J.ophthalmol.(Ukraine).2020;6:19-24.
|
http://doi.org/10.31288/oftalmolzh202061924 Received: 25 August 2020; Published on-line: 21 December 2020 Comparing detection rates of near-infrared transpalpebral transillumination, ultrasonography and radiography for foreign bodies in the anterior segment of the eye M. B. Kogan, O. S. Zadorozhnyy, O. S. Petretska, T. A. Krasnovid, A. R. Korol SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine"; Odesa (Ukraine) E-mail: mihailkogan2@gmail.com TO CITE THIS ARTICLE: Kogan MB, Zadorozhnyy OS, Petretska OS, Krasnovid TA, Korol AR. Comparing detection rates of near-infrared transpalpebral transillumination, ultrasonography and radiography for foreign bodies in the anterior segment of the eye. J.ophthalmol.(Ukraine).2020;6:19-24.http://doi.org/10.31288/oftalmolzh202061924 Background: Penetrating globe injury is a leading cause of registered visual disability among working-age adults. Despite advances in imaging techniques, the detection of an intraocular foreign body (IOFB) in the projection of the ciliary body is still a challenge for the ophthalmologist. Purpose: To compare detection rates of near-infrared transpalpebral transillumination, ultrasonography and radiography for foreign bodies situated in the anterior segment of the eye. Material and Methods: Thirty male patients (30 eyes; age, 21 to 65 years) with penetrating globe injuries and suspected foreign body in the anterior segment of the eye (the anterior chamber, lens, anterior vitreous cavity) were under our observation. The fellow eye was unaffected. Patients underwent visual acuity assessment, biomicroscopy, ophthalmoscopy, ultrasound scanning of the anterior and posterior segment of the eye, ultrasound biometry, radiography and near-infrared transpalpebral transillumination (NIR TPT). Results: The use of a non-invasive NIR TPT method in conjunction with traditional imaging modalities (radiography and ultrasound) resulted in a ten percent increase in the rate of detection of anterior segment foreign bodies due to the detection of some X-ray-negative IOFBs and identification of small (less than 1 mm) IOFBs. Conclusion: The NIR TPT method allows for non-invasive visualization of anterior segment foreign bodies of various compositions in patients with penetrating globe injuries. The use of a non-invasive NIR TPT method in conjunction with traditional imaging modalities resulted in a ten percent increase in the rate of detection of foreign bodies due to the detection of some X-ray-negative IOFBs and identification of small (less than 1 mm) IOFBs. Massive subconjunctival hemorrhages hamper adequate detection of foreign bodies in the projection of the ciliary body by NIR TPT due to intensive absorption of near-infrared light. Keywords: penetrating globe injury, intraocular foreign body, infrared radiation, transillumination
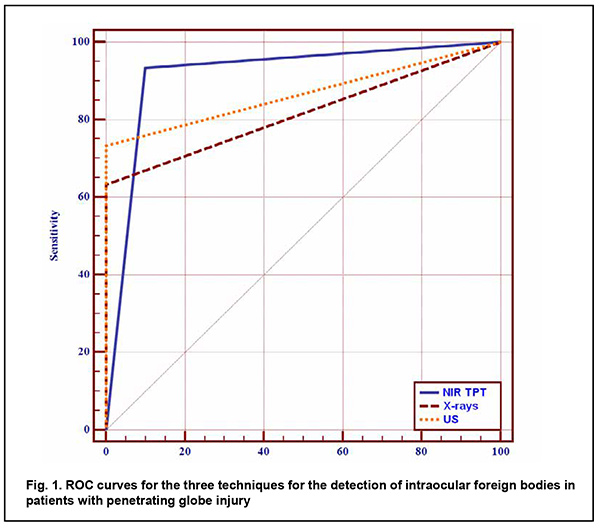
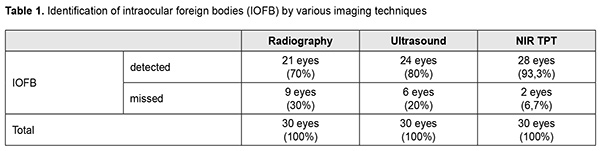
Introduction Penetrating globe injury is a leading cause of registered visual disability among working-age adults. Intraocular foreign bodies (IOFBs) account for 18%-41% of all penetrating globe injuries. The visual prognosis of an injury with an IOFB is determined by the size, composition, depth and location of the foreign body, and its duration in situ [1-3]. Endophthalmitis is one of the most severe potential complications of penetrating globe injury. Among patients with infectious endophthalmitis, post-traumatic endophthalmitis comprises about 10–30% of cases. Factors associated with increased risk of endophthalmitis following penetrating trauma include retained IOFB, delay in wound closure of >24 h and injury in a rural setting. Soil contamination is believed to result in a higher rate of endophthalmitis for open globe injuries occurring in a rural versus a non-rural setting. Endophthalmitis developed in 30% of patients with rural penetrating trauma, compared with 11% of patients with non-rural penetrating trauma [4, 5]. The incidence of endophthalmitis was higher after IOFB-related penetrating globe injury than after penetrating globe injury without IOFB [6]. Metallosis is a dangerous complication after metallic IOFB-related penetrating globe injury. It occurs through damage to intraocular tissue through toxic effects of retained metallic IOFB, these effects manifesting clinically as recurrent episodes of choroidal inflammation. Clinical manifestations developing as early as the first weeks after the traumatic event and cases of metallic foreign bodies presenting years after the initial trauma without causing severe ocular inflammatory response have been rarely reported [7-11]. Therefore, early detection of an IOFB is not only important for selecting the most appropriate surgical treatment strategy but also a factor influencing the treatment outcome. Despite continuous advances in imaging techniques, early detection of an IOFB is still a challenge for the ophthalmologist. Visualizing a ciliary body IOFB is especially challenging. Approximately 5% of IOFBs are found in the projection of or close to the ciliary body [3, 7]. Computed tomography (CT), radiography with the Komberg-Baltin prosthesis, ultrasonography and magnetic resonance imaging (MRI) are the most effective techniques for detecting and localizing an IOFB. Nevertheless, there are an ample number of reports of missed anterior chamber IOFBs [8, 10]. We have previously demonstrated that near-infrared transpalpebral transillumination (NIR TPT) is a modality enabling easy and non-invasive visualization and assessment of the sizes of ciliary body structures [11-13]. In addition, NIR TPT enables visualization of shadows of ciliary body IOFBs of various origin (metallic, stone and wood) in patients with penetrating globe injuries. The use of NIR TPT as means for visualizing an IOFB in conjunction with traditional imaging modalities seems promising and would improve our ability to diagnose these patients preoperatively [14-16]. The purpose of the study was to compare detection rates of near-infrared transpalpebral transillumination, ultrasonography and radiography for foreign bodies situated in the anterior segment of the eye. Material and Methods This was an open-label, prospective and non-interventional study. This study was performed within the framework of a planned research design and the study protocol was approved by the Bioethics Committee of the Filatov Institute. The study followed the ethical standards stated in the Declaration of Helsinki, the European Convention on Human Rights and Biomedicine and relevant laws of Ukraine. Informed consent was obtained from all study subjects. Thirty male patients (30 eyes; age, 21 to 65 years) with penetrating globe injuries and suspected foreign body in the anterior segment of the eye (the anterior chamber, lens, anterior vitreous cavity) were under our observation. They underwent visual acuity assessment, biomicroscopy, ophthalmoscopy, metal detector examination, anteroposterior and lateral radiography (both with and without using the Komberg-Baltin prosthesis), ultrasound biometry, ultrasound scanning of the anterior eye and posterior eye; ultrasound distant perimetry; metal detector examination; and NIR TPT. A diagnosis of IOFB was confirmed or denied by the three imaging modalities (NIR TPT, ultrasound scanning and X-ray examination) using the signs that were specific for each of the modalities. The NIR TPT system used consisted of (1) a wireless infrared light-emitting-diode light source with a dominant wavelength of 940 nm and (2) slit-lamp attachable monochrome video camera (Blackfly®, FLIR Integrated Imaging Solutions Inc., Canada) capable of recording NIR images and video [14, 15, 17]. The transpalpebral illumination study was performed with the patient sitting at the slit lamp. Images of scleral shadows of the IOFB, pars plicata and pars plana were taken and saved in the computer. We used the Aviso ultrasound (Quantel Medical; Cournon d'Auvergne, France) with 10-MHz and 50-MHz linear probes for the posterior and anterior segments of the eye, respectively. The ultrasound study was performed with the patient lying on his back, and with the head of the bed raised. In the ultrasound study with the anterior probe, patients were administered topical anesthesias with ophthalmic 0.5% proparacaine hydrochloride (ALCAINE®, SA Alcon-Couvreur NV, Puurs, Belgium), and, subsequently, Vidisic Eye Gel (Dr. GERHARD MANN Chem.-Pharm. Fabrik, Berlin, Germany) as a contact gel. The posterior probe was placed over the patient’s closed eyelid to scan the eye non-invasively. Targeted anteroposterior and lateral radiography (with the Komberg-Baltin prosthesis) was performed using a Proteus XR/a radiography system (GE Healthcare, Milwaukee, Wis), and patients were administered topical anesthesias with ophthalmic 0.5% proparacaine hydrochloride (ALCAINE®). Contact invasive imaging studies (radiography with the Komberg-Baltin prosthesis, ultrasound scanning of the anterior eye and ultrasound biometry) were not performed in patients with a non-adapted corneal or scleral wound. Receiver operating characteristic (ROC) curves were constructed to obtain graphical representation of selectivity and specificity, and the area under the ROC curve was calculated to compare the efficacy of various imaging techniques for detection of foreign bodies in the anterior eye. Predictive characteristics for the techniques for the detection of IOFBs are reported as mean and 95% confidence intervals (CI). Statistical analyses were conducted using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software [18]. Results An intraocular foreign body was detected in the anterior segment (the anterior chamber, lens, anterior vitreous cavity) in all the 30 patients. Of the 30 eyes with IOFB, a foreign body was identified and localized by radiography in 21 eyes (70%). Radiography failed to detect a foreign body in the rest 9 eyes (30%) because the foreign body was either composed of organic material (rock or wood) or metallic and small (less than 1.0 mm). Of note that, in 6 patients (20%), a foreign body was found by radiography, but it was not possible to localize it with the Komberg-Baltin prosthesis due to the non-adapted wound of the globe and associated risk of iatrogenic complications. Radiography showed no false positives, but 3 false negatives, all of which were associated with small (≤0.5 x 0.5 mm) metallic foreign bodies. Of the 30 eyes with IOFB, a foreign body was identified by ultrasound in 24 eyes (80%). Ultrasound scanning of the anterior eye could not be performed in 6 patients (20%) due to the non-adapted wound of the globe. Ultrasonography showed no false positives. NIR TPT revealed a foreign body in the anterior eye in 28 eyes (93.3%) of the 30 eyes with IOFB. Particularly, NIR TPT found a foreign body in the anterior segment in 3 eyes in which either an IOFB was missed by radiography and ultrasound, or ultrasound could not be performed. NIR TPT failed to detect a foreign body in 2 eyes (6.6%). In one of these two eyes, a foreign body could not be detected by NIR TPT because of shielding effect of massive subconjunctival hemorrhage, but it was detected both by radiography and ultrasound. In the other eye, neither of the imaging modalities could detect the IOFB because the latter was too small, but the foreign body was revealed during surgery. In addition, two eyes were mistakenly found to have a foreign body in the anterior vitreous (false positive results) by NIR TPT, but this was subsequently confirmed neither by radiography nor by ultrasound. These two patients had subconjunctival and vitreous hemorrhages. Of note is that the method we have developed (1) enabled the diagnosis of IOFB in swollen and opaque lens masses and opaque corneas, and (2) correctly detected not only X-ray positive foreign bodies, but also X-ray-negative foreign bodies. ROC analysis of the IOFB detection methods was performed for 50 eyes; the presence of a foreign body was confirmed for 30, and the absence of a foreign body was confirmed for 20 of these eyes. ROC curves for the three IOFB detection methods are shown in Figure 1.
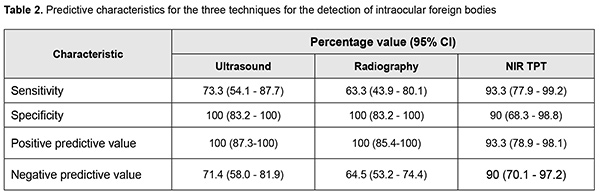
The area under curve (AUC) for NIR TPT was 0.92 (95% CI, 0.80–0.98); for radiography, 0.82 (95% CI, 0.68–0.91), and for ultrasound, 0.87 (95% CI, 0.74–0.95), demonstrating good efficacy of all the three IOFB detection methods, although there was no significant difference (p > 0.05) in AUC between each two of them. Table 2 shows predictive characteristics of the methods under analysis.
Discussion Inadequate foreign body visualization is the main reason of unsuccessful removal attempts and late removal of foreign bodies situated in the anterior segment of the eye [19-21]. Although radiography is an effective imaging modality enabling detection and accurate localization of an IOFB, detecting an X-ray negative foreign body by radiography is difficult. Thus, the foreign bodies composed of organic materials (stone or wood) were missed by radiography in our study. In addition, small (≤ 1.0 mm) metallic foreign bodies may be missed by radiography due to their shape and/or location in the anterior chamber angle, beneath the iris, or in the ciliary body area, which was confirmed by the current study. Moreover, accurate IOFB localization by radiography with the Komberg-Baltin prosthesis sometimes cannot be performed due to the non-adapted wound of the globe and/or associated risk of iatrogenic complications. Ultrasonography is another imaging modality proved to be effective in detecting foreign bodies of various sizes, shapes, materials and locations (including the anterior segment of the eye). In some cases, however, ultrasonography should not be performed due to high risk of iatrogenic complications. Patients with non-adapted corneal or scleral defects may have additional wound infection; prolapse of the retina, choroid or sclera; or iatrogenic expulsive hemorrhage due to globe contact with or compression by the probe that is applied directly upon the surface of the globe [22]. Thus, ultrasound study of the anterior segment of the eye could not be safely performed in 19.8% of study patients due to the presence of a non-adapted globe wound, which limited out ability to diagnose IOFB in these patients. The use of near-infrared LED illumination in NIR TPT enables transillumination not only through the sclera, but even through the patient’s lid. In addition, absence of physical contact between LED light source and the cornea and sclera allows excluding complications and trauma of these ocular structures. We managed to conduct the NIR TPT procedure quickly and safely with as little pain and discomfort to the patient as possible in all cases of the study. Particularly, no iatrogenic damage was observed after performing the procedure in patients with non-adapted corneal and scleral defects. The use of LED as a source of infrared light simplifies the globe transillumination system, and there is no need for the use of optic fibers to transmit the light radiation to the eye. The LED light source is a compact wireless device that needs no additional infrared filters. One may use infrared LEDs of different wavelengths to achieve better visualization of the globe. With the use of near-infrared light for globe transillumination, there is no glare from bright visible light, which makes the conduct of studies in this patient category easier. The proposed visualization approach enables taking real-time photographs and shooting real-time video of TPT pictures [11-13]. In addition, we managed to visualize IOFBs of various compositions and dimensions, particularly, in the presence of opaque media using NIR TPT. Thus, NIR TPT found a foreign body in the anterior eye in the three eyes (10% of the study patients) in which either an IOFB was missed by radiography and ultrasound, or ultrasound could not be performed due to the presence of a non-adapted globe wound. Moreover, NIR TPT enables visualizing ciliary body structures and localizing and measuring the dimensions of shadows cast by these structures on the sclera [14-16]. Thus, in the current study, we managed to localize an IOFB shadow with respect to shadows cast by ciliary body structures on the sclera, which allowed localization of a foreign body and selecting the most appropriate surgical treatment strategy. The method of NIR TPT, however, has certain drawbacks. For example, a foreign body in the projection of the ciliary body is difficult to identify in the presence of massive subconjunctival hemorrhage due to a shielding effect of blood with respect to the near-infrared light. In addition, intensive absorption of near-infrared light by subconjunctival blood in some cases led to incorrect assessment of NIR TPT pictures and false positive results. The use of a non-invasive NIR TPT in conjunction with traditional imaging modalities (radiography and ultrasound) resulted in a ten percent increase in the rate of detection of anterior segment foreign bodies due to the detection of some X-ray-negative IOFBs and identification of small (less than 1 mm) IOFBs. References 1.Lima-Gómez V, Blanco-Hernández D, Rojas-Dosal J. Ocular trauma score at the initial evaluation of ocular trauma. Cir Cir. May-Jun 2010;78(3):209-13. 2.Loporchio D, Mukkamala L, Gorukanti K, Zarbin M, Langer P, Bhagat N. Intraocular foreign bodies. Surv Ophthalmol. 2016; 61(5):582-96. 3.Zhang Y, Zhang M, Jiang C, Qiu HY. Intraocular foreign bodies in China: clinical characteristics, prognostic factors, and visual outcomes in 1,421 eyes. Am J Ophthalmol. 2011;152(1):66-73. 4.Kuhn F, Pieramici DJ. Intraocular foreign bodies, In: Ferenc K, Pieramici D (eds) Ocular Trauma: Principles and Practice. New York, Thieme; 2002, p. 235-63. 5.Potts AM, Distler JA. Shape factor in the penetration of intraocular foreign bodies. Am J Ophthalmol. 1985;100(1):183-7. 6.Reynolds DS, Flynn HW, Jr. Endophthalmitis after penetrating ocular trauma. Curr Opin Ophthalmol. 1997; 8:32–38. 7.Arora R, Sanga L, Kumar M, Taneja M. Intralenticular foreign bodies: report of eight cases and review of management. Indian J Ophthalmol. 2000;48:119-22. 8.Lee W, Park SY, Park TK, Kim HK, Ohn YH. Mature cataract and lens-induced glaucoma associated with an asymptomatic intralenticular foreign body. J Cataract Refract Surg. 2007 Mar;33(3):550-2. 9.Lin YC, Kuo CL, Chen YM. Intralenticular foreign body: A case report and literature review. Taiwan J Ophthalmol. 2019;9(1):53–59. 10.Raina U, Kumar V, Kumar V, Sud R, Goel N, Ghosh B. Metallic intraocular foreign body retained for four years – an unusual presentation. Cont Lens Anterior Eye. 2010;33:202-4. 11.Tokoro M, Yasukawa T, Okada M, Ogura Y, Uchida S. Copper foreign body in the lens without damage of iris and lens capsule. Int Ophthalmol. 2007;27(5):329-31. doi: 10.1007/s10792-007-9074-5. 12.Zadorozhnyy O, Alibet Yassine, Kryvoruchko A, Levytska G, Pasyechnikova N. Dimensions of ciliary body structures in various axial lengths in patients with rhegmatogenous retinal detachment. J Ophthalmol (Ukraine). 2017;6:32-6. 13.Zadorozhnyy O, Korol A, Nevska A, Kustryn T, Pasyechnikova N. Ciliary body imaging with transpalpebral near-infrared transillumination – a pilot study. Klinika oczna. 2016;3:184-6. 14.Kogan M, Zadorozhnyy O, Petretska O, Krasnovid T, Korol A, Pasyechnikova N. [Imaging of Intraocular Foreign Bodies Located in the Projection of the Ciliary Body by Infrared Transillumination (Pilot Study)]. Klin Monbl Augenheilkd. 2020; 237(07): 889-93. German. 15.Kogan MB. Visualization of anterior eye structures by near-infrared transillumination in patients with contusions of the globe. J Ophthalmol (Ukraine). 2020;2:46-50. 16.Kogan MB, Zadorozhnyy OS, Petretska OS, Krasnovid TA, Korol AR, Pasyechnikova NV. Visualization of intraocular foreign bodies in the projection of the ciliary body by transpalpebral near-infrared transillumination. J Ophthalmol (Ukraine). 2019;4:23-27. 17.Zadorozhnyy O, Guzun O, Kustryn T, Nasinnyk I, Chechin P, Korol A. Targeted transscleral laser photocoagulation of the ciliary body in patients with neovascular glaucoma. J Ophthalmol (Ukraine). 2019;4:3-7. 18.Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–458. doi: 10.1038/bmt.2012.244 19.Coleman DJ, Lucas BC, Rondeau MJ, Chang S. Management of intraocular foreign bodies. Ophthalmology. 1987; 94: 1647–53. 20.Erikitola O, Shahid S, Waqar S, Hewick S. Ocular trauma:classification, management and prognosis. Brit J Hosp Med. 2013;74:108-11. 21.Pandey A.N. Ocular Foreign Bodies: A Review. J Clin Exp Ophthalmol. 2017; 8:645. 22.Navon SE. Management of the ruptured globe. Int Ophthalmol Clin. 1995;35:71-91. The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|