J.ophthalmol.(Ukraine).2019;6:3-6.
|
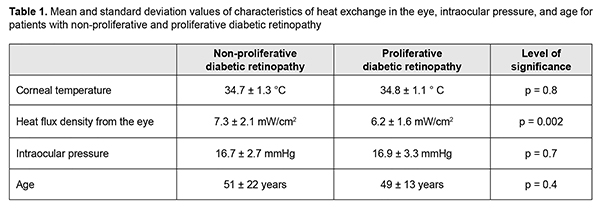
http://doi.org/10.31288/oftalmolzh2019638 Received: 15 October 2019; Published on-line: 31 December 2019 Temperature of and heat flux density from the external ocular surface in diabetic retinopathy patients: a pilot study L.I. Anatychuk,1,2 Member of the NAS of Ukraine, Dr Sc (Phys and Math), Prof.; N.V. Pasyechnikova,3 Associate Member of the NAS of Ukraine Dr Sc (Med), Prof.; V.A. Naumenko,3 Dr Sc (Med), Prof.; O.S. Zadorozhnyy,3 Cand Sc (Med); N.I. Khramenko,3 Cand Sc (Med); R.E. Nazaretian3; R.R. Kobylianskyi,1,2 Cand Sc (Phys and Math) 1 Institute of Thermoelectricity, National Academy of Science and Ministry of Education and Science, Ukraine; Chernivtsi (Ukraine) 2 Yuriy Fedkovych Chernivtsi National University; Chernivtsi (Ukraine) 3 SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the National Academy of Medical Sciences of Ukraine"; Odesa (Ukraine) E-mail: zadoroleg2@gmail.com Background: Heat exchange characteristics include not only temperatures and temperature distribution, but also heat flux (HF). Purpose: To examine temperature of and density of HF from the ocular surface in the eyes of patients with diabetic retinopathy (DR). Material and Methods: Sixty-two patients (123 eyes) with DR were under observation. Of these, 28 (55 eyes) and 34 (68 eyes) were diagnosed with non-proliferative DR (NPDR) and proliferative DR (PDR), respectively. They underwent a general clinical examination and measurements of temperature of the external corneal surface and density of HF from the eye. In addition, all NPDR patients underwent rheoophthalmography (ROG). Results: There was a significant difference in density of HF from the ocular surface (7.3 ± 2.1 mW/cm2 vs 6.3 ± 1.6 mW/cm2; p = 0.002), but not in ocular surface temperature (34.7 ± 1.3 °С vs 34.8 ± 1.1 °С; p = 0.8) between NPDR patients and PDR patients. HF density from the eye was positively correlated with the ocular blood volume coefficient (RQ; also named the rheographic coefficient) as assessed by ROG (r = 0.5; p = 0.01) for patients with NPDR. There was a relationship between the density of heat flux from the ocular surface and age of DR patients. Conclusion: Preliminary results suggest that (1) compared to the temperature of the ocular surface, the heat flux from the ocular surface better reflects the status of heat exchange in the eye, and (2) the technique might be promising as a diagnostic test for various pathological conditions involving impaired heat processes in the eye. Keywords: thermoelectric device, temperature of the external ocular surface, heat flux density, rheoophthalmography, diabetic retinopathy Introduction Special attention is paid at this time to studies on the heat processes that take place continuously in the human body and are essential for its normal vital activities under various conditions. The literature has reported on the features of daily variations in body temperature [1,2], effect of physical activity on changes in body temperature [3], and changes in the patient’s body temperature during surgery [4]. Relationships have been reported between the temperature of the external ocular surface and the status of blood circulation in the eye, intraocular pressure, and presence of intraocular inflammation or tumors [4-9]. The features of heat processes in a diabetic mellitus patient, including intraocular processes, are still poorly understood [10]. Heat exchange characteristics include not only temperatures and temperature distribution, but also heat flux (HF), which is a major heat exchange index and reflects the function of organs and tissues more completely than the two former characteristics [11]. We have previously reported initial results of heat flux measurements in the eyes of a group of healthy individuals with the use of our in-house thermoelectric device [12], and noted an age-related difference in these eyes. In addition, we have hypothesized that age-related atrophic choroidal changes and associated decreased volume of blood in the uveal tract could be a cause of a decrease in heat flux density from the eye with age in healthy individuals. The purpose of the study was to examine temperature of and heat flux density from the ocular surface in the eyes of patients with diabetic retinopathy (DR). Material and Methods This open pilot study followed the ethical standards stated in the Declaration of Helsinki and was approved by the Local Ethics Committee of the Filatov Institute. Written informed consent was obtained from all individuals enrolled in the study. Sixty-two patients (123 eyes; age, 16 to 86 years) with DR were under observation. Of these, 28 (55 eyes) and 34 (68 eyes) were diagnosed with non-proliferative DR (NPDR) and proliferative DR (PDR), respectively. In each patient, the stage of DR was the same in both eyes. Patients with neovascular glaucoma or with a history of intravitreal antiangiogenic therapy or vitrectomy were excluded from the study. Patients underwent a general clinical examination and measurements of temperature of the external corneal surface and heat flux density from the eye. The thermoelectric device developed within the framework of the partnership agreement between the Institute of Thermoelectricity of the NAS of Ukraine and MES of Ukraine and the Filatov Institute of the NAS of Ukraine was used for measurements of temperature of the external ocular surface and heat flux density from the eye [12]. Studies were performed within the specified time period of the day (3:00 PM to 4:00 PM) under stable environmental conditions (air temperature and humidity control and minimal indoor air velocity). During the study period, the mean temperature in the room was 23.0±1.9 °С. Before evaluation, patients spent 15 minutes indoors for adaptation to the room environment. No mydriatic was used. Patients were administered epibulbar anesthesia with ophthalmic 0.5% proparacaine hydrochloride (ALCAINE®, SA Alcon-Couvreur NV, Puurs, Belgium). Temperatures and heat flux density were recorded 15 minutes after instilling a drop of the anesthetic. During data acquisition, patients were positioned before a slit-lamp apparatus. The prism-transducer assembly was attached to the conventional prism mount of the Goldmann tonometer, and the thermoelectric heat-flux transducer came into direct contact with the subject’s central cornea in all cases. In addition, all patients with NPDR underwent rheoophthalmography. The rheographic coefficient (RQ; also named the ocular blood volume coefficient), an index characterizing the volume of blood entering the eye per unit time, was calculated based on rheoophthalmographic studies. Group data were tested for normality. The level of significance p ? 0.05 was assumed. Quantitative data are presented as mean and standard deviation (SD). Pearson's correlation analysis was used to determine if there was an association between the two methods. Statistical analyses were conducted using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software [13]. Results Table 1 presents mean ocular surface temperature, the density of heat flux from the ocular surface, IOP, and age of patients with NPDR and PDR.
There was no significant difference in heat flux density between PDR eyes that did and did not undergo retinal laser photocoagulation (p = 0.6). Heat flux density from the eye was positively correlated with the ocular blood volume coefficient (RQ) (? = 0.5; p = 0.01) for patients with NPDR. A weaker correlation was found between the corneal temperature and the RQ (? = 0.3; p = 0.15). Thus, mean heat flux density from the eye was 5.3 ± 2.6 mW/cm2 for patients with RQ ? 2.0 ‰, and 7.2 ± 2.3 mW/cm2 for those with RQ > 2.0 ‰ (p = 0.03). In addition, mean corneal temperature was 34.3 ± 1.0 °С for patients with RQ ? 2.0 ‰, and 35.1 ± 1.3 °С for those with RQ > 2.0 ‰ (p = 0.1). At the next stage of the study, we assessed a relationship between the density of heat flux from the ocular surface and age. For this purpose, patients were divided into three age groups: 16-30 years (group 1; 12 patients; 24 eyes), 31-60 years (group 2; 31 patients; 62 eyes), and 61-86 years (group 3; 19 patients; 37 eyes). In these groups, mean density of heat flux from the ocular surface was 8.1 ± 1.8 mW/cm2, 6.4 ± 1.9 mW/cm2 (p < 0.001), and 6.1 ± 1.8 mW/cm2 (p < 0.001 and p =0.3 for comparisons with group 1 and group 2, respectively), respectively. No corneal trauma or other complications were observed in any participant during the examination. Discussion We found that PDR patients had lower mean density of heat flux from the ocular surface compared to NPDR patients, which may be the result of a more severe impairment of hemodynamics in PDR. These findings are in agreement with reports in the literature that eyes with PDR have thinner choroids, compared with eyes with NPDR [14]. In addition, we found no significant difference in temperature of the external ocular surface between patients differing in the stage of DR. Moreover, we found a positive correlation between the heat flux density and the rheographic coefficient obtained from ophtalmorheographic examination, which supports the hypothesis that low blood volume in the uveal tract is a cause of a decrease in heat flux density from the eye with age in healthy individuals [12]. Of note was also a mild correlation of the temperature of the external corneal surface and the ocular blood volume coefficient. Furthermore, there was a difference in density of heat flux from the ocular surface between DR patients of different age groups, which is in agreement with our previous findings from healthy individuals, and may be explained by age-related atrophic choroidal changes and associated decreased blood volume in the uveal tract [12,15]. Therefore, compared to the temperature of the external corneal surface, the heat flux from the ocular surface seems to be a more informative index of heat exchange, providing valuable additional information about the status of circulation in the uveal tract. A limitation of this study is that the study cohort included patients who had undergone treatment for DR, particularly, retinal laser photocoagulation. However, we found no significant difference in heat flux density between PDR eyes that did and did not undergo retinal laser photocoagulation (p = 0.6). Further studies targeted at investigating the potential of the ophthalmic heat flux density measurement technique are warranted to assess its value in the diagnosis of various eye disorders. Conclusion First, there was a significant difference in density of heat flux from the ocular surface (7.3 ± 2.1 mW/cm2 vs 6.3 ± 1.6 mW/cm2; p = 0.002), but not in external ocular surface temperature (34.7 ± 1.3 °С vs 34.8 ± 1.1 °С; p = 0.8) between NPDR patients and PDR patients. Second, there was a stronger correlation of the rheographic coefficient obtained from ophtalmorheographic examination, with the density of heat flux from the ocular surface (? = 0.5; p = 0.1), than with the corneal temperature (? = 0.3; p = 0.15) for NPDR patients. Mean heat flux density from the eye was 5.3 ± 2.6 mW/cm2 for patients with RQ ? 2.0 ‰, and 7.2 ± 2.3 mW/cm2 for those with RQ > 2.0 ‰ (p = 0.03). Third, there was a relationship between the density of heat flux from the ocular surface and age of DR patients, with mean values of 8.1 ± 1.8 mW/cm2, 6.4 ± 1.9 mW/cm2, and 6.1 ± 1.8 mW/cm2, for the groups of 16-30 years, 31-60 years, and 61-86 years, respectively. Finally, our preliminary results suggest that (1) compared to the temperature of the external corneal surface, the heat flux from the ocular surface better reflects the status of heat exchange in the eye, and (2) the technique might be promising as a diagnostic test for various pathological conditions involving impaired heat processes in the eye. Acknowledgment The authors thank Prof. A.S. Buiko for his methodological help.
References 1.Burfield HJ, Carkeet A, Ostrin LA. Ocular and Systemic Diurnal Rhythms in Emmetropic and Myopic Adults. Invest Ophthalmol Vis Sci. 2019 May 1;60(6):2237-2247. 2.S?omko J, Zalewski P. The circadian rhythm of core body temperature (Part I): The use of modern telemetry systems to monitor core body temperature variability. Pol Hyperb Res. 2016;55:79-83. 3.Kazama A, Takatsu S, Hasegawa H. Effect of increase in body temperature on cognitive function during prolonged exercise. Jpn J Phys Fitness Sports Med. 2012;61(5):459-67. 4.Boisson M, Alaux A, Kerforne T, Mimoz O, Debaene B, Dahyot-Fizelier C, Frasca D. Intra-operative cutaneous temperature monitoring with zero-heat-flux technique (3M SpotOn) in comparison with oesophageal and arterial temperature: A prospective observational study. Eur J Anaesthesiol. 2018 Nov;35(11):825-830. 5.Tan J-H, Ng EYK, Acharya UR, Chee C. Infrared thermography on ocular surface temperature: A review. Infrared Phys Techn. 2009;52:97-108. 6.Zadorozhnyy OS, Guzun OV, Bratishko AIu, Kustrin TB, Nasinnik IO, Korol AR. Infrared thermography of external ocular surface in patients with absolute glaucoma in transscleral cyclophotocoagulation: a pilot study. J ophthalmol (Ukraine). 2018;2:23-28. 7.Bu?ko AS, Tsykalo AL, Terent'eva LS, Niankina EE. [Thermography based on liquid crystals in ophthalmologic oncology]. Oftalmol Zh. 1977;32(2):110-4. Russian. 8.Galassi F, Giambene B, Corvi A, Falaschi G. Evaluation of ocular surface temperature and retrobulbar haemodynamics by infrared thermography and colour Doppler imaging in patients with glaucoma. Br J Ophthalmol. 2007;91:878-81. 9.Sodi A, Giambene B, Falaschi G, et al. Ocular surface temperature in central retinal vein occlusion: preliminary data. Eur J Ophthalmol. 2007 Sep-Oct;17(5):755-9. 10.Kenny GP, Sigal RJ, McGinn R. Body temperature regulation in diabetes. Temperature. 2016 Jan 4;3(1):119-45. 11.Grischenko TG, Dekusha LV, Vorobiov L.Y. [Heat flow measuring: theory, metrology, practice]. Book 1. [Methods and means of heat flow measuring]. Kyiv: Institute of Engineering Thermophysics of NASU; 2017. Russian. 12.Anatychuk LI, Pasyechnikova NV, Naumenko VА, Zadorozhnyy OS, Gavrilyuk MV, Kobylianskyi RR. A thermoelectric device for ophthalmic heat flux density measurements: results of piloting in healthy individuals. J ophthalmol (Ukraine). 2019;3:45-51. 13.Yankovoy A.G. [Multivariate analysis in the STATISTICA system]. Odesa: Optimum; 2001. 216 p. Russian. 14.Sudhalkar A, Venkata A, Raman R, Rao PS, Jonnadula GB. Choroidal thickness in diabetic patients of Indian ethnicity. Indian J Ophthalmol. 2015 Dec;63(12):912-6.
None of the authors has any conflicting interests to disclose
|