practically equally common in ascending OA; each of them accounted for a share of 3.0% in 2017.
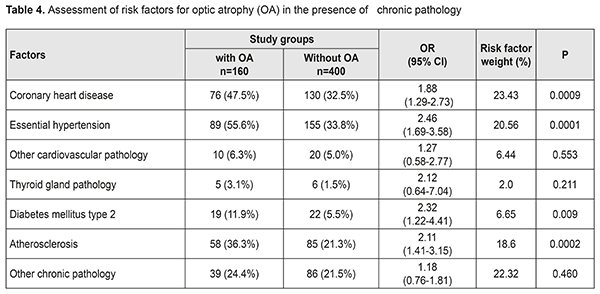
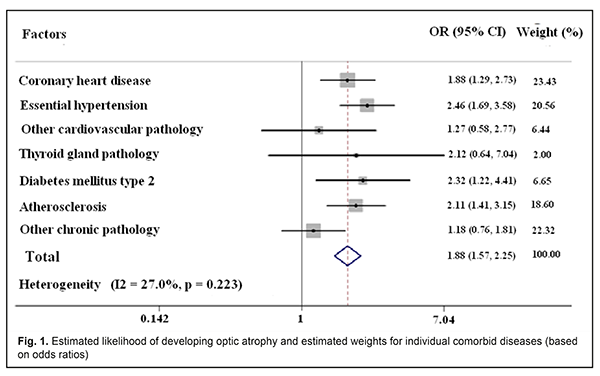
What draws attention is a rather high percentage of cases with idiopatic etiology of ascending OA (5% in 2014 and a 4.1% higher percentage in 2017). This trend indicates that there are still some problems with the diagnosis, and emphasizes the relevance of the issue. The pattern of distribution among the three groups (primary descending OA, secondary descending OA, and ascending OA) practically did not change during the period for assessment. This was confirmed also by the structural change coefficient (1.13%) for etiological factors of optic atrophy. A comprehensive approach is relevant to the study of OA because the latter is a disease of multiple etiologies, and various factors can influence the development and course of the disease. We conducted a study of the risk factors for OA. Our population-based cohort study involved both a case-control (the group with OA versus the group without OA) comparison for prevalence of individual factors and relative risk assessment. We found that a comorbid disease plays a statistically significant role in the formation of OA. Specifically, coronary heart disease, essential hypertension, diabetes mellitus type 2, and atherosclerosis were found significantly more frequently in patients with than in those without OA (47.5% vs 32.5%, 55.6% vs 33.8, 11.9% vs 5.5, and 36.3% vs 21.3, respectively, р=0.0002). The obtained data made us determine odds ratios (ORs) for the likelihood of developing OA in the presence of a given comorbid disease. The ORs for developing OA were 1.88 (95% CI = 1.29 to 2.73) for the presence of coronary heart disease, 2.46 (95% CI = 1.69 to 3.58) for the presence of essential hypertension, 2.32 (95% CI = 1.22 to 4.41) for the presence of diabetes mellitus type 2, and 2.11 (95% CI = 1.41 to 3.15) for the presence of atherosclerosis. Patients with comorbid thyroid gland disorders or chronic pathology tended to have an increased risk of developing OA, although the difference was not significant (Table 4).
Coronary heart disease, essential hypertension, and atherosclerosis were found to be the most substantial among comorbid disorders with regard to contribution to the risk of developing OA (23.43%, 20.56%, and 18.6%; Fig. 1).
Although the degree of prognostic significance varied among individual examined factors of comorbid pathology, we found no statistically significant difference based on the heterogeneity analysis, with heterogeneity coefficient (І2 = 27.0%, р = 0.223). This allows using these factors in further research and clinical practice to improve the diagnosis and management of atrophy in these patients. Conclusion Etiological factors for OA in various groups of patients were subjected to analysis. Supratentorial tumors prevailed (78.0-79.4%) among the neurosurgical disease causing optic atrophy. Vascular factor was the most common cause (27.6-28.5%) of ascending OA, followed by inflammatory (25.5-30.1%). The value of structural change coefficient for etiological factors of optic atrophy over the period of assessment was 1.13%, evidencing insignificant changes in the structure of causes of OA, and thus allowing for extrapolation of the analysis results to the general population and other time periods. We found the presence of essential hypertension, diabetes mellitus type 2, and atherosclerosis to be significant medical risk factors for OA, with odds ratios of 2.46 (95% CI = 1.69 to 3.58), 2.32 (95% CI = 1.22 to 4.41), and 2.11 (95% CI = 1.41 to 3.15), respectively. References 1.Gustov AV, Sigrianskii KI, Stoliarova GhP. [Practical neuroophthalmology in 2 volumes]. N. Novgorod: N. Novgorodskaya gosudarstvennaya medicinskaya academia; 2000. 2.Morosov VI, Yakovlev AA. [Diseases of the visual pathway: Clinical picture, diagnosis and treatment]. Moscow: Binom; 2010. 3.Nikoforov AS, Guseva MR. [Ophthalmoneurology]. Moscow: GEOTAR-Media; 2014. 4.Vitovska OP, Vasyuta VA, Konah VM. [Optic nerve atrophy: main problems and ways of prevention]. Kiev: Tri K; 2016. 5.Chinta S, Wallang BS, Sachdeva V, et al. Etiology and clinical profile of childhood optic nerve atrophy at a tertiary eye care center in South India. Indian J Ophthalmol. 2014; 62(10): 1003-7. doi: 10.4103/0301-4738.145996. 6.Mbekeani JN, Fattah MA, Poulsen DM, et al. Etiology of optic atrophy: a prospective observational study from Saudi Arabia. Ann Saudi Med. 2017 May-Jun;37(3): 232-9. doi: 10.5144/0256-4947.2017.232. 2017 May-Jun;37(3):232-239. 7.Roodhooft JM. Nonglaucomatous optic disk atrophy and excavation in the elderly. Bull Soc Belge Ophtalmol. 2003;(287): 45-9. 8.Tagoe NN, Essuman VA, Fordjuor G, et al. Neuro-Ophthalmic and Clinical Characteristics of Brain Tumours in a Tertiary Hospital in Ghana. Ghana Med J. 2015 Sep;49(3):181-6.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|