J.ophthalmol.(Ukraine).2021;2:3-9.
|
http://doi.org/10.31288/oftalmolzh2021239 Received: 01 December 2020; Published on-line: 19 April 2021 Conjunctival cytology in patients treated for ocular infectious diseases Sh. A. Dzhamalova, N. R. Yangieva, Z. Kh. Kuryazova Tashkent State Dentistry Institute; Tashkent (Uzbekistan) E-mail: shirinkon@mail.ru TO CITE THIS ARTICLE: Dzhamalova ShA, Yangieva NR, Kuryazova ZKh. Conjunctival cytology in patients treated for ocular infectious diseases. J.ophthalmol.(Ukraine).2021;2:3-9.http://doi.org/10.31288/oftalmolzh2021239 Background: Anti-inflammatory therapy is a mainstay of treatment for patients with ocular inflammatory disorders. Although glucocorticosteroids (GCS) demonstrate a potent anti-inflammatory and anti-allergic effect, treatment with GCS is associated with a risk of serious side effects. Non-steroidal anti-inflammatory agents (NSAIDs) possess somewhat lower anti-inflammatory activity compared to GCS, and their development and incorporation into clinical eye care practice seem reasonable. Purpose: To assess the efficacy of a 0.5% benzketosone ointment, a novel topical ocular medication manufactured in Uzbekistan, in the treatment of infectious conjunctivitis and blepharitis. Material and Methods: One hundred and thirty-one patients (175 eyes; 64 men and 67 women) were included in this study to assess the efficacy of treatment with 0.5% benzketosone ointment (Certificate №06-07) for ocular inflammatory disorders. Patients of the control group received the conventional therapy, whereas those of the experimental group received 0.5% benzketosone ointment in addition to the conventional therapy. A modified impression cytology technique was used to monitor the therapeutic effect. Results: Modified impression cytology showed that the incorporation of benzketosone ointment in the conventional treatment for conjunctivitis or blepharitis resulted in a substantial decrease in exudation and cell proliferation, which was manifested by a decrease in numbers of basophils and eosinophils, restoration of epithelial cell structure and earlier normalization of mean nucleocytoplasmic ratio values and earlier reduction in tissue and protein detritus in conjunctival specimens of the experimental group compared to controls. Conclusion: Modified impression cytology provided evidence that the incorporation of benzketosone ointment in the conventional treatment for conjunctivitis or blepharitis improved regenerative activity, metabolic processes and symptoms of ocular inflammation. Keywords: non-steroidal anti-inflammatory agents, conjunctivitis and blepharitis, conjunctival impression cytology
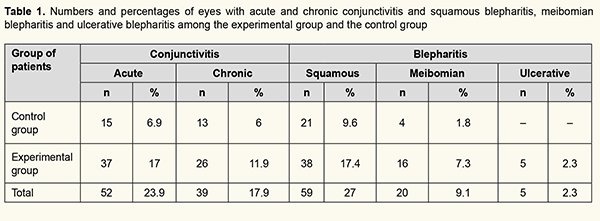
Introduction Ocular inflammatory disorders are common eye diseases, mostly of infectious nature, and, in particular, cause red eye syndrome [1, 2]. It has been reported [3-5] that, among patients with ocular inflammatory disorders, conjunctivitis was the most common (66.7%), followed by blepharitis (23.3%), whereas corneal inflammatory disorders (4.2%) and intraocular inflammatory disorders like uveitis, chorioretinitis, and neuritis (5.8%) were less common, but it is these disorders that are a common cause of visual loss and blindness. Among the eye patients registered in Uzbekistan during 2007-2011 years, 20% were those with ocular inflammatory disorders, with conjunctivitis being the most common (42%), followed by blepharoconjunctivitis (40%), chalazia and hordeola (8%), blepharitis (5%) and keratitis, episcleritis, uveitis and chorioretinitis (5%) [6]. Anti-inflammatory therapy is a mainstay of treatment for patients with ocular inflammatory disorders [7-11], with the anti-inflammatory medications being targeted primarily on the prevention of and reduction in the release of inflammatory mediators. Glucocorticosteroids (GCS) and non-steroidal anti-inflammatory agents (NSAIDs) can exert impact on this process [12, 13]. Although GCS demonstrate a potent anti-inflammatory and anti-allergic effect, their application is associated with a risk of reduction in immune protection, and this is why they are not recommended for viral corneal (superficial keratitis with epithelial defects) and conjunctival disorders, mycobacterial and fungal ocular infections. Long-term treatment with GCS can result in elevated intraocular pressure (potentially leading to glaucoma), reduction in lens transparency (with the development of posterior subcapsular cataract), low wound healing rate and the development of secondary infection. Rarely, they may also cause scleromalacia and corneal ulcerations, leading to severe corneal scarring. Another disadvantage of GCS therapy is that, if improperly applied, it may disrupt the ocular inflammatory process without achieving complete recovery, and contribute to the transition of an acute condition to a chronic condition with frequent relapses. The development and incorporation of NSAIDs into clinical eye care practice seems reasonable because they possess somewhat lower anti-inflammatory activity compared to GCS and do not cause the GCS-specific side effects. The primary clinical value of NSAIDs is related to their non-specific anti-inflammatory activity which is combined with their antipyretic and analgetic effects. In addition, they are effective at all phases of inflammation. Particularly, NSAIDs: ● reduce capillary permeability, and, consequently, reduce exudative inflammation ● stabilize lysosomal membranes and reduce lysosomal enzyme secretion, thus reducing tissue alteration at the focus of inflammation ● have an impact on the synthesis and activity of inflammatory mediators and reduce the production of adenosine triphosphoric acid (ATP), a major source of energy for inflammatory reactions ● exert a cytostatic effect and thus inhibit proliferative processes and platelet aggregation. General NSAID therapy may have serious side effects such as erosions and ulcerative lesions of the gastrointestinal tract, changes in the central nervous system, blood, liver and kidneys. Topical NSAID therapy, however, has a low risk of side effects, and this risk is confined solely to allergic manifestations. As opposed to GCS, NSAIDs do not induce glaucoma or cataract, and do not potentiate infection. Although NSAIDs do not cause the GCS-specific side effects, they possess somewhat lower anti-inflammatory activity compared to GCS, and this is the reason why few of them are manufactured in the form of ocular pharmaceuticals [12, 13]. Laboratory, bacteriological and bacterial microscopy studies may be used to assess the efficacy of a new drug introduced as a component of treatment, but the diagnostic value of these studies may be reduced if they have been preceded by antibacterial treatment. Conjunctival scraping for cytologic or immune fluorescence assessment is commonly used, but it has limitations because it is considered traumatic and invasive (i.e., its application should be preceded by anesthesia and followed by the use of antiseptics) [14]. Some researchers consider impression cytology as an alternative, since this technique is effective in determining the etiology of disease. The advantages of the technique include the possibility to control the efficacy of treatment, introduce changes in treatment regimens and determine a final treatment outcome. In addition, it is easy to use and does not require topical anesthetics [15]. The following points are taken into account when using impression cytology: ● the presence and type of exudate (serous, fibrinous, purulent and hemorrhagic), pseudomembranes, cellular detritis, sticky and fibrin filaments, bacteria and mycelium ● the presence of a layer of the changed epithelium, including goblet cells ● change in nucleocytoplasmic ratio (NCR) ● the presence of dystrophic and necrotic epithelial cells (karyopyknosis, karyorrhexis, karyolysis, and fragmented nucleus) and keratinization ● the presence of pathological inclusions (cocci, initial or elementary bodies, viral bodies) in the nucleus or cytoplasm, hydropic degeneration of epithelial cells; ● the presence of inflammatory cells (neutrophils, eosinophils, basophils, plasma cells and histiocytes); ● the presence of multinucleate syncytial giant cells [16]. In addition, not only clinical signs but also the following signs obtained from impression cytology can demonstrate regress of the disease: restoration of the normal epithelial layer and goblet cell density, disappearance of intracellular inclusions and local reactive changes (individual desquamated epithelial cells and solitary white cells) [6, 16, 17]. Therefore, impression cytology has a clinical value for diagnosis of conjunctival inflammatory processes and makes the treatment procedure easier. The purpose of this study was to assess the efficacy of a 0.5% benzketosone ointment, a novel topical ocular medication manufactured in Uzbekistan, in the treatment of infectious conjunctivitis and blepharitis. Material and Methods One hundred and thirty-one patients (175 eyes; 64 men and 67 women) were included in this study to assess the efficacy of treatment with 0.5% benzketosone ointment (Certificate №06-07) for ocular inflammatory disorders. Patient age ranged from 16 to 82 years. All patients included in the study had been diagnosed with conjunctivitis or blepharitis based on bacterial culture (Table 1).
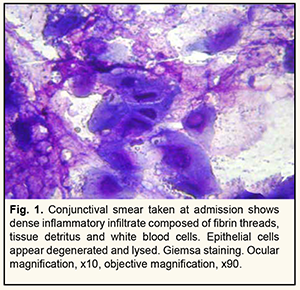
Patients with conjunctivitis (28 eyes) of the control group received conventional treatment for the disease: eye washing with a disinfectant solution (potassium permanganate KMnO4 or furacilin 1:5000), topical antibacterial drops (30% sodium sulfacetamide, 0.25% chloramphenicol) and 1% tetracycline ointment. Patients with conjunctivitis (63 eyes) of the experimental group received 0.5% benzketosone ointment instead of 1% tetracycline ointment. Patients with blepharitis (25 eyes) of the control group received the treatment similar to patients with conjunctivitis of this group after eyelid margin washing. Patients with blepharitis (59 eyes) of the experimental group received 0.5% benzketosone ointment instead of 1% tetracycline ointment. In addition, patients with meibomian blepharitis received eyelid massage followed by eyelid disinfection with alcohol and 1% brilliant green solution, whereas those with ulcerative blepharitis were treated with gauze soaked with antibiotic solution. A modified impression cytology technique was used to monitor the therapeutic effect. Briefly, the patient’s lower eyelid was retracted, the 0.8 µm-cellulose acetate filter membrane (Sartorius AG, Göttingen, Germany) gently placed in the conjunctival sac, and the lower eyelid carefully pressed against the globe. The filter was impressed upon the area of affected conjunctiva. The lower eyelid was retracted again, and the filter strip was carefully peeled off with sheets of bulbar and tarsal conjunctival epithelial cells adhering. The strips were then mounted on well-degreased glass slides. Cytologic smears were air dried and stained with May-Grunewald for 1-3 minutes. After being fixed, imprints were washed with distilled water, stained with Romanovsky-Giemsa for 20-30 minutes, washed with distilled water, and air dried. Cytological specimens were examined and their photographs were taken in an Opton light photo-microscope III (Oberkochen, Germany) at an ocular magnification of x10 and objective magnification of x90. Samples were collected at days 3, 7 and 10 of treatment. Microsoft Excel 7.0 software was used for statistical analyses. The Student's t-test was used to compare the means between two groups. The level of significance p ≤ 0.05 was assumed. Results Conjunctival swabs were collected for culture before treatment to verify the bacterial origin of the disease. Staphylococcus haemolyticus was the most common isolated organism (23.9%), followed by Staphylococcus epidermidis (17.2%) and Staphylococcus aureus (16.4%). Two or more organisms were isolated from 42% of samples. Most commonly, these were combinations of Staphylococci (including Staphylococcus pyogenes), diphtheroids, micrococci, and Candida, and rarely, E. Coli. Our findings are in agreement with those reported by Vorontsova and colleagues [18]. In their study of patients with chronic conjunctivitis, a single organism was found in 75%, and two or more organisms were isolated from 25% of samples. In addition, Staphylococcus epidermidis was isolated from 40%, S. aureus, from 10%, S. viridians and other Gram-positive opportunistic organisms, from 3%, and Gram-negative opportunistic organisms, from 5% of samples. In the first days of the study, morphological signs of inflammation prevailed in cytological specimens collected from patients with conjunctivitis and those with blepharitis from both groups. It was not uncommon that specimens exhibited a large amount of slimy protein aggregates, fibrin threads and tissue detritus (Fig. 1).
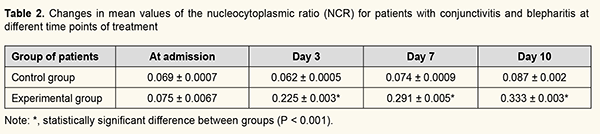
Inflammatory infiltrates were rich in fibrin filaments and protein clumps with contracted or destroyed epithelial cells in between them. Polynuclear white cells included basophils and eosinophils with signs of active degranulation; they densely surrounded epithelial cells and detritus with microorganisms, which also indicated the prevalence of alteration and exudation. Polymorphic changes were noted in conjunctival epithelial cells. The nuclei appeared increased in size and hyperchromatic, and some of the cells had a nucleolus. The cytoplasm showed degenerative and dystrophic changes manifested by eosinophil inclusions and vacuolization of the peripheral cytoplasm. Multinucleate symplasts were observed. At this time point, the mean nucleocytoplasmic ratio (NCR) was 0.069, which was significantly lower than a normal value of 0.2 (Table 2).
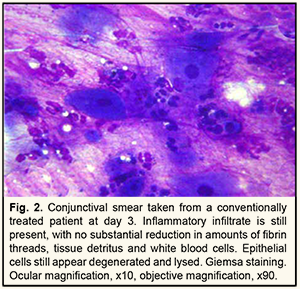
There was a substantial difference in subsequent changes in the conjunctival surface over time between those patients whose treatment included tetracycline ointment and those whose treatment included benzketosone ointment. At day 3, morphological signs of inflammation were still present in patients of the control group. Particularly, there was no substantial decrease in the amount of detritus or fibrin filaments. Epithelial cells mostly appeared contracted or destroyed. The cytoplasm still showed eosinophil inclusions and vacuolization. The nuclei still appeared hyperchromatic and had a nucleolus. At this time point, the mean NCR was still low (0.069; Fig. 2).
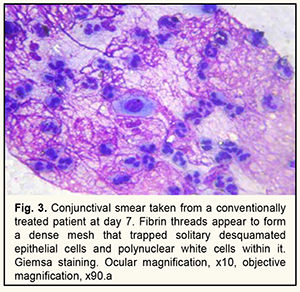
At day 7, conjunctival smears exhibited numerous fibrin threads and protein clumps. These threads appeared to form a dense mesh (Fig. 3) that trapped solitary desquamated epithelial cells and polynuclear white cells within it. At this time point, the mean NCR was 0.074.
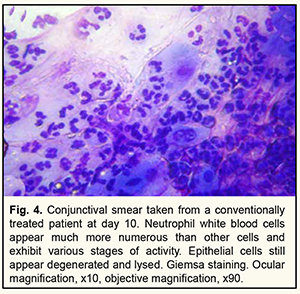
At day 10, neutrophil white blood cells were much more numerous than other cells (Fig. 4) in conjunctival smears and exhibited various stages of activity (cells were segmented, rod-shaped or bean-shaped). They appeared to densely surround desquamated epithelial cells which showed degenerative changes and destruction. Among epithelial cells, there were binucleate and multinucleate symplasts whose cytoplasm appeared increased in volume due to vacuolation and clearing. In addition, the mean NCR was 0.087, which was still significantly less than a normal value, and 1.2 times less that at the previous time point.
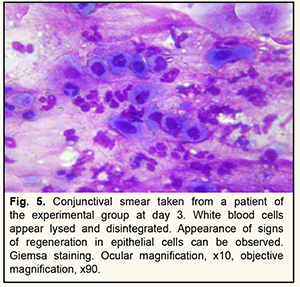
At day 3, patients treated particularly with benzketosone ointment for conjunctivitis or blepharitis showed reduced activity of alteration processes and inflammatory exudation. This was morphologically manifested by decreased amounts of inflammatory slimy and fibrin masses, and the destroyed white cells appearing as eosin-stained masses of irregular form. The epithelial cells exhibited less pronounced degenerative changes, and their nuclei appeared somewhat hypertrophic and hyperchromatic (Fig. 5).
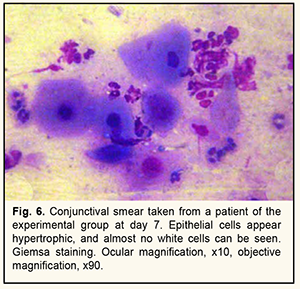
From the very first days of treatment, there was an increase in the mean NCR in the conjunctival smears taken from the experimental group; particularly, at day 3, the mean NCR was 0.225, which was close to a normal value of 0.2. By day 7 of the treatment, there was almost no evidence of inflammation in the cytologic specimens. There were only solitary white cells and lymphocytes appeared lysed (Fig. 6). Among epithelial cells, reparatory and regenerative processes were more common than degenerative processes; the mean NCR was 0.291, which was 1.5 higher than a normal value, and 3.9 times higher than the value for the control group at this time point.
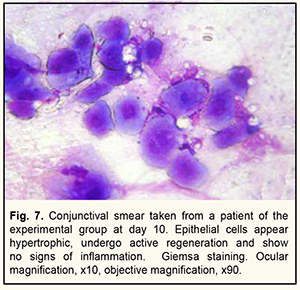
At day 10, only layers of the epithelial cells with signs of hypertrophy and hyperchromacy (Fig. 7) were seen in the conjunctival samples taken from patients of the experimental group. The cytoplasm of these cells was homogeneously stained and showed no degenerative structural changes. The nuclei varied in size and staining intensity, and most of them were hypertrophic and hyperchromatic. The mean NCR was 0.33.
Therefore, our cytological study demonstrated that sticky protein aggregates, fibrin threads and detritus prevailed in the conjunctival samples taken from the patients treated conventionally for blepharitis and conjunctivitis from the first days of treatment. Occasionally, basophils and eosinophils with signs of active degranulation appeared in the inflammatory infiltrate composed of polynuclear white cells, which also indicated the prevalence of alteration and exudation. Polymorphic changes were noted in the conjunctival epithelial cells. The nuclei appeared increased in size and hyperchromatic, and some of the cells had a nucleolus. In addition, these cells showed cytoplasmic degenerative changes like eosinophilic cytoplasmic inclusions and vacuolization of the peripheral cytoplasm. Multinucleate symplasts appeared occasionally. Moreover, there was practically no change in the mean NCR at various time points of inflammatory disease compared to baseline. Discussion Therefore, patients who received particularly benzketosone ointment for conjunctivitis or blepharitis showed faster relief of inflammation than those treated conventionally, which is likely associated with the capacity of NSAIDs to arrest the synthesis of prostaglandins responsible for inflammation by inhibiting cyclooxygenase, a prostaglandin synthesis enzyme. Our findings are in agreement with those of the studies by Slonimskii and colleagues [12] and Razumova and Godzenko [13] who compared four NSAIDs (bromfenac, keterolac, diclofenac and indometacin) for treatment efficacy. They also explain the anti-inflammatory, antipyretic and analgetic effects of NSAIDs by their capacity to inhibit cyclooxygenase and thus disrupt prostaglandin synthesis. Impression cytology verified the mechanisms of action of benzketosone: ● the cytologic evidence of a reduction in the numbers of basophils in the course of inflammation and exudation indicated the suppression of ancient inflammatory mediators, histamine and serotonine ● the disappearance of white cells was caused by the inhibition of prostaglandins and leukotrienes by benzketosone ● the restoration of cytoplasmic and nuclear structure of epithelial cells and increase in mean NCR values was caused by their increased metabolic processes and increased regeneration activity. The reliability of impression cytology for the diagnosis of dry eye was confirmed in a study by Patraievskii and Trishkin [16] who compared the available diagnostic methods (biomicroscopy signs and subjective symptoms; fluorescein and lissamine green; Schirmer test and tear film breakup time (TBUT); and impression cytology) for this disease. They found that impression cytology provided more valuable data even for the diagnosis of mild dry eye compared to other techniques. Studies by Ianchenko [17] and Ieremenko and colleagues [15] demonstrated the value of impression cytology for studies of conjunctival morphology in patients with chronic ocular ischemic syndrome and dry eye. Therefore, modified impression cytology showed that the incorporation of benzketosone ointment in the conventional treatment for conjunctivitis or blepharitis resulted in a substantial decrease in exudation and cell proliferation, which was manifested by a decrease in numbers of basophils and eosinophils and restoration of epithelial cell structure. This was confirmed by earlier normalization of mean NCR values and earlier reduction in tissue and protein detritis in conjunctival specimens of the experimental group compared to controls. Therefore, modified impression cytology enabled assessment of the efficacy of a 0.5% benzketosone ointment, a novel topical ocular medication manufactured in Uzbekistan, in the treatment of infectious conjunctivitis and blepharitis. The incorporation of benzketosone ointment in the conventional treatment for conjunctivitis or blepharitis improved regenerative activity, metabolic processes and symptoms of ocular inflammation, which was confirmed by cytologic evidence of an improvement in the morphology of conjunctival cells.
References 1.Dovgan’ EV. [Topical antimicrobial agents in ophthalmology: a review]. Ophthalmology in Russia. 2014;11(2):10-8. Russian. 2.Maichuk DIu. [Infectious ocular surface disorders (conjunctivitis and keratitis)]. In: [Maichuk DIu, editor. Red eye syndrome]. Moscow: Media Sfera; 2010. Russian. 3.Maichuk IuF. [Current medication therapy for conjunctivitis: a guide for physicians]. Moscow; 2013. Russian. 4.Neroev VV. [Guidelines for further development of the eye care service in the Russian Federation]. In: [Proceedings of the 9th Russian Ophthalmology Congress]. Moscow; 2010. p. 52-55. Russian. 5.Neroev VV, Maichuk IuF. [Diseases of the conjunctiva]. In: [Short National Guidelines on Eye Disease Management]. Moscow; 2014. p. 367-407. Russian. 6.Sidikov ZU. [Achievements and problems of the eye care service in the Republic of Uzbekistan]. Organizaziia i upravleniie zdravookhraneniiem. Tashkent. 2012;10:41-50. Russian. 7.Maichuk IuF. [Current therapeutic potential toward conjunctivitis]. In: [Proceedings of the 17th Russian National Congress on “Man and medications”]. 12-16 April, 2010. Moscow. p.215-225. Russian. 8.Maichuk IuF, Iani EV. [Novel approaches to the treatment of blepharitis]. Kataraktalnaia i refraktsionnaia khirurgiia. 2012;12(1):59-62. Russian. 9.Behrens-Baumann W. Topical antimycotic drugs. In: Kramer A, Behrens-Baumann W, editors. Antiseptic prophylaxis and therapy in ocular infections. Karger; 2002. p.263–80. Crossref PubMed 10.Larcombe J. Review: antibiotic therapy leads to slightly earlier recovery in acute bacterial conjunctivitis. Evid Based Med. 2006 Dec;11(6):180. 11.Kaercher T, Buchholz P, Kimmich F. Treatment of patients with keratoconjunctivitis sicca with OPtive: results of a multicenter, open-label observational study in Germany. Clin Ophthalmol. 2009;3:33–9. Crossref PubMed 12.Slonimskii AIu, Slonimskii IuB, Obrubov AS. [A novel non-steroidal anti-inflammatory agent for the treatment of various eye disorders]. Ophthalmology in Russia. 2016;13(1):33-7. Russian. https://doi: 10.18008 / 1816 5095 2016-33-37. 13.Razumova IIu, Godzenko AA. [Non-steroidal anti-inflammatory agent for the treatment of anterior uveitis associated with spondyloarthritis]. 2020;5(136):70-7. Russian. 14.Astakhov IuS, Riks IA. [Current methods for the diagnosis and treatment of conjunctivitis]. St Petersburg: Pavlov Medical University; 2007. Russian. 15.Eremenko AI, Ianchenko SV, Kiseliov AV. [Modified impression cytology for patients with dry eye secondary to topical ophthalmic preservatives]. Kubanskii nauchnyi meditsinskii vestnik. 2009;9(114):48-50. Russian. 16.Petraievskii AV, Trishkin KS. [Clinical and cytological diagnosis of dey eye]. Vestnik VolgGMU. 2012;4(44):52-4. Russian. 17.Ianchenko SV. [Modified impression cytology for patients with dry eye associated with chronic ocular ischemic syndrome]. Vestnik novykh meditsinskikh tekhnologii. 2009;16(1):149. Russian. 18.Vorontsova TN, Brzheskiy VV, Mikhailova MV. [Microflora of conjunctiva in children and its sensitivity and resistance to antibacterial drugs]. Ophthalmology in Russia. 2012;9(1):10-8. Russian. https://doi.org/10.18008/1816-5095-2012-1-83-91. Conflict of interests: All authors declare no conflict of interests.
|