J.ophthalmol.(Ukraine).2020;5:79-85.
|
http://doi.org/10.31288/oftalmolzh202057985 Received: 15 June 2020; Published on-line: 27 October 2020
Strategies for the development of cyber-ophthalmology Y. Danyk1, O. Zborovska2, N. Pasyechnikova2 1 Institute of Information Technologies; Kyiv (Ukraine) 2 SI "Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine"; Odesa (Ukraine) E-mail: filatoveye@gmail.com TO CITE THIS ARTICLE: Danyk Y, Zborovska O, Pasyechnikova N. Strategies for the development of cyber-ophthalmology. J.ophthalmol.(Ukraine).2020;5:79-85. http://doi.org/10.31288/oftalmolzh202057985 Background: Making the tertiary management of eye diseases improved and widely available for all social groups in all parts of Ukraine is a pressing challenge for not only the Ministry of Health, but also for the state. Purpose: To provide scientific and theoretical assessment of establishing a new branch of ophthalmology, cyber-ophthalmology. Results: We demonstrated that the studied issue is relevant and important in the light of developments in tele- and cyber-medicine, expansion of application of information technologies to and introduction of artificial intelligence in medicine and in particular in ophthalmology. Conclusion: Cyber-ophthalmology is becoming reality and a systematically important branch of ophthalmology. Research in and developments of this branch are essential for providing tertiary eye disease management and improved disease treatment efficacy for all social groups. Keywords: cyber-ophthalmology, cyber-medicine, telemedicine, artificial intelligence, neurocomputer interface, cybersecurity
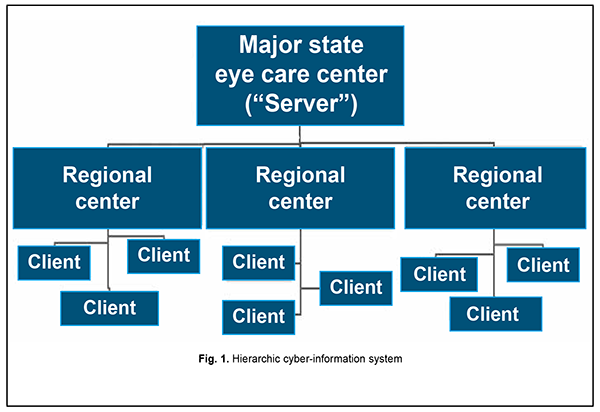
Introduction Few people can boast perfect vision and having no vision-related problems. Currently, the prevalence rate of eye disease in Ukraine is approximately 3,227 per 100,000 individuals [1], and the rates of disability due to visual impairments are still high. In Ukraine, the number of registered individuals with low vision or blindness is about 300 thousand (including 40 thousand of blind persons), which makes the prevalence rate of 37.69 per 10,000 population [3]. In addition, an estimated 213,223 people live with glaucoma (a prevalence rate of 612.7/100,000), and the prevalence rate of diabetic retinopathy, a disease requiring laser coagulation or surgery, is 458.0/100,000 [1]. Moreover, there is shortage of outpatient ophthalmologists in Ukraine, with the number of outpatient ophthalmologist posts exceeding the number of outpatient ophthalmologists employed (0.52/10,000 population vs 0.45/10,000 population). High everyday visual loads associated with working on a computer or other gadgets, driving, prolonged TV watching, watching 3D movies, and using virtual and augmented reality technology affect visual function. The situation may be aggravated for reasons related to the COVID-19 pandemic, with the corporate world switching over to “work from home” and the education to “study from home” concepts, and, consequently, with significantly increased both hours worked on gadgets and spent in cyberspace, and visual load and information load. It should be also taken into account that 80 percent of eye disorders are manifestations of other diseases of the body. Therefore, making the tertiary management of eye diseases improved and widely available for all social groups in all parts of Ukraine is a pressing challenge for not only the Ministry of Health, but also for the state. There is shortage of special eye care rooms (dispensaries and centers) practically in all regions of the country. The on-going reforms aim to meet this challenge through transfer of most eye care patients to private facilities and implementation of state-and-private partnership projects. The in-patient eye care in Ukraine also has a number of problems. In many places of the country, the requirements are not met with respect to the conditions, skilled personnel and high-tech equipment for diagnostic and treatment of eye disorders. The lack of availability of adequate eye care for rural people remains a serious issue of concern. All of that necessitates novel comprehensive high-tech approaches to improvement in eye care quality and availability. In order to meet the demands, we should (1) implement non-inpatient and resource-saving clinical technologies, (2) transfer some portions of conservative and surgical eye care to out-patient settings when the technologies available at the point-of-care make it possible (3) comprehensively improve measures for disease prevention, and (4) increase the rates of approaching eye care centers and diagnosing and treating eye disorders in a timely manner. In addition, we should utilize the potential of novel information and cyber technologies and advance the methodological and organizational foundations of ophthalmology to facilitate meeting the challenges. The purpose of the article was to provide scientific and theoretical assessment of establishing a new branch of ophthalmology, cyber-ophthalmology, and to consider a strategy for its development. Material and Methods The methods used in the research included system analysis (decision-making system and methods, consolidated information, data analysis), bibliographic, historical, concept modeling, and expert assessment. The material used in the research included the literature and information related to new developments in ophthalmology, telemedicine, cyber-medicine, cyber-physical systems, information and digital technologies. The relevant databases and material from PubMed, Scopus, Medline, Cochrane base, and Google scholar were subject to analysis. More than 1800 published sources were analyzed. Results As a branch of medicine studying visual system anatomy and physiology and eye disease treatment and prevention, ophthalmology has passed several phases of development. As a branch of medical science, it only began shaping in the early 19th century. It was only in the 20th century that new instrumental methods were developed for diagnosing eye disorders. In addition, at that time, new effective medications and surgical techniques (for corneal transplantation, retinal detachment, intraocular tumor photocoagulation, etc.) were developed. Ocular laser therapy and eye microsurgery were introduced into practice in the second half of the 20th century. A number of ophthalmological sub-specialties have been shaped to date, including laser ophthalmology, ocular microsurgery, neuro-ophthalmology, refractive surgery, cataract and glaucoma surgery, pediatric ophthalmology, strabismology, retinology, vitreo-retinal surgery, ocular traumatology, uveitis specialty, ophthalmocombustiology, ophthalmic oncology, corneal specialty, and optometry. Currently, the provision of care in an ophthalmological sub-specialty is associated with extensive application of electronic, information, telecommunication, robotic, cyber-physical, sensor and big data technologies, cybernetics, and technologies for medical data exchange and solving clinical, administrative, learning and scientific problems. Theory, methods and technologies of organization of their rational application for each ophthalmological sub-specialty, while used in a systematic and comprehensive way within the framework of ophthalmology in the context of improving efficacy and quality of eye care, are a subject of cyber-ophthalmology. The major task of cyber-ophthalmology is to collect, update, systematize and review critically the facts, synthesize new knowledge and perform generalizations that (a) describe phenomena and processes relevant to application of electronic, information, telecommunication, robotic, cyber-physical, sensor and large data processing, artificial intelligence, cybernetics, and medical data exchange technologies, and technologies for solving clinical, administrative, learning and scientific problems, and (b) allow establishing relations of cause and effect between them and predicting their behavior. The above phenomena and processes constitute the object of cyber-ophthalmology. Analysis of cyber-ophthalmology as a branch of ophthalmology and studies relevant to its components allow to single out its (1) purpose, (2) basic laws and general principles of the development (the theoretical component of cyber-ophthalmology), and (3) principles of practical application which are important for defining tasks, ways and means for establishing a branch-wise integrating cyber ophthalmological system, managing this system, and providing overall support for the process (the applied component of cyber-ophthalmology). Advances in telemedicine, medical cybernetics and cyber-medicine (application of computer and telecommunication technologies for medical data communication (e.g., doctor-doctor and doctor-patient communication), solving other medical problems with the help of information and communication technologies, and application of ideas, methods and equipment of cybernetics and robotic and cyberphysical systems in medicine and public health) initially underlay the formation of cyber-ophthalmology. The current functions of telemedicine include clinical, management, preventive, learning and scientific functions. The main task of telemedicine is the delivery of healthcare services, where distance and availability of tertiary healthcare professionals are critical factors. The aim of telemedicine is to provide expert-based health care to understaffed remote medical sites, and to optimize health care organization and control under these conditions. Today, the term “cyber medicine” is more suitable for describing high-tech medicine, applications of neurocomputer interface (or brain-computer interface), big-data medical systems, artificial intelligence, medical bioengineering, medical cyber-physical systems, robotic medicine and bionics. Most researchers understand cyber medicine as a theoretical and practical branch of medicine which is based on the phenomena and laws of the vital activities of the human body and its environment, and associated with relevant technologies, methods and methodologies of cybernetics. There are many examples of advances in cyber medicine in the context of the development and application of robotic and cyber-physical systems and facilities [4, 5, 7, 8, 11]. Robotic surgery began developing during the 1980s. Da Vinci Surgical System was one of the first robotic-assisted, minimally invasive surgical systems. The active development of bionic limbs (particularly, arms) began in the mid-20th century, and a lot of companies compete on this market. 3D-printed bionic arms are of relatively low cost. An eight-year-old boy, Freddie Payne, was the world's youngest person to be fitted with a 3D-printed bionic arm designed by Open Bionics. A visual prosthesis, often referred to as a bionic eye, is an experimental visual device intended to restore functional vision in those suffering from partial or total blindness. Many devices have been developed, usually modeled on the cochlear implant or bionic ear devices, a type of neural prosthesis [2]. The list of such devices includes Argus II, manufactured by Second Sight Medical Products Inc.; microsystem-based visual prosthesis (MIVP); implantable miniature telescope; microphotodiode array (MPDA) Project Alpha IMS, a subretinal prosthesis; artificial silicone retina (ASR); a photovoltaic retinal implant (PRIMA) bionic vision system; subchoroidal implant developed by Bionic Vision Technologies; Dobelle Eye (similar in function to the Harvard/MIT retinal implant, except the stimulator chip sits in the primary visual cortex, rather than on the retina); and intracortical visual prosthesis [10, 13]. Among others, companies like IBM, Google, Apple, Microsoft, and General Electric are already developing intelligent medical products and services. According to Venture Scanner, a research group, there are more than 800 AI-oriented companies worldwide. Companies from the US, UK, and Israel are most active in developing these technologies. Google’s DeepMind Health, a health AI system, analyzes the available information about the patient's symptoms and gives a list of recommendations, and the doctor, using the advice of such an assistant, prescribes a course of treatment for the patient. IBM's Watson Health is used to help establishing diagnoses and identify symptoms of cardiomyopathy, thrombosis and heart attacks. Artificial intelligence also allows assessing the effect of medication on the human body, and helps the physician to understand the way in which patient’s genetics exerts an impact on disease course and if a patient’s condition is going to improve with administration of a new medication. Using the IBM Watson Health Cloud healthcare technology, the doctor receives and analyzes data about the patient’s body from an electronic bracelet, and, on the basis of this, selects an effective course of treatment. Altris AI, a startup launched in Ukraine with its head office in Chicago and research and design department in Ukraine, aims to detect retinal conditions on OCT scans. The above projects and many others exemplify applications of AI, innovative information, sensor and cyber technologies aimed at treatment and rehabilitation. The main aim of cyber-ophthalmology is enabling the best results of eye care provision with a low investment of resources on the basis of (1) application of electronic, information, telecommunication, robotic, cyber-physical, sensor and, AI and cybernetic systems, and (2) rational organization of the operation of these systems in the area of ophthalmology. Basic laws and general principles of the development of cyber-ophthalmology Cyber-ophthalmology, therefore, is a systemically important branch of ophthalmology, and involves essential components of telemedicine and cyber-medicine among other high-tech components. Cyber-ophthalmology uses telemedicine as a tool for achieving the above aim. In some way, it may be said that cyber-ophthalmology is based on the systemic integration of advances from telemedicine, cyber-medicine, medical cybernetics and robotics, current information and cyber technologies in the area of ophthalmology, and is an essential and systemically important branch of ophthalmology. Diagnosis, treatment and prevention of eye disorders, medical data communication, implementation and use of the potential of telemedicine and medical cybernetics in ophthalmology still largely depend on the potential for processing, communication, interpretation and storage of big data, often much bigger than in other branches of medicine. Therefore, big data processing is of major importance in this context. There is a real need for application of novel comprehensive high-tech approaches to improvement in eye care quality and availability practically in all regions of Ukraine, especially with regard to rural areas. The above problem may be solved in general by developing a hierarchical client-server cyber-information system for eye care provision using information, telecommunication, network and cyber-physical systems. Let us consider a possible model of client-server cyber-information system for eye care provision under above conditions (Fig. 1). Such a system is composed of clients (local eye care provision points) and servers (regional eye care provision centers and a major eye care provision center). The basic idea is that centers have means for eye disease diagnosis and treatment, staff for secondary eye care provision, and patient and treatment databases, whereas clients (local primary eye care provision points) are equipped with external interfaces to allow for access to and enable interaction with centers with respect to medical examination and primary diagnosis. A regional server center maintains and controls these processes, is responsible for data integrity and storage, and provides operations for (a) determining the appropriate course of actions for each patient and (b) interaction on this matter with the major national center where the available national- and international-level ophthalmology-relevant data is stored and processed. Therefore, on the basis of current cyber information technologies, network architecture should be formed, with the tasks or network loads distributed over service providers (so-called servers) and local primary eye care provision points (so-called clients). Client-server network interaction will be performed via network protocols. Servers will receive service requests and provide the clients with resources in the form of real-time consultations and diagnosis, e.g., via Internet.
In addition, the eye care provision process will consist of phases that may be formalized and algorithmized in the following way. First, the first patient visit (routine eye examination) to the local primary eye care provision point (family physician), preliminary history taking and entering the history into the database for preliminary ophthalmological analysis, and, if required, sending a request through the network to the regional eye care provision center, and, if required, having consultation from specialists of the center. Second, entering the patient’s first visit and complaints data, and specifying measures taken in respective electronic logbook. Third, deciding whether the patient should be treated at the local eye care provision point or referred for secondary or tertiary diagnostics and treatment to the regional center. Fourth, examining the patient at the regional center (if required, with involvement of remote examiners from the major national eye care center) and deciding whether the patient should be treated at the former center or referred for secondary or tertiary diagnostics and treatment to the latter center. Fifth, examining and diagnosing the patient at the major national eye care center and deciding on further treatment and rehabilitation options. Finally, providing information support for the patient and physician’s actions at all stages of eye care delivery. Discussion Practical application principles In general, the national cyber-ophthalmology system may be composed structurally and technically from (1) the basic national cyber-ophthalmology network and (2) the national cyber-ophthalmology network advanced on the basis of state-and-private partnership. Either of them should include primary eye care provision points, regional eye care provision centers and the major national tertiary eye care provision center. In addition, these points and centers should be equipped with relevant (1) electronic, cyber-physical and data systems for diagnosis and treatment and (2) information and communication and computer systems for maintaining the cyber-ophthalmology system with relevant software, control systems and databases. Moreover, the points and centers should be staffed with medical and IT staff. The feature of the national cyber-ophthalmology system is that its functional and structural components are consolidated in the complex adaptive cybernetic system having specific aim, functions, tasks, organizational structure, direct connections and feedbacks, to provide early and adequate eye care to patients, and in accordance with a unified design and plan. This system – in the sense of the system theory – is a complex multilayer hierarchical system that has some functions and components with interrelations relevant to medical care levels. Early and accurate diagnosis is essential for preserving full vision. Numerous general diagnostic tools and specific electronic information-and-cybernetic tools are available that can provide and store digital diagnostic data. This enables developing and using the electronic patient record (EPR) and developing and implementing the electronic health record system in ophthalmology. The introduction of diagnostic technologies in eye disease care has facilitated our understanding of the pathogenetic aspects of ocular disease, the development of novel disease prevention methods, and laid the basis for new approaches to disease treatment and assessment of treatment efficacy. Precision, non-invasive and objective diagnostic systems with an archiving feature facilitate establishing the diagnosis in subclinical or early clinical disease stages, provide early indications for treatment and assessment of treatment efficacy, and enable automated EPR management and storage in relevant databases on the spot and, if required, at the major eye care provision center. There is a requirement for a properly equipped center for reading, sorting and interpreting the collected diagnostic data. Collecting health-related patient data followed by correct structuring, interpretation and application of this data in diagnostic procedures will lead to early care provision and personalized treatment. This is what such global companies as IBM and Google deal with today [9, 10]. In addition, this is associated with the challenge of big ophthalmological data processing. As regards the specific use of the notion of ‘big data’ in ophthalmology, the following point should be made. Problems with appropriate early referrals of patients by family physicians and primary care ophthalmologists to tertiary eye care institutions are common in the absence of the system proposed for cyber-ophthalmology or if the system cannot perform big data operations. In addition, a substantial portion of the patients referred to tertiary eye care institutions are referred too late or wrongfully, which results in reduced treatment efficacy or a loss of time or other resources, respectively. We are striving to optimize the efficacy of the ophthalmologist’s work in primary and secondary eye care settings, and to provide a patient with adequate and early medical care, particularly, through the use of best practices of applications of technologies for processing big medical datasets in national eye care practice. For this purpose, we may use the existing universal technologies with a potential to assist ophthalmologists in recording the data required for diagnosis of eye disease while remote access to regional or major ophthalmological center for data collection, processing, analysis, storage and communication (CDCPASC) is available. These study methods should be readily available, have the same characteristics for all eye care clinics and rooms, and provide digitizable results. It is noteworthy that implementation of this step requires high-skilled ophthalmologists eager to learn novel cyber-diagnostic methods. However, we should not neglect mobile gadgets and smartphone data collection applications that would be readily available and understandable for patients [13]. In addition, the requirement for a uniform standard for interpretation of obtained data is essential. The best approach in this case would be to use the current available and develop new software for data collection, processing, analysis, sorting, integration, decoding and interpretation. In so doing, we should take into account that there have been reports on a more accurate disease diagnosis by AI than by a physician [12], although AI is not yet adequate to replace a clinically skilled physician. The CDCPASC should be staffed with a specialist with skills in maintenance of AI and big data software to improve the efficacy of implementing cyber-ophthalmology technologies for early and adequate eye disease diagnosis. In addition, the CDCPASC should be equipped with adequate sensor and cyber-information tools and systems for data collection, processing and storage and fast internet connection to facilitate on-line diagnosis. Under current conditions and forecasted future conditions, the processes accompanying the activities in any component of or the entire eye care delivery system, include co-operation of the complex system of interconnected components of different origin (e.g., technical, biological, social, etc.), staff and the cyber-physical systems capable of data reception, storing, transformation and communication in accordance with the specified purpose and under complex coordinated control, which are the classical signs of a cybernetic system and medical cybernetics within the framework of ophthalmology. This, in turn, is leading to the formation and development of a separate branch of ophthalmology, which studies the patterns of and pursues these processes. Information and communication and cyber-physical technologies have changed life and basic principles of operation of entire industries and branches of healthcare over the recent 30-40 years. Ophthalmology is a branch of medicine in which these technologies are already becoming systemically important and essential for delivering adequate eye care to all segments of the population. The major trends in cyber-ophthalmology are (1) ensuring the possibility of early provision of adequate eye care throughout the country and (2) obtaining access to and exchanging required data anytime and anyplace, with the capability of big data operations and processing with application of, e.g., cloud technologies (flexible storing and processing of scaled data) and having all of the necessary data safety measures and cyber-safety measures in general in place. Therefore, now we are at the start of a sea change in medicine and particularly in ophthalmology. Cyber-ophthalmology should be further and systemically implemented in the framework of the development of advanced technologies and their application in medicine, in order to make cyber-ophthalmology reality, a systematically important branch of ophthalmology and having grounds for further advances. Research in and developments of this branch are essential for providing tertiary eye disease management and improved disease treatment efficacy for all social groups. However, the emergence and effective development of cyber-ophthalmology depends on a number of objective and subjective factors. According to an article published in Gazeta Lekarska (issue No.267, 1937, p.15), telemedicine was first applied in 1935 in Lviv, when Ukrainian professors Marian Franke and Witold Lipinski organized a permanent operation of tele-electrocardiography. We hope that the introduction of cyber-ophthalmology will be also associated with our country. In addition, the development of aids for data categorization, interpretation, delegation, and snooping becomes increasing topical, and cyber threats make data processing and communication challenging and require advanced and reliable data protection. In the current work, we analyzed the aspects of the establishment and the major trends in the development of telemedicine, cyber-medicine, neurocomputer interfaces and cyber-information components of ophthalmology in the context of the formation cyber-ophthalmology, a new branch in ophthalmology. Cyber-ophthalmology is a component and separate branch of ophthalmology, which represent the theory and practice of applications of ideas, methods and equipment of electronic, information, telecommunication, robotic, cyber-physical, sensor and large data processing technologies, artificial intelligence and cybernetics for studies in ocular anatomy and physiology and eye disorders, and developing and application of the methods of eye disease treatment and prevention and ocular prosthetics, medical data communication, and solving clinical, administrative, learning and scientific problems to improve eye care delivery. Therefore, the work presented the major development phases and prospects of cyber-ophthalmology in a changing digital world on the bases of findings of system analysis and studies.
References 1.Karmazina OO, Release Officer. [Healthcare institutions in and disease prevalences in the population of Ukraine in 2017]. Kyiv: State Statistics Service of Ukraine; 2018. Ukrainian. 2.Visual prosthesis. https://en.wikipedia.org/wiki/Visual_prosthesis 3.Iakushenko LM. [Current issues of social protection of disabled persons]. Sotsialna polityka. 2009;9. Ukrainian. 4.Chun DW, Heier JS, Raizman MB. Visual prosthetic device for bilateral end–stage macular degeneration. Expert Review of Medical Devices. 2005 Nov;2(6):657-65. 5.Farandos NM, Yetisen AK, Monteiro MJ, et al. Contact Lens Sensors in Ocular Diagnostics. Adv Healthc Mater. 2015;4:792–810. 6.Fernandes RA, Diniz B, Ribeiro R, Humayun M. Artificial vision through neuronal stimulation. Neurosci Lett. 2012;519(2):122–8. 7.Miyawaki Y, Uchida H, Yamashita O, et al. Visual Image Reconstruction from Human Brain Activity using a Combination of Multiscale Local Image Decoders. Neuron. 2008 Dec 10;60(5):915-29. 8.Rush AD, Troyk PR. A power and data link for a wireless–implanted neural recording system. IEEE Trans Biomed Eng. 2012 Nov;59(11):3255-62. 9.Santhanam G, Ryu SI, Yu BM, et al. A high–performance brain–computer interface. 2006 Jul 13;442(7099):195-8. 10.Vidal J. Toward Direct Brain–Computer Communication. Annu Rev Biophys Bioeng. 1973;2:157-80. 11.Wolpaw JR, McFarland DJ, Neat GW, et al. An EEG–based brain–computer interface for cursor control. Electroencephalogr Clin Neurophysiol. 1991 Mar;78(3):252-9. 12.Wolpaw JR, Birbaumer N, Heetderks WJ, et al. Brain–Computer Interface Technology: A Review of the First International Meeting. IEEE Trans Rehabil Eng. 2000 Jun;8(2):164-73. 13.Fernandes RA, Diniz B, Ribeiro R. Artificial vision through neuronal stimulation. Neuroscience Letters. 2012;519(2):122-8.
The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|