J.ophthalmol.(Ukraine).2020;5:56-61.
|
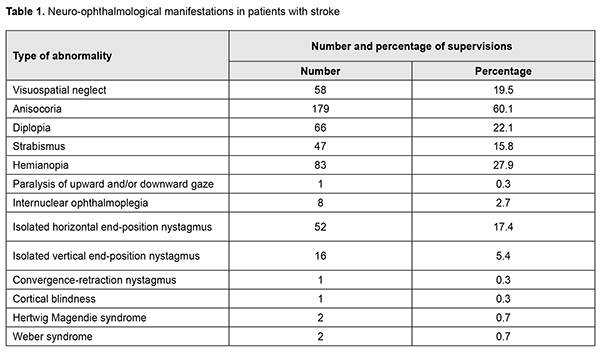
http://doi.org/10.31288/oftalmolzh202055661 Received: 24 June 2020; Published on-line: 27 October 2020 Neuro-ophthalmological abnormalities in patients with ischemic stroke in the setting of a stroke center of a university clinic T. M. Muratova, L. V. Venger, D. M. Khramtsov, Iu. M. Vorokhta, V. D. Teliushchenko Odesa National Medical University; Odesa (Ukraine) E-mail: yuri.vorokhta@gmail.com TO CITE THIS ARTICLE: Muratova TM, Venger LV, Khramtsov DM, Vorokhta IuM, Teliushchenko VD. Neuro-ophthalmological abnormalities in patients with ischemic stroke in the setting of a stroke center of a university clinic. J.ophthalmol.(Ukraine).2020;5:56-61. http://doi.org/10.31288/oftalmolzh202055661 Background: Stroke remains one of the leading causes of death and disability in the world. Most patients with stroke exhibit neuro-ophthalmological abnormalities. Purpose: To assess the frequency of neuro-ophthalmological abnormalities in patients with stroke in the setting of a stroke center of a university clinic. Material and Methods: Two hundred and ninety-eight patients with acute ischemic cerebrovascular accidents who were under observation at the stroke service of the Neurology Department of the Center for Reconstructive and Restorative Medicine (University Clinic) of the Odesa National Medical University from January 2016 through December 2019 were included in the study. Frequency of neuro-ophthalmological symptoms was assessed at the first neurological examination visit and after ophthalmologist consultation was obtained. Results: Of the 298 patients with stroke, most (162; 54%) were men. Mean patient age was 60.4 ± 1.1 years and mean National Institutes of Health Stroke Scale (NIHSS) score was 10.1 ± 0.9. In addition, of the 298 patients, 163 (54.7%) were admitted to the clinic within a day after onset of clinical symptoms of a stroke. Stroke syndromes were categorized into four subtypes, total anterior circulation infarcts (TACI), partial anterior circulation infarcts (PACI), lacunar circulation infarcts (LACI), and posterior circulation infarcts (POCI). PACI were the most common (139 cases or 36.6%), followed by LACI (88 cases or 29.5%), whereas TACI were least common (28 cases or 10.5%). Of special interest were POSI (43 cases or 14.4%). Fourteen patients with POSI (4.7% of the total study patients) had lesions of the midbrain and pons. Neuro-ophthalmological manifestations were found in 88.8% of patients. Of these manifestations, anisocoria was the most common (60.1%), followed by hemianopia (27.9%), diplopia (22.1%) and visuospatial neglect (19.5%), and various oculomotor abnormalities. Internuclear ophthalmoplegia (INO) was found only in 8 cases (2.7%). Conclusion: Diagnosing neuro-ophthalmological syndromes requires coordinated efforts of the neurologist and ophthalmologist in the setting of a multi-professional team. Keywords: neuroophthalmology, stroke, diagnosis
Introduction Stroke remains one of the leading causes of death and disability in the world, and projections show that with a ‘business as usual’ approach, the burden of stroke will not decrease in the next decade or beyond [1, 2]. An important contributing factor to this is that the number of older persons in Europe is rising, with a projected increase of 35% between 2017 and 2050 [2]. Action Plan for Stroke in Europe 2018-2030 identifies one of the four overreaching targets for 2030 as “to treat 90% or more of all patients with stroke in Europe in a dedicated stroke unit as the first level of care”. In addition, this plan defines stroke unit as a dedicated geographically clearly defined area or ward in a hospital, where stroke patients are admitted and cared for by a multi-professional team (medical, nursing and therapy staff) who have specialist knowledge of cerebral function, training and skills in stroke care with well-defined individual tasks, regular interaction with other disciplines and stroke leadership [2-4]. This team coordinates care through regular, multidisciplinary meetings. Moreover, the plan defines stroke center as a hospital infrastructure and related processes of care that provide the full pathway of stroke unit care [2]. A stroke center is the coordinating body of the entire chain of care. This covers pre-hospital care, ongoing rehabilitation and secondary prevention and access to neurosurgical and vascular intervention [2, 3]. A stroke unit is the most important component of a stroke center [2, 5]. The Stroke Center provides stroke unit services for the population of its own catchment area and serves as a referral center for peripheral hospitals with stroke units in case their patients need services which are not available locally [2, 3,5]. Neuro-ophthalmological abnormalities have been reported in as much as 90% of patients with stroke [6, 7]. Particularly, retinal hemorrhage; Terson’s syndrome; amaurosis fugax; Prevost's sign; diplopia and strabismus; Hertwig Magendie syndrome; other oculomotor disorders; cortical blindness; unilateral or bilateral hemianopia, sometimes with sparing of central tubular vision; and palinopsia have been reported to occur in patients with stroke [6-9]. Unfortunately, an eye examination is sometimes postponed even in the setting of a functioning and adequate multi-professional team, which increases the risk of misdiagnosis [10]. The purpose of the study was to assess the frequency of neuro-ophthalmological abnormalities in patients with stroke in the setting of a stroke center of a university clinic. Material and Methods Two hundred and ninety-eight patients with acute ischemic cerebrovascular accidents who were under observation at the stroke service of the Neurology Department of the Center for Reconstructive and Restorative Medicine (University Clinic) of the Odesa National Medical University from January 2016 through December 2019 were included in the study. Patients received observation and treatment as per Decree No.602 of August 3, 2012, “On Approval and Introduction of Medical and Technological Documents for Standardization of Care in Ischemic Stroke” and the 2018 and 2019 AHA/ASA Guidelines for the Early Management of Acute Ischemic Stroke [11-13]. This study conformed to the principles of the Helsinki declaration and laws of Ukraine. Frequency of neuro-ophthalmological symptoms was assessed at the first neurological examination visit and after ophthalmologist consultation was obtained (on Day 1 of hospitalization for those admitted on weekdays and Day 2 or 3 for those admitted over a weekend or on public holidays). Computer tomography (CT) of the brain was performed at admittance to the inpatient setting. Magnetic resonance imaging (MRI) or another CRT of the brain was performed, if indicated [14]. Stroke syndromes were categorized into four subtypes, total anterior circulation infarcts (TACI), partial anterior circulation infarcts (PACI), lacunar circulation infarcts (LACI), and posterior circulation infarcts (POCI), as per the Oxfordshire Community Stroke Project Classification (OCSP) [15]. An eye examination included visual acuity, tonometry, perimetry, the status of binocular vision, ocular motility, angle of deviation, convergence, and fundus ophthalmoscopy [16]. Statistical analyses (specifically, analysis of variance) were conducted using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software [17]. Results Of the 298 patients, most (162; 54%) were men. Mean patient age was 60.4 ± 1.1 years and mean National Institutes of Health Stroke Scale (NIHSS) score was 10.1 ± 0.9. In addition, of the 298 patients, 163 (54.7%) were admitted to the clinic within a day after onset of clinical symptoms of a stroke. Of the stroke syndrome subtypes, PACI was the most common (139 cases or 36.6%), followed by LACI (88 cases or 29.5%), whereas TACI was least common (28 cases or 10.5%). Of special interest were cases with POSI (43 cases or 14.4%). Fourteen patients with POSI (4.7% of the total study patients) had lesions of the midbrain and pons. Neuro-ophthalmological manifestations were found in 88.8% of patients. Of these manifestations, anisocoria was the most common (60.1%), followed by hemianopia (27.9%), diplopia (22.1%) and visuospatial neglect (19.5%), and various oculomotor abnormalities (Table 1).
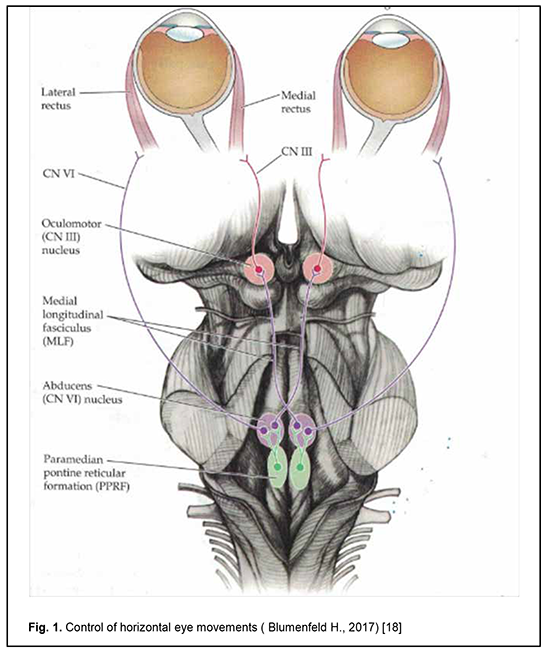
Internuclear ophthalmoplegia (INO) was found only in 8 cases (2.7%) (Table 1). The INO is characterized clinically by an ispilateral adduction deficit on attempted gaze to the contralateral side [8]. In addition, contralateral abduction and vertical saccades are preserved, but patients with INO present with dissociative nystagmus and diplopia. The clinical picture results from lesion of the medial longitudinal fasciculus (MLF) that extends from the nucleus of Darkshevich and the interstitial nucleus of Cajal at the level of the metathalamus, penetrates the brainstem at the midline, ventral to the central periaqueductal gray matter, and enters anterior spinal cord funiculi beneath the rhomboid fossa, where it terminates at neurons of the anterior spinal cord horns at the level of the neck [18]. The MLF is a fiber tract with fibers related to various systems. It has descending and ascending components that interconnect paired brainstem structures (Fig. 1), particularly, the nuclei of cranial nerves III, IV and VI that innervate the oculomotor muscles, the vestibular nuclei and cell structures of the reticular formation, and the anterior horns of the cervical spinal cord [18]. Normally, movements of eye globes are harmonius due to the associative function of the MLF. Damage to the MLF results in oculovestibular abnormalities; they depend on the location and extent of the focus of pathology [8, 9, 18].
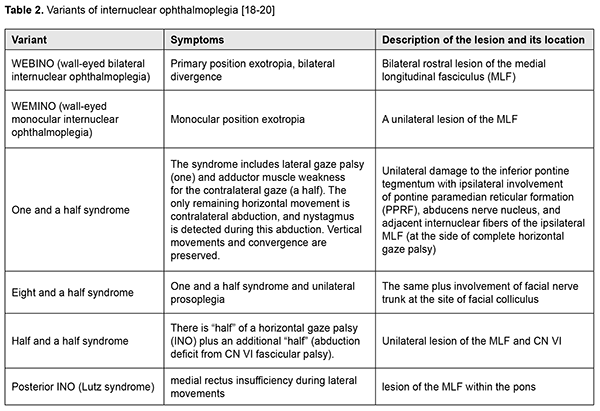
Unilateral internuclear ophthalmoplegia (INO) is the most common, while bilateral INO, wall-eyed bilateral INO (WEBINO) syndrome and “one and a half” syndrome are less common among the variants of INO in patients with stroke (Table 2) [8, 9, 19, 20].
When a superior MLF lesion is near the CN III nucleus, the eyes are divergent due to bilateral involvement of the medial recti and there is a loss of convergence mechanism. The WEBINO syndrome (wall-eyed bilateral INO) consists of bilateral INO with exotropia and loss of convergence, and indicates a midbrain lesion (specifically, a lesion of the MLF and the oculomotor nerve neurons innervating medial rectus muscle). The “one and a half” syndrome is characterized by a lesion of the paramedian pontine reticular formation or the abducens nucleus, with interruption of internuclear fibers of the ipsilateral MLF [18, 20]. The eye affected by the lesion cannot move horizontally to either side, and the only remaining horizontal movement is contralateral abduction; convergence is unaffected. A so-called posterior INO is uncommon in acute stroke [10, 16, 18]. It is the result of the lesion of the MLF within the pons. In addition, lateral eye movements are restricted due to medial rectus weakness, e.g., leftward gaze reveals a deficit of rightward adduction, but abduction is normal in either direction (although apparent atactic nystagmus can be seen in typical cases of posterior INO on the side of abduction). The involvement of mostly adductive movements is typical for this syndrome, irrespective of gaze direction, and minimum nystagmus can be seen on the side of adduction [16, 20]. One patient showed the signs of Parinaud syndrome that develops when there is a bilateral lesion of the rostral midbrain at the level of the superior colliculus. Paralysis of upward gaze and convergence, bilateral partial ptosis, pupillary light-near dissociation and convergence-retraction nystagmus are characteristic for this syndrome. Vertical eye movement center, the anterior part of the posterior longitudinal fasciculus, and the posterior cerebral commissure are involved in the pathological process. The syndrome can be caused by impaired posterior cerebral circulation [18]. Two patients showed signs of Weber syndrome with lesions of the nuclei and roots of the oculomotor nerve and the pyramidal tract [16, 18]. Ptosis, mydriasis, divergent strabismus, diplopia, impaired accommodation, and exophthalmos were seen on the affected side, whereas central hemiparesis, paresis of facial and lingual muscles and hemihypesthesia were seen on the contralateral side. Hertwig Magendie syndrome was diagnosed in two patients. The globe on the affected side rotated downwards and nasally, and the globe on the contralateral side rotated upwards and temporally. These dissociated positions of the eyes were preserved even with a change in gaze direction. The syndrome develops if the pathological focus is present in the rostral midbrain and other portions of the midbrain, and is caused by dysfunction of the posterior longitudinal fasciculus that coordinates conjugate eye movements [18]. Discussion Although many of the above described conditions are uncommon, these clinical syndromes reflect damage to functionally important structures of the midbrain, and are important for predicting recovery and assessing the patient’s potential for rehabilitation [10, 16, 21]. Diagnosing these disorders in the setting of a stroke unit or center requires close cooperation between the neurologist and ophthalmologist. This cooperation may be difficult to achieve if the patient is admitted at night or over a weekend, which makes an ophthalmologist consultation postponed by hours and even days. Rational assessment of oculomotor function is important in the differential diagnosis of neuro-ophthalmological manifestations of stroke (Table 2). The prognosis is favorable for most patients with post-ICA INO, but the recovery may be incomplete. Partial regression of clinical signs and symptoms commonly begins as early as 2-3 months after stroke. Patients with WEBINO or WEMINO sometimes require corrective surgery to address primary position exotropia. In the current study, 75.1% stroke patients with neurtoophthalmological manifestations showed partial regression of clinical symptoms 3 months after stroke. Therefore, neuro-ophthalmological manifestations were found in 88.8% of patients with stroke in the setting of a stroke center of a university clinic. Of these manifestations, anisocoria was the most common (60.1%), followed by hemianopia (27.9%), diplopia (22.1%) and visuospatial neglect (19.5%), and various oculomotor abnormalities. In addition, of the total stroke patients, 4.7% had lesions of the midbrain and pons with ophthalmoplegic manifestations. Our experience argues that diagnosing neuro-ophthalmological syndromes requires coordinated efforts of the neurologist and ophthalmologist in the setting of a multi-professional team.
References 1.Muratova T, Khramtsov D, Stoyanov A, Vorokhta Y. Clinical epidemiology of ischemic stroke: global trends and regional differences. Georgian Med News. 2020 Feb;(299):83-6. 2.Norrving B, Barrick J, Davalos A, Dichgans M, Cordonnier C, Guekht A, et al. Action Plan for Stroke in Europe 2018-2030. Eur Stroke J. 2018 Dec;3(4):309-36. 3.Dutta D, Hellier K, Obaid M, Deering A. Evaluation of a single centre stroke service reconfiguration - the impact of transition from a combined (acute and rehabilitation) stroke unit to a hyperacute model of stroke care. Future Healthc J. 2017 Jun;4(2):99-104 4.Rowe FJ; VIS Group. Accuracy of referrals for visual assessment in a stroke population. Eye (Lond). 2011 Feb;25(2):161-7. 5.Sacco RL. Stroke Vision 2020: Creating a Roadmap for the Next Decade. Stroke. 2020 Mar;51(3):1040-6. 6.Klyushnikov SA, Aziatska GA. [Oculomotor disorders in neurological practice]. Nervnyie bolezni. 2015; 4:41-6. Russian. 7.Rowe FJ, Conroy EJ, Barton PG, Bedson E, Cwiklinski E, Dodridge C, et al. A Randomised Controlled Trial of Treatment for Post-Stroke Homonymous Hemianopia: Screening and Recruitment. Neuroophthalmology. 2016 Jan 19;40(1):1-7. 8.Hanna KL, Rowe FJ. Health Inequalities Associated with Post-Stroke Visual Impairment in the United Kingdom and Ireland: A Systematic Review. Neuroophthalmology. 2017 Mar 1;41(3):117-136. 9.Walle KM, Nordvik JE, Becker F, Espeseth T, Sneve MH, Laeng B. Unilateral neglect post stroke: Eye movement frequencies indicate directional hypokinesia while fixation distributions suggest compensational mechanism. Brain Behav. 2019 Jan;9(1):e01170. 10.Gorbulina VS, Zatei AO. [Ways to improve neuroophthalmology]. Alleia nauki. 2018;3(7):54-7. Russian. 11.[Order of the Ministry of Health of Ukraine No. 602 issued on 3.08.2012 “On approval and implementation of medical and technological documents on standardization of medical care for ischemic stroke”, as amended and supplemented by Order No. 34 of the Ministry of Health of Ukraine of 15.09.2014]. Access mode: http://search.ligazakon.ua/l_doc2.nsf/link1/MOZ16323.html. Ukrainian. 12.Jadhav AP, Mokin M, Ortega-Gutierrez S, Haussen D, Liebeskind D, Nogueira R, et al. An Appraisal of the 2018 Guidelines for the Early Management of Patients with Acute Ischemic Stroke. Interv Neurol. 2020 Feb;8(1):55-9. 13.Warner JJ, Harrington RA, Sacco RL, Elkind MSV. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke. Stroke. 2019 Dec;50(12):3331-3332. 14.Markdorf SA, Predtechenskaya EV, Savelov AA, Tulupov AA, Shtark MB. [Neuroimaging and cerebral infarction (stroke)]. Uspekhi fiziologicheskikh nauk. 2018; 49(2): 60-71. Russian. 15.Elkind MS. Stroke Etiologic Classification-Moving From Prediction to Precision. JAMA Neurol. 2017 Apr 1;74(4):388-90. 16.Gustov AV, Takhtaev IuV, Sigrianskii KI, Murzin VA. [Practical neuroophthalmology: a guide for doctors]. Nizhnii Novgorod: Publishing House of Nizhnii Novgorod State Medical Academy; 2011. Russian. 17.Khalafian A.A. [Industrial statistics: Quality control, process analysis, experiment planning in the STATISTICA package]. Moscow: Librocom, 2013. Russian. 18.Blumenfeld H. Neuroanatomy through clinical cases. 2nd ed. Sunderland, MA: Sinauer Associates; 2010. 19.Vázquez-Justes D, Martín-Cucó A, Gallego-Sánchez Y, Vicente-Pascual M. WEBINO syndrome (wall-eyed bilateral internuclear ophthalmoplegia) secondary to ischemic stroke, about a case. Arch Soc Esp Oftalmol. 2020 Apr;95(4):205-208. 20.Vynckier J, Lemmens R. Torsional internuclear ophthalmoplegia in acute ischemic stroke. Neurol Clin Pract. 2019 Apr;9(2):168-9. 21.Hanna KL, Rowe FJ. Clinical versus Evidence-based Rehabilitation Options for Post-stroke Visual Impairment. Neuroophthalmology. 2017 Jul 6;41(6):297-305.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|