J.ophthalmol.(Ukraine).2021;2:69-71.
|
http://doi.org/10.31288/oftalmolzh202126971 Received: 03 December 2020; Published on-line: 19 April 2021 COVID-19-associated cavernous sinus thrombosis: a case report O. I. Oripov, E. N. Bilalov Tashkent Medical Academy; Tashkent (Uzbekistan) E-mail: okil.oripov@mail.ru TO CITE THIS ARTICLE: Oripov OI, Bilalov EN. COVID-19-associated cavernous sinus thrombosis: a case report. J.ophthalmol.(Ukraine).2021;2:69-71. http://doi.org/10.31288/oftalmolzh202126971 This paper describes a case of cavernous sinus thrombosis. The condition developed in a patient who had been treated for confirmed COVID-19. Left eye examination findings were as follows: amaurosis; absence of periorbital skin sensation; signs of orbital cellulitis; ptosis; chemosis; total ophthalmoplegia; exophthalmos; decreased corneal sensation; widened pupil; and absence of pupil light reflex. In addition, ophthalmoscopy showed diffused retinal and optic disc edema. The patient had an atypical clinical course which could not be clearly identified as septic or aseptic, and his elevated D-dimer level could indicate a potential relationship between this condition and COVID-19. Keywords: COVID-19; ocular symptoms of COVID-19; COVID-19-associated coagulopathy; cavernous sinus thrombosis
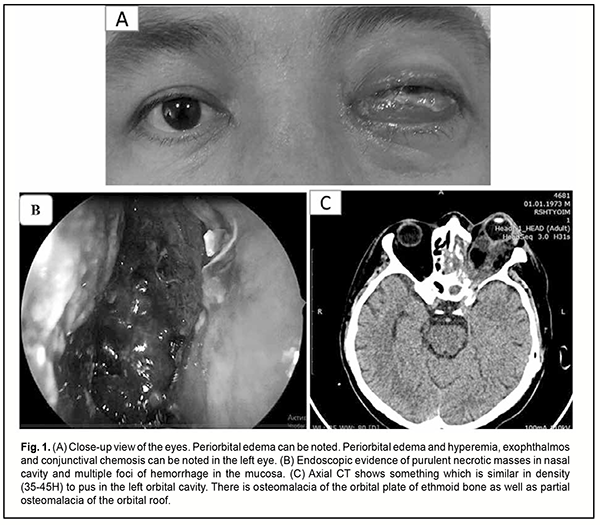
Introduction It has been demonstrated that patients with a severe course of COVID-19 tend to develop thromboembolic complications [1, 2]. Cavernous sinus thrombosis (CST) is one of the most dangerous disorders of the venous system of the brain with involvement of the visual pathway. The disease is usually caused by infection of the oral and nasal cavities, maxillary and frontal sinuses, and facial soft tissue, as well as by septic processes in a body weakened by chronic disorders [3, 4, 5]. In the Republic of Uzbekistan, the rate of CST among former COVID-19 patients has unprecedentedly increased, with almost 300 such cases registered by November 2020 [6]. Hereby we report a case of severe CST associated with COVID-19. Case report A male patient presented to the Multifield Clinic of Tashkent Medical Academy with complaints of severe pain in the left face, loss of sight, purulent nasal discharge, shortness of breath, cough, and weakness. His history was significant for years of type 2 diabetes mellitus. In addition, the patient received treatment for COVID-19 in July, 2020. Ten days after discharge from the in-patient setting, he started noting swollen eyelids, blepharoptosis and vision loss in the left eye, severe headache and nausea, and was hospitalized for these symptoms. The patient reported that he gradually started noting blepharoptosis and vision loss in the left eye after he initially experienced shortness of breath through the nose. Subsequently, these symptoms were accompanied by severe headache. The patient was diagnosed with meningoencephalitis of the frontal lobes. As he had a history of COVID-19, exhibited frontal lobe abscesses, hemorrhage into a right frontal lobe abscess cavity, and retrobulbar abscess, and had pansinusitis, cavernous sinus thrombosis, type 2 diabetes mellitus, and left interstitial pneumonia, he underwent “emptying and draining frontal lobe abscesses through trephine openings made one on each side of the head under local anesthesia”. Following this procedure, the patient experienced some improvement, with clarified consciousness and a reduction in body temperature. After he was consulted by neurosurgery, it was decided to continue his treatment under the supervision of maxillofacial surgeons and ophthalmologists. On examination, his general condition was bad, body temperature was 37.8 °C, skin and mucous membranes were pale; the respiration was vesicular; no rales; respiration rate, 24/min; blood pressure, 120/80 mmHg; and heart rate, 89/min. The peripheral lymph nodes were enlarged. Left eye examination findings were as follows: pattern vision with left amaurosis; a swollen and hyperemic periorbital area; ophthalmoplegia; exophthalmos; conjunctival chemosis; transparent cornea; decreased corneal sensation; moderately deep anterior chamber; transparent aqueous humor; widened pupil; absence of pupil light reflex; and partial lens opacity. Detailed ophthalmoscopy was not possible (Fig. 1).
Figure 1 (B) shows a CT image of the patient. Axial CT shows something which is similar in density (35-45H) to pus in the left orbital cavity. There was osteomalacia of the orbital plate of ethmoid bone as well as partial osteomalacia of the orbital roof. In addition, purulent material in the maxillary sinus cavity and signs of frontal lobe encephalitis were seen. Laboratory test results included: C-reactive protein, 80 mg/L; Antistreptolysin O, 300 ul/ml; antineutrophil antibodies, 0.10; D-dimer, 1206 ng/ml; fibrinogen, 743 mg/dl; activated partial thromboplastin time, 32 sec; prothrombin index, 87%; prothrombin time, 16 sec; and international normalized ratio (in the presence of anticoagulation therapy), 1.35. The diagnosis was established based on the results of clinical and laboratory tests and imaging studies Major diagnosis: Cavernous sinus thrombosis and left chronic purulent pansinusitis in the acute phase. Complication: abscess in the orbital cavity. Concomitant diagnosis: Post-COVID-19 condition. Left interstitial pneumonia condition. Post-frontal lobe abscess drainage condition. Type 2 diabetes mellitus. An expert panel of related specialties decided that a functional endoscopic sinus surgery (FESS) with debridement and decompression of the orbit had to be conducted by a team of ophthalmologists, maxillofacial surgeons and otolaryngologists. Approximately 15-20 milliliters of purulent material were evacuated from the orbital cavity. Revision of the cavity confirmed purulent-and-necrotic melting of the orbital plate of ethmoid bone as well as a portion of the orbital roof. Subsequently, ethmoidotomy and maxillary sinusotomy and evacuation and drainage of purulent material were conducted. Postoperatively, the patient improved progressively in the presence of lavage of the cavities with antiseptic solutions and comprehensive systemic medical therapy. At day 5 after surgery, eye swelling improved, but amaurosis, and ophthalmoplegia were still present, and periorbital skin sensation was still absent. In addition, ophthalmoscopy showed diffused retinal and optic disc edema. Discussion The reviewed case of cavernous sinus thrombosis had an untypical clinical course. Cavernous sinus thrombosis cannot be clearly classified as aseptic or septic with regard to characteristics of changes and time points of changes in pathognomonic signs. On the one hand, there was a gradual increase in symptoms, which is characteristic for an aseptic course and was confirmed by coagulation tests. On the other hand, orbititomy demonstrated signs of orbital phlegmon, which result in the development of septic cavernous sinus thrombosis. It is, however, difficult to determine whether the development of unilateral purulent pansinusitis with involvement of the orbit preceded cavernous sinus thrombosis with a subsequent purulent-and-necrotic process in the sinuses or the latter preceded the former. The D-dimer level was five times higher than normal in our patient who had been taking platelet antiaggregants and indirect anticoagulants for years. This finding indicates that he could develop COVID-19-associated coagulopathy, likely a major factor leading to the above condition. In addition, of note that C-reactive protein and antistreptolysin O levels were substantially (13 times and 1.5 times, respectively) higher than normal; this may indicate that the patient had vasculitis. Conclusion We may conclude that we encountered an unusual course of cavernous sinus thrombosis which does not conform to the general regularities of the course of this pathologic condition. It is noteworthy that more than ten similar COVID-19-associated cases have been registered in the Republic of Uzbekistan during the recent five months. Therefore, further and more systemic research work on this issue is required to elucidate the role of COVID-19-associated coagulopathy and vasculitis in the development of thrombotic and purulent-and-necrotic processes in the maxillofacial area.
References 1.Al-Ani F, Chehade S., Lazo-Langner A. Thrombosis risk associated with COVID-19 infection. A scoping review. Thromb Res. 2020 Aug;192:152-60. 2.Panigada M, Bottino N, Tagliabue P, Grasselli G, Novembrino C, Chantarangkul V, at al. Hypercoagulability of COVID-19 patients in intensive care unit: a report of thromboelastography findings and other parameters of hemostasis. J Thromb Haemost. 2020;18(7):1738–42. 3.Al-Samkari H, Karp Leaf RS, Dzik WH, Carlson JC, Fogerty AE, Waheed A, et al. COVID and coagulation: bleeding and thrombotic manifestations of SARS-CoV2 infection. Blood. 2020 Jul 23;136(4):489-500. 4.Hughes C, Nichols T, Pike M, Subbe C, Elghenzai S. Cerebral venous sinus thrombosis as a presentation of COVID-19. Eur J Case Rep Intern Med. 2020 Apr 29;7(5):001691. 5.Silvis SM, Sousa DAD, Ferro JM, Coutinho JM. Cerebral venous thrombosis. Nat Rev Neurol. 2017 Sep;13(9):555-65. 6.Oripov OI, Bilalov EN, Umarov RZ. [COVID-19-associated cavernous sinus thrombosis]. Vestnik Tashkentskoi medicinskoi akademii (spetsial'nyi vypusk). 2020:34-42.
The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
|