J.ophthalmol.(Ukraine).2021;1:10-16.
|
http://doi.org/10.31288/oftalmolzh202111016 Received: 27 May 2020; Published on-line: 12 February 2021 Objective criteria of the axial and refractive components in the modified classification for distinguishing among axial, refractive, mixed and combinatory myopias proposed based on the analysis of morphometric parameters of myopic and emmetropic eyes O.V. Maliieva, N.M. Bushuieva SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine; Odesa (Ukraine) E-mail: doc.malieva@gmail.com TO CITE THIS ARTICLE: Maliieva OV, Bushuieva NM. Objective criteria of the axial and refractive components in the modified classification for distinguishing among axial, refractive, mixed and combinatory myopias proposed based on the analysis of morphometric parameters of myopic and emmetropic eyes. J.ophthalmol.(Ukraine).2021;1:10-6. http://doi.org/10.31288/oftalmolzh202111016 Background: Myopia is heterogeneous with regard to its origin and varies in its course and prognosis of sequelae. The lack of criteria does not allow in practice to distinguish among different types of the disease. Purpose: First, to study morphometric parameters characterizing the axial and refractive components (the axial length (AL) and corneal refractive power (CRP)) in myopes and emmetropes, and; second, to develop the criteria for selecting the ranges for axial, refractive, mixed and combinatory myopias based on the statistical analysis of AL and CRP. Material and Methods: Two hundred and sixty four patients (502 eyes) with various severities of myopia (mean myopic refractive error, –2.74 ± 2.41 D) and 78 emmetropes (145 eyes) were included in the study. Patients underwent visual acuity assessment for distance; autokeratorefractometry; measurement of horizontal pupil diameter and horizontal corneal diameter; ultrasonography of the posterior and anterior segments of the eye for AL, anterior chamber depth, and lens thickness measurements and pachymetry; and uncorrected intraocular pressure (IOP) and IOP corrected for pachymetry measurements. Results: The objective limits for different types of myopia were calculated based on the axial component (AL, 24.3 mm) and refractive component (CRP, 43.86 D). The newly developed objective criteria allow for establishing the type of myopia corresponding to axial and refractive components on the basis of corneal refractive power and axial length of the eye. The proposed modified classification of the types of myopia takes in account the axial and refractive components and allows for distinguishing practically among refractive myopia (AL ≤ 24.3 mm and CRP > 43.86 D), axial myopia (AL > 24.3 mm and CRP ≤ 43.86 D), mixed myopia (AL > 24.3 mm and CRP > 43.86 D), and combinatory myopia (AL ≤ 24.3 mm and CRP ≤ 43.86 D, similar to emmetropes). Keywords: myopia, classification, emmetropia, axial length of the eye, corneal refractive power, corneal radius
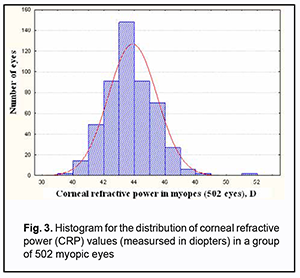
Introduction The global prevalence of myopia has been rising steadily over the past few decades [1-4]. It is difficult to distinguish among different types of the disease, because myopia is heterogeneous [5-7] with regard to its origin, varies in its course and prognosis of complications, and there are no clear criteria for distinguishing among the types. For example, a diagnosis of degenerative myopia can be established only in the presence of changes in the fundus [8, 9]. The onset of refractive myopia is more common in early school ages [1, 3, 10] due to increased near vision load [11, 12]. Some studies found that eyes with larger axial length tend to have flatter cornea (and, correspondingly, less corneal refractive power), whereas others reported that the more general expectancy of rather flat corneas in high myopia was not fulfilled [13, 14]. Several studies have shown that myopic eyes have greater mean corneal powers than emmetropic eyes; this may be mostly due to greater corneal powers being a risk factor for youth-onset myopia [15]. When myopia develops, in some cases the cornea may undergo a “paradoxical” steepening, which accelerates, rather than retards, the development of myopia [15]. The literature reflects the idea of refractive myopia as myopia with an emmetropic axial length [16]. Schmid (2021) [16] characterized two categories of myopia (axial myopia and refractive myopia), and distinguished four forms of axial myopia. Ludwig and colleagues [17] stressed that myopic pathology can affect all regions of the retina, though there is currently no classification system to distinguish anterior (peripheral) and posterior (macular) pathology. They hypothesized that these classifications are characterized by distinct demographic and refractive features, highlighting the disparity in types of pathologic myopia, and concluded that, high myopia may be divided into four distinct subgroups based on the presence and location of pathology, which is associated with differences in age, gender, race, and refractive error. The variety in clinical refraction is caused by a combination of a number of anatomical and optical parameters of the eye [18-21]. Tron (1947) [21] performed biometric measurements of and studied patterns of changes in some anatomical and optical parameters in 62 emmetropic eyes, and distinguished four types of myopia (axial, refractive, mixed and combinatory) based on the ranges of the anterior length and refractive power in these eyes [21]. The absence of objective criteria does not allow differentiating between these types of myopia. The purpose of the study was twofold: first, to study morphometric parameters characterizing the axial and refractive components (such as the axial length (AL) and corneal refractive power (CRP)) in myopes and emmetropes, and; second, to develop the criteria for selecting the ranges for axial, refractive, mixed and combinatory myopias based on the statistical analysis of AL and CRP. Material and Methods A total of 264 patients (502 eyes; mean age, 18.41 ± 10.14 years) with various severities of myopia (mean myopic refractive error under cycloplegic conditions, –2.74 ± 2.41 D) were included in this study. Of these, 178 (338 eyes; 67.33%) were female and 86 (164 eyes; 32.66%) were male. The control group included 78 emmetropes (145 eyes; mean age, 23.42 ±18.63 years). Of these, 54 (104 eyes; 71.25%) were female and 24 (41 eyes; 28.75%) were male. Patients underwent visual acuity assessment for distance; autokeratorefractometry (Accuref–K 9001, Shin Nippon), including measurement of actual refractive error under cycloplegic conditions, 30 minutes after the pupil was dilated with 1% cyclomed; measurement of horizontal pupil diameter (keratotopography, РСТ–110, Optopol, Poland) and horizontal corneal diameter (KR–8900 Topcon and HRK–7000 Huvitz); ultrasonography of the posterior and anterior segments of the eye for AL, anterior chamber depth (ACD), and lens thickness (CT) measurements and pachymetry (Desmin M; Optopol); and uncorrected intraocular pressure (IOP) (Reichart–АТ555) and IOP corrected for pachymetry (Desmin M) measurements. Statistical analysis of the morphometric parameters of the eyes for the total sample and for the distinguished groups was carried out. Median and skewness (A) values were calculated in addition to mean and standard deviation values. The features of parameter distribution were used as the basis for subsequent selection of the methods for testing asymmetry hypotheses and analyzing the relationships among structural and functional characteristics. Statistical analyses were conducted using Microsoft Excel and Statistica 12.0 (StatSoft, Tulsa, OK, USA) software. Results In this work, we studied ocular morphometric parameters (especially mean AL and CRP) in emmetropes, because these parameters are key indicators for distinguishing among myopic eyes based on the axial or refractive component. In the group of emmetropes, the refractive error under cycloplegic conditions ranged from 0.5 D to +0.5 F, and AL, from 22.11 mm to 25.08 mm (Table 1). Statistics for ocular morphometric parameters of emmetropes are shown in Table. 1.
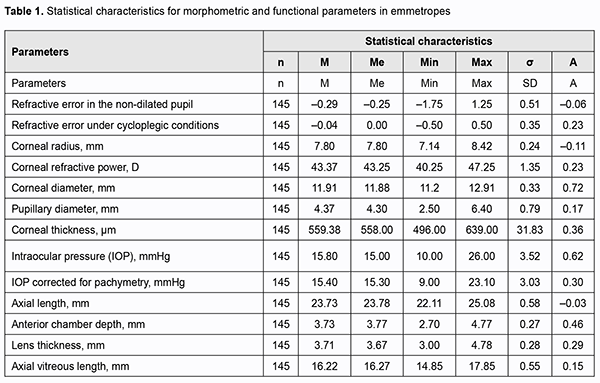
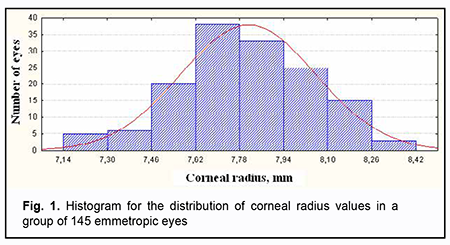
Fig. 1 shows the histogram of the distribution of corneal radius among the group of emmetropes, with a mean value of 7.80 ± 0.24 mm. Fig. 2 shows the histogram of the distribution of CRP among the group of emmetropes, with a mean value of 43.37 ± 1.35 D. In this study, mean corneal radius and median corneal radius values for emmetropes were equal (Me = 7.80 mm) (Table 1 and Fig. 1). Corneal radius was shorter (М ± SD = 7.72 ± 0.27 mm vs 7.72 ± 0.27 mm) and the cornea was significantly steeper (t = 3.43; p<0.01) in myopes than in emmetropes.
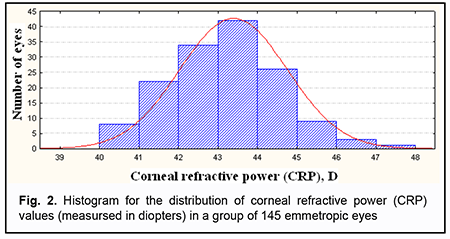
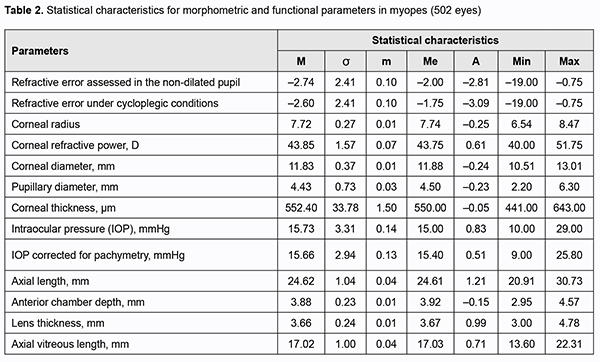
Statistical characteristics of the distributions of ocular biometric parameters for myopes were obtained, and, on this basis, the features of distributions of ocular biometric parameters, axial length (AL) and corneal refractive power (CRP), were found. Table 2 shows statistical parameters (mean, standard deviation, median, maximum, minimum and skewness) for functional characteristics of ocular structures for 502 myopic eyes. CRP was 43.87±1.57 D, with a median value of 43.7 D (Fig. 3), and minimum and maximum values of 40.0 D and 51.75 D, respectively (Table 2), for 502 myopic eyes. In addition, CRP skewness was larger in myopes than in emmetropes (0.61 versus 0.23; Table 2 and Table 1, respectively).
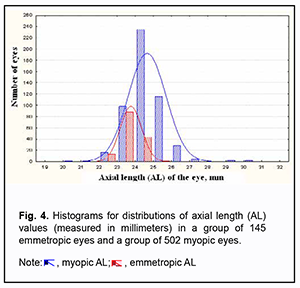
For the sample of myopic eyes, the distribution of CRP was moderately skewed, with larger skewedness and median values (0.61 and 43.75 D, respectively), than for the sample of emmetropic eyes (0.23 and 43.37 D, respectively). Mean CRP values for the samples of myopic eyes (502 eyes) and emmetropic eyes (145 eyes) were 43.86 ± 1.58 D and 43.37±1.35 D, respectively. In addition, mean corneal refractive power was statistically significantly (t =3.63; p < 0.01), by 0.49 D, larger, and the difference between mean and median CRP values was smaller, for myopic eyes than for emmetropic eyes. There was a symmetric distribution of AL values for emmetropes (Fig. 4), but not for myopes. Thus, the skewness for emmetropes was (–0.03) (Table 1, Fig. 4), and 1.21 for myopes (Table 2). The AL ranged from 22.11 mm to 25.08 mm (Table 1) for emmetropes, and from 20.91 mm to 30.73 mm (Table 2) for myopes.
Discussion The fact that corneal curvature and refractive power myopic are greater in myopic eyes than in emmetropic eyes [13, 15, 22] was confirmed in our study, and could distinguish really steep corneas with greater curvature from others. This allows distinguishing the refractive component that can affect the development of myopic refractive error. In view of the foregoing, a mean CRP value of 43.86 D for myopes (with a significant difference from that for emmetropes; t = 3.63; p < 0.01) was chosen as a cut-off value in order to segregate myopia with a refractive component (patients with a CRP ≥ 43.86 D, which corresponds to CRP > 43.75 D, taking in account a measurement increment of 0.25 D for the autorefractokeratometer) and myopia without a refractive component (patients with a CRP ≤ 43.75 D). The latter patients will not have a refractive component affecting the development of myopic refraction, because CRP values in this group will be normally distributed, and will be close to those for emmetropes. It was found that, for emmetropes, the AL value will be within a range of mean AL ± SD (23.7 ± 0.6 mm; i.e., 23.1 mm to 24.3 mm), with a spread from 22.11 mm to 25.08 mm (Table 1). These findings are in agreement with those of Rykov’s fundamental study [23] on ocular morphometric parameters, who demonstrated that, for emmetropes, the distribution of AL had a maximum around 22.5-23.5 mm. In the current study, 85% of emmetropes had an AL of less or equal to 24.3 mm. Since AL values greater than 24.3 mm were found to be uncommon in emmetropes, an AL value of 24.3 mm was chosen as a cut-off value in order to segregate myopia with an axial component and myopia without an axial component. This is in agreement with the opinion of Zhou and colleagues, who believe that axial myopia occurs if the length of the eyeball is more than the average length of about 24 mm [24]. In the current study, we found that the mean AL for 502 myopic eyes was 24.62 mm, which was close to the values found by others. In a study by Park and colleagues [25], the mean AL for myopic patients aged 29 to 95 years (41.56 ± 15.70 years) was 24.35 ± 1.49 mm. In view of the foregoing, an AL value of 24.3 mm and a CRP value of 43.86 D that we propose to use as cut-off values for distinguishing axial, refractive, mixed and combinatory myopias, are objective and quite contrary to those proposed earlier by Tron [21]. This allows proposing a modified classification scheme for types of myopia based on CRP and AL parameters characterizing refractive and axial components, respectively [26]. This modified classification scheme distinguishes among refractive myopia (AL ≤ 24.3 mm and CRP > 43.86 D), axial myopia (AL > 24.3 mm and CRP ≤ 43.86 D), mixed myopia (AL > 24.3 mm and CRP > 43.86 D), and combinatory myopia (AL ≤ 24.3 mm and CRP ≤ 43.86 D, similar to emmetropes) [27, 28]. Tron [21] proposed an AL value of 22.4 mm to 27.3 mm and a CRP value of 52.59 D to 64.21 D as cut-off values for distinguishing various types of myopia, e.g., axial myopia (AL > 27.3 mm and CRP of 52.59 D to 64.21 D) and refractive myopia (an “emmetropic” AL of 22.4 mm to 27.3 mm and a CRP value greater than 64.21 D, a maximum for emmetropes). Tron [21 proposed to use extreme emmetropic values of AL (22.4 mm and 27.3 mm) and ocular refractive power (ORP; 52.59 D and 64.21 D) as cut-off values for distinguishing various types of myopia, e.g., axial myopia (AL > 27.3 mm and ORP of 52.59 D to 64.21 D), with the ORP value being equal to the sum of the CRP value and lens refractive power (LRP) value, and refractive myopia (an “emmetropic” AL of 22.4 mm to 27.3 mm and a CRP value greater than 64.21 D, a maximum for emmetropes). A clinical example from Torn [21] is given below. For patient No.253, CRP = 48.34 D, LRP = 48.34 D, AL = 26.42 mm, refractive error = -12.0 D. The patient was classified by Torn as a refractive myope. We believe that the patient could not be classified as a refractive myope, because both the refractive component (CRP = 48.34 D) and the axial component [26] (AL = 26.42 mm) are involved in the development of this myopia. Based on the classification criteria proposed by us, the patient should be classified as a mixed myope [27]. In addition, Torn classified the following two cases as mixed myopes: patient No. 168 (CRP = 46.35 D, LRP = 22.52 D, AL = 22.29 mm, refractive error = -15.0 D) and patient No. 268 (CRP = 48.98 D, LRP = 19.95 D, AL = 27.57 mm, refractive error = -15.0 D). It is well seen from the above two cases that a difference in the magnitude of AL was as large as 5.28 mm (for axial lengths of 22.29 D and 27.57 mm), and a difference in the magnitude of refractive error was as large as 14.5 D (for refractive errors of -0.5 D and -15.0 D), although a corneal refractive power value was high for both cases (46.35 D and 48.98 D). As opposed to Tron, we used classification criteria proposed by us and classified patient No. 168 (CRP = 46.35 D, AL = 22.29 mm) as a refractive myope, because in this case, the AL value corresponds to those related to emmetropes and even hypermetropes, and the refractive component is involved in the development of this myopia [26]. We, however, believe that patient No.268 from a study by Tron indeed could be classified as a mixed myope, with the involvement of both the axial and refractive components resulting in a high myopic refractive error of -15 D. It means that there were substantial differences between the above two cases from a study by Tron with regard to fundus changes, state of the ocular shells, prognosis for the course of myopia and potential for sequelae. Consequently, patient No. 168 could not be classified as the same type of myopia as patient No. 268. These example cases demonstrate shortcomings of the previous criteria for distinguishing among axial, refractive, mixed and combinatory myopias, and the need for applying the new approach to diagnosing these types of myopia. Therefore, the newly developed objective criteria allow for establishing the type of myopia corresponding to axial and refractive components on the basis of corneal refractive power and axial length of the eye. These criteria fundamentally change the approach to distinguishing among axial, refractive, mixed and combinatory myopias. The proposed modified classification of the types of myopia takes in account the axial and refractive components and allows for distinguishing practically among refractive myopia (AL ≤ 24.3 mm and CRP > 43.86 D), axial myopia (AL > 24.3 mm and CRP ≤ 43.86 D), mixed myopia (AL > 24.3 mm and CRP > 43.86 D), and combinatory myopia (AL ≤ 24.3 mm and CRP ≤ 43.86 D, similar to emmetropes). Differential diagnosis among these types of myopia will allow a clinician to anticipate the course of the disease, changes in the ocular shells and fundus, risk of sequelae, and to take appropriate measures for stabilization of myopia promptly.
References 1.Lin LLK, Shih YF, Tsai CB, et al. Epidemiological study of ocular refractions among school–children (aged 6 through 18) in Taiwan. ARVO Abstract. Invest Ophthalmol Vis Sci. 1996;37:S1002. 2.Parssinen O. The increased prevalence of myopia in Finland. Acta Ophthalmol. 2012; 90: 497-502. 3.Parssinen O, Lyyra AL. Myopia and myopic progression among schoolchildren: a three–year follow–up study. Invest Ophthalmol Vis Sci. 1993 Aug;34(9):2794-802. 4.Vitale S, Sperduto RD, Ferris FL 3rd. Increased prevalence of myopia in the United States between 1971-1972 and 1999-2004. Arch Ophthalmol. 2009 Dec;127(12):1632-9. 5.Khoo CY, NG RFS. Methodologies for Interventional Myopia Studies. Ann Acad Med Singap. 2006 Apr;35(4):282-6. 6.Sperduto RD, Seigel D, Roberts J, Rowland M. Prevalence of myopia in the United States. Arch Ophthalmol. 1983 Mar;101(3):405-7. 7.Dobrovolskiĭ VN. [On the question of the causes of myopia]. Iezhenedelnaia klinicheskaia gazeta. 1885;1:13–6. Russian. 8.Strang NC, Winn B, Gilmartin B. Repeatability of post–task regression of accommodation in emmetropia and late–onset myopia. Ophthal Physiol Opt. 1994 Jan;14(1):88-91. 9.Tarutta EP. [Capabilities for preventing progressive and complicated myopia in view of the current knowledge about its pathogenesis]. Proceedings of the 8th Congress of Russian ophthalmologists. Moscow; 2005. p. 712–3. Russian. 10.Zadnik K, Mutti DO, Fusaro RE, Adams AJ. Longitudinal evidence of crystalline lens thinning in children. Invest Ophthalmol Vis Sci. 1995 Jul;36(8):1581-7. 11.Avetisov ES. [Myopia as a manifestation of the body's adaptive response]. In: Proceedings of the 2nd Russian Congress of Ophthalmologists. Moscow; 1968. p.363–73. Russian. 12.Dashevskiĭ AI. [Myopia]. Leningrad: Medgiz; 1962. Russian. 13.Fledelius HC, Goldschmidt E. Oculometry findings in high myopia at adult age: considerations based on oculometric follow-up data over 28 years in a cohort-based Danish high-myopia series. Acta Ophthalmol. 2010 Jun;88(4):472-8. 14.Martin R, Ortiz S, Rio–Cristobal A. White–to–white corneal diameter differences in moderately and highly myopic eyes: partial coherence interferometry versus scanning–slit topography. J Cataract Refract Surg. 2013 Apr;39(4):585–9. 15.Grosvenor T, Goss DA. Role of the cornea in emmetropia and myopia. Optom Vis Sci. Optom Vis Sci. 1998 Feb;75(2):132–45. 16.Schmid K. Myopia Manual. An impartial documentation of all the reasons, therapies and recommendations. Available at: http://www.myopia-manual.de/private/manual-2021-jan.pdf. 17.Ludwig CA, Shields RA, Chen TA, et al. A novel classification of high myopia into anterior and posterior pathologic subtypes. Graefes Arch Clin Exp Ophthalmol. 2018 Oct;256(10):1847-56. 18.Avetisov ES. [Myopia]. Moscow: Meditsina; 1986. Russian. 19.Bushuieva NN. [Modern aspects of etiology, pathogenesis and surgical treatment of progressive myopia]. Oftalmol Zh. 2006;3(1):65–70. Russian. 20.Bystritskiĭ VI. [On the treatment of accommodation spasms and some issues of the pathogenesis of axial progressive myopia]. Ofalmol Zh. 1991;1:28–31. Russian. 21.Thron EZh. [Variability of the components of the optical system of the eye and its clinical importance]. Leningrad: Voienno-meditsinskaia akademiia;1947. Russian. 22.Maliieva OV. [The morphometric indicators of optical environments in patients with myopia, taking into account age and degree of myopia]. Tavricheskii mediko- biologicheskii vestnik. 2012;3(15):85-90. 23.Rykov SA. [The eye as a system. Structure. Function. Relationship]. Kyiv: Medekol;2000. Russian. 24.Zhou XD, Wang FR, Zhou SZ, Shi JS. A computed tomographic study of the relation between ocular axial biometry and refraction. In: Myopia Updates: Proceedings of the 6th international conference on myopia. Editor, Tokoro T. New York, 1998. p.112–5. 25.Park SH, Park KH, Kim JM, Choi CY. Relation between Axial Length and Ocular Parameters. Ophthalmologica. 2010;224(3):188-93. 26.Maliieva OV, Bushuieva NM. Pat. of Ukraine №9,137,183,299. IPC (2014.01): A61F 9/00. [A method for diagnosing myopia progression]. No. u 2014 04603; 06/25/2014. Bul No 12. Ukrainian. 27.Maliieva OV, Bushuyeva NM. Pat. of Ukraine № 83,299 Ukraine. IPC (2013.01): A61F 9/00. [Methods for identifying patients with signs of axial, refractive, mixed or combinatory myopia]. No. u 2013 0837 08/27/2013. Bul No 16. Ukrainian. 28.Fledelius H.C. Is myopia getting more frequent? Across–sectional study of 1416 Danes aged 16 years +. Acta Ophthalmol (Copenh). 1983;61:545–9.
The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
|