J.ophthalmol.(Ukraine).2021;3:15-22.
|
http://doi.org/10.31288/oftalmolzh202131522 Received: 21 January 2021; Published on-line: 29 June 2021 Preoperative serum 25-hydroxycalciferol levels in Kherson-region patients with cataract only, cataract plus glaucoma or cataract plus high myopia N. S. Lutsenko 1, O. V. Krasnozhan 2, 3, N. F. Efimenko 1 1 SI “Zaporizhia Medical Academy of Post-Graduate Education Ministry of Health of Ukraine”; Zaporizhia (Ukraine) 2 Donetsk National Medical University; Liman (Ukraine) 2 KPP "Kherson City Clinical Hospital named after A. and O. Tropin"; Kherson (Ukraine) E-mail: oko.clinic@gmail.com TO CITE THIS ARTICLE:Lutsenko NS, Krasnozhan OV, Efimenko NF. Preoperative serum 25-hydroxycalciferol levels in Kherson-region patients with cataract only, cataract plus glaucoma or cataract plus high myopia. J.ophthalmol.(Ukraine).2021;3:15-22. http://doi.org/10.31288/oftalmolzh202131522 Background: The contribution of cataract to the total prevalence of eye disease in Ukraine increased from 14.7% in 2001 to 15.9% in 2011. Studies have shown that 15% to 76% of eyes with glaucoma have cataract. In addition, cataract associated with myopia is 45-fold more frequent than cataract associated with other refractive errors. Blood 25-hydroxycalciferol is a biologically active substance that reflects vitamin D levels in man. Vitamin D is a general term used to denote vitamin D2 (also called ergocalciferol) and vitamin D3 (also called cholecalciferol). 25-hydroxycalciferol plays a key role in the preservation of the structure of the connective tissue, regulation of inflammatory processes, and energy exchange in the body, but its role in patients with cataract only, cataract plus glaucoma or cataract plus high myopia, however, has been poorly studied. Purpose: To assess preoperative serum 25-hydroxycalciferol levels in Kherson-region patients with cataract only, cataract plus primary open-angle glaucoma (POAG) or cataract plus high myopia. Material and Methods: Immediately before they underwent cataract surgery during November 2017 to April 2018, 128 Kherson-region patients underwent assessment of their serum 25-hydroxycalciferol levels. Patients were divided into three disease groups depending on the presence of POAG or high myopia: group 1 (controls; cataract only; n = 38), group 2 (cataract plus POAG; n = 36) and group 3 (cataract plus high myopia; n = 54). Age groups and men and women within disease groups were assessed separately for serum 25-hydroxycalciferol levels. Serum samples were analyzed for 25-hydroxycalciferol using enzyme immunoassay (IDS, Germany). Results: Patients of all disease groups showed substantial deficiency in serum 25-hydroxycalciferol levels compared to a norm of 30 ng/ml or more. In each disease group, women showed lower serum 25-hydroxycalciferol levels than men, and the difference was significant for groups with cataract plus myopia (Р = 0.04) and cataract plus glaucoma (Р = 0.006), but not for the cataract-only group. Conclusion: We found low serum 25-hydroxycalciferol levels in all patients with age-related cataract, especially in those with concomitant high myopia or POAG. The study patients older than 75 years showed severely deficient serum 25-hydroxycalciferol levels, with no significant difference among study groups. Keywords: cataract, high myopia, 25-hydroxycalciferol Conflict of Interest Statement:The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
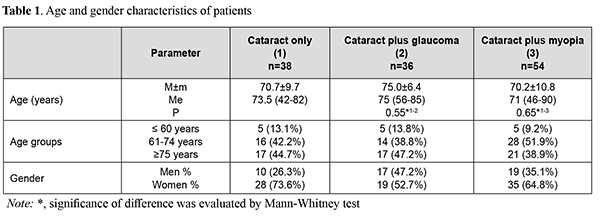
Introduction The contribution of cataract to the total prevalence of eye disease in Ukraine increased from 14.7% in 2001 to 15.9% in 2011 [1]. Studies have shown that 15 % to 76 % of eyes with glaucoma have cataract [2]. In addition, the association of cataract with myopia is 45-fold more frequent than that of cataract with other refractive errors [3-5]. There is much in common between the pathogenesis of glaucoma and myopia, and the role of genetic factors, metabolic and degenerative impairments in the development of either disease have been demonstrated [6-9]; this should be taken in account while approaching the surgical rehabilitation of a case of both cataract and one of the above eye disorders. Blood 25-hydroxycalciferol is a biologically active substance that reflects vitamin D levels in man. Vitamin D is a general term used to denote vitamin D2 (also called ergocholecalciferol) and vitamin D3 (also called cholecalciferol) [10]. 25-hydroxycalciferol plays a key role in the preservation of the structure of the connective tissue; regulation of inflammatory processes, neuromediator synthesis and nerve impulse transfer; and energy exchange in the body [11-13]. However, the role of 25-hydroxycalciferol in eye disease pathogenesis has been poorly studied. Isolated studies have reported the presence of vitamin D receptor in the ocular tissue (particularly, cells of the corneal endothelium and nonpigmented ciliary body epithelium and sclera fibroblasts) [14-16]. Studies have demonstrated changes in serum 25-hydroxycalciferol in patients with cataract, primary open-angle glaucoma (POAG), and myopia, and proposed that it plays a role in the pathogenesis of these disorders [13, 15, 17-27]. It is known that vitamin D is involved in immunomodulation in glaucoma, regulation of the synthesis of neurotrophic factors in the central nervous system, and regulation of oxidative stress in neurons through the activation of calcium channels [13, 18,19, 28, 29]. Up to date, the role of serum 25-hydroxycalciferol level in patients with cataract, however, has been poorly studied. In addition, assessment of serum 25-hydroxycalciferol levels in patients with both cataract and a common eye disease (POAG or myopia) is of scientific interest. These issues require detailed research and are dealt with in the current study. The purpose of this study was to assess preoperative serum 25-hydroxycalciferol levels in Kherson-region patients with cataract only, cataract plus POAG or cataract plus high myopia. Material and Methods Immediately before they underwent cataract surgery during November 2017 to April 2018, 128 Kherson-region patients underwent assessment of their serum 25-hydroxycalciferol levels. The period from late autumn to early spring (November to April) was selected to exclude the period of high insolation and obtain true values for serum 25-hydroxycalciferol levels in study patients. Patients were divided into three groups depending on the presence of POAG or high myopia: group 1 (controls; cataract only; n = 38), group 2 (cataract plus POAG; n = 36) and group 3 (cataract plus high myopia; n = 54). The presence of a spherical refractive error of at least 6.0 D and/or an eye of an axial length exceeding 24 mm was the criterion for inclusion in the group of high myopia. The presence of glaucoma compensated with topical hypotensive therapy was the criterion for inclusion in the group of POAG. Exclusion criteria were: terminal glaucoma, severe concomitant eye disease (retinal degenerative disease, uveitis, optic nerve atrophy, etc.), pseudoexfoliation syndrome, somatic disease (diabetes mellitus, bronchial asthma, autoimmune or rheumatoid disease, and cancer). The absence of these diseases was confirmed by somatic, somatic status assessment, and review of documentation in the medical record. Patients receiving dietary supplements containing calcium, 25-hydroxycalciferol and/or other pharmaceuticals for osteoporosis were also excluded. Study patients underwent a routine eye examination (visual acuity assessment, perimetry, biometry, tonometry, biomicroscopy, ophthalmoscopy, echobiometry, and keratorefractometry). Age groups and men and women within disease groups were assessed separately for serum 25-hydroxycalciferol levels. Three age groups were formed for analysis of serum 25-hydroxycalciferol levels based on the WHO classification: age group 1, patients younger than 60 years; age group 2, patients of 61 to 74 years; and age group 3, patients older than 75 years. The study followed the ethical standards stated in the Declaration of Helsinki, the European Convention on Human Rights and Biomedicine and relevant laws of Ukraine. Informed consent was obtained from all study subjects. The study protocol was approved by the Ethics Committee of Zaporizhzhia Medical Academy of Post-Graduate Education, Ministry of Health of Ukraine (Extract of the Minutes of the Committee No.10 of December 17, 2020). An overnight venous blood sample (10 mL) was obtained from an antecubital forearm vein into the vacutainer tube containing EDTA. Immediately thereafter, the sample was centrifuged, and the serum was separated, transferred to an Eppendorf tube, and frozen at -20º С until further analysis. Serum samples were analyzed for 25-hydroxycalciferol using enzyme immunoassay (IDS, Germany). Serum vitamin D levels were classified as adequate (>30 ng/ml), insufficient (20 to 30 ng/ml), moderate deficient (10 to 20 ng/ml) or severe deficient (<10 ng/ml). Statistical analyses were conducted using Statistica 10.0 (StatSoft, Tulsa, OK, USA) software. The Shapiro–Wilk test was used to test normality. The Mann-Whitney test was further used to compare two series of data, and Kruskal–Wallis test, to compare more than two series of data. Spearman correlation was used to assess the relationship between variational series. The level of significance p < 0.05 was assumed. Results We assessed serum 25-hydroxycalciferol levels for cataract-only, cataract plus POAG and cataract plus high myopia groups. Table 1 presents age and gender distribution among study subjects for these three groups.
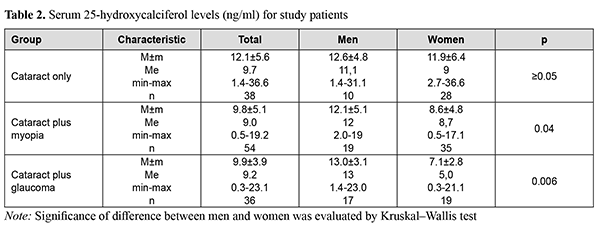
Table 2 presents mean serum 25-hydroxycalciferol levels for cataract-only, cataract plus POAG and cataract plus high myopia groups.
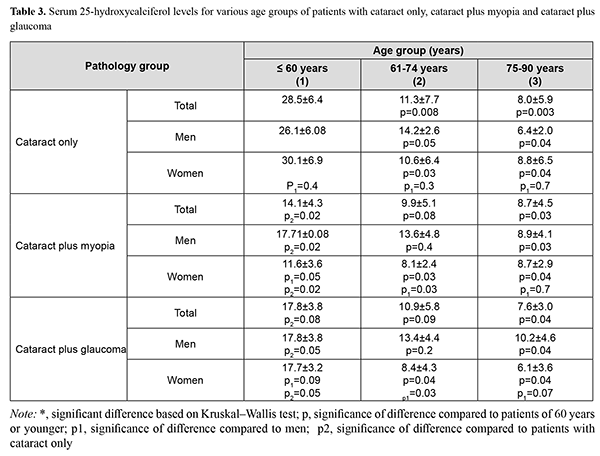
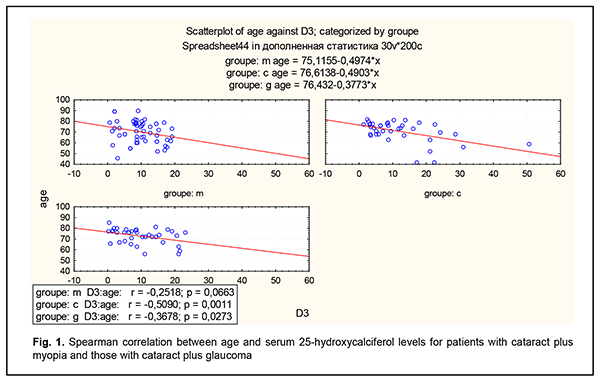
Patients of all the groups showed substantial deficiency in serum 25-hydroxycalciferol levels compared to a norm of 30 ng/ml or more. In each group, women showed lower serum 25-hydroxycalciferol levels than men, and the difference was significant for groups with cataract plus myopia (Р=0.04) and cataract plus glaucoma (Р=0.006), but not for the cataract-only group. Changes in serum 25-hydroxycalciferol levels with gender and age in patients with myopia and glaucoma are presented in Table 3. In each group, patients older than 75 years showed statistically significantly lower serum 25-hydroxycalciferol levels than the norm; in addition, serum 25-hydroxycalciferol level was negatively correlated with age (Fig. 1).
Discussion The role of vitamin D in cardiovascular diseases [25, 29] and ocular disorders like age-related macular degeneration [30], diabetic retinopathy [31], dry eye, etc. [15, 16, 21, 22, 24, 26, 27, 32] has been demonstrated. There have been controversial reports with regard to serum 25–hydroxyl vitamin D deficiency and age–related cataract [32]. Abdellah and colleagues [20] studied the relation between the serum 25-hydroxyl vitamin D (OH D) level and the occurrence of age-related cataract in a Egyptian case-control study. They found that 25-OH D levels in all enrolled individuals were below the reference levels with a severe deficiency in cataract patients. The current study enrolled the patients aged 40 to 90 years who were free from the diseases that could affect serum 25–hydroxyl vitamin D levels and did not receive vitamin D supplementation. We found marked 25-hydroxycalciferol deficiency in Kherson-region patients with cataract only, with a mean serum 25-hydroxycalciferol level of 12.1±5.6 ng/ml, which was higher than in a study by Abdellah and colleagues [20] (7.6 ± 5.5 ng/ml) and lower than in a study by Min–Chul and colleagues [34] (15.6 ng/ml). Vitamin D deficiency is a common issue, and low serum 25-hydroxycalciferol levels have been reported by numerous studies [14, 35, 36]. Although Kherson region is in the southern part of Ukraine, where the annual number of sunny days is higher than in Northern Ukraine, the level of insolation in the region is not sufficient to produce enough vitamin D for the body, which may be partially explained by the fact that older individuals spend little time outdoors. We found that women had lower serum 25-hydroxycalciferol level than men, and this difference was significant (р≤0.05) for groups with cataract plus myopia (Р=0.04) and cataract plus glaucoma (Р=0.006), but not for the cataract-only group. Findings from previous studies are inconsistent with regard to gender difference in serum 25-hydroxycalciferol levels. Most studies [14, 16, 37] noted that women had lower serum 25-hydroxycalciferol levels than men, but some studies found 25-hydroxycalciferol levels in the serum [25] and aqueous [34] to be higher in women than men. Because we found a gender difference in serum 25-hydroxycalciferol levels, we studied changes in 25-hydroxycalciferol levels with age and gender for patients with cataract plus POAG and patients with cataract plus high myopia. There was a significant difference in serum 25-hydroxycalciferol level between patients younger than 60 years and those older than 75 years for each study group. In addition, serum 25-hydroxycalciferol levels were lower in women than in men for patients with cataract plus POAG and those with cataract plus high myopia. It should be noted that there was a statistically significant difference (р=0.04) in serum 25-hydroxycalciferol level between the controls (patients with cataract only) aged below 60 years (28.5±6.4 ng/mL) and their peers with cataract plus high myopia (14.1±4.3 ng/mL) and cataract plus POAG (17.8±3.8 ng/mL), but not between the controls aged above 75 years (8.0±5.9 ng/mL) and their peers with cataract plus high myopia (8.7±4.5 ng/mL) and cataract plus POAG (7.6±3.0 ng/mL). Serum 25-hydroxycalciferol levels were significantly negatively correlated with age for patients with cataract only (r = -0.51, р = 0.001) and those with cataract plus POAG (r = -0.37, р = 0.03). A study by Abdellah and colleagues (2019) [20] but not studies by Cho and colleagues (2020) [34] and Rao and colleagues (2015) [16] also found serum 25-hydroxycalciferol levels to be correlated with age for patients with cataract. Of note, in the current study, serum 25-hydroxycalciferol levels were not significantly negatively correlated with age for patients with cataract plus myopia (r = -0.25, р = 0.06), which is likely to be at least partially explained by low serum 25-hydroxycalciferol levels in patients with cataract plus myopia for all age groups. Others have reported on associations of serum 25-hydroxycalciferol levels with the axial length of the eye and the risk of developing myopia in children. In addition, an association has been found between the time spent outdoors and myopia progression [15, 16, 36, 38, 40]. However, the relationship of serum 25-hydroxycalciferol levels and the onset of cataract in patients with high myopia has been poorly investigated. In the current study, of note, low serum 25-hydroxycalciferol levels were found not only in patients with high myopia, but also in those with glaucoma, and the amount of difference between groups was especially notable for patients younger than 60 years. Studies have reported on lower serum 25-hydroxycalciferol levels in patients with POAG compared to healthy individuals [39]. Particularly, serum vitamin D status was associated with the presence of POAG for populations from France, China and Africa [24, 26, 39-42. In the current study, we found lower serum 25-hydroxycalciferol levels (9.9 ± 7.1 ng/mL) in patients with cataract plus POAG compared to patients with cataract only (12.1 ± 5.6 ng/mL). Therefore, we found low serum 25-hydroxycalciferol levels in all patients with age-related cataract, especially in those with concomitant high myopia or POAG. Studying serum 25-hydroxycalciferol levels in patients with cataract and concomitant high myopia or POAG makes the fundamental difference between our study and most studies by others who mainly assessed associations of serum 25-hydroxycalciferol levels with types of cataract (cortical, nuclear, and posterior subcapsular cataract). The current study is limited by a small cohort and absence of distribution of patients depending on the type of cataract or the time spent outdoors. In spite of these limitations, our study identified an issue of very low serum 25-hydroxycalciferol levels in all patients with cataract, and a concomitant POAG or high myopia as an additional factor for low extremely low serum 25-hydroxycalciferol levels. Studies of serum 25-hydroxycalciferol levels in patients POAG or high myopia will be useful and improve our understanding of disease mechanisms, because in the human body, 25-hydroxycalciferol plays a role not only in the regulation of phosphorus and calcium metabolism, but also in the regulation of atherosclerosis, development of autoimmune abnormalities, and synthesis of cytokines, matrix metalloproteinases, and collagen. In conclusion, first, in all the examined Kherson-region patients with cataract, preoperative serum 25-hydroxycalciferol levels were substantially lower than reference values, with the levels for the patients with cataract only being deficient (i.e., 10 to 20 ng/ml), and those for the patients with cataract plus POAG or cataract plus high myopia being severely deficient. Second, among the patients younger than 60 years, those with cataract plus high myopia had the lowest mean serum 25-hydroxycalciferol level (14.1±4.3 ng/ml). Finally, all study patients older than 75 years showed severely deficient serum 25-hydroxycalciferol levels, with no significant difference among study groups. References 1.Vitovska OP. [Health promotion strategy in ophthalmology]. Russkii meditsinckii zhurnal. Klinicheskaia oftalmologiia. Glaukoma. 2013;3:88–92. Russian. 2.Malyugin BE, Timoshkina NT, Dzhndoyan GT, et al. [Outcomes of phacoemulsification with IOL implantation and simultaneous non-penetrating tunnel sclerectomy]. Oftalmokhirurgiia. 1997;3:49-57. Russian. 3.Zakhlyuk M. [Comprehensive surgical treatment of complicated cataracts in myopia]. [Abstract of Cand Sc (Med) Thesis]. Moscow; 2000. Russian. 4.Sokolov KV. [Features of surgical cataract treatment in patients with degenerative myopia]. Tikhookeanskii zhurnal. 2016;3:54–57. Russian. 5.Iusef IuN, Iusef SIu, Reznikova EV, Vvedenskiĭ AS. [Cataract surgery in patients with high myopia]. Vestn Oftalmol. 2005 Nov-Dec;121(6):47-9. Russian. 6.Aznabaev BM, Zagidullina AS, Lakman IA, Islamova RR, Sattarova RR. [Correlation of Corneoscleral Membrane Biomechanical Properties and Eye Morphometric Parameters in Patients with Primary Open-Angle Glaucoma]. Ophthalmology in Russia. 2019;16(3):335-43. Russian. 7.Belogurova AV. [Differential diagnosis criteria for and monitoring of the glaucoma process in axial myopia]. [Abstract of Cand Sc (Med) Thesis]. Moscow: Institute for Advanced Training of the Russian Federal Medical-Biological Agency. 2016. Russian. 8.Kazakova A.V., Eskina E.N. [Glaucoma diagnostics in myopic patients]. National Journal Glaucoma. 2015;14(3):87-100. Russian. 9.Yudashev AM, Usenko VA. [Clinico-anatomical features of the eye in patients with both high myopia and juvenile glaucoma]. Klinicheskaia oftalmologiia. 2017;4:244–7. Russian. 10.Gromova OA, Troshin IYu. Gusev EI, Zakharova IN, editors. [Vitamin D: A Change in Paradigm]. Moscow: Torus Press; 2015. Russian. 11.Pigarova EA, Rozhinskaya LY, Belaya JE, et al. [Russian Association of Endocrinologists recommendations for diagnosis, treatment and prevention of vitamin D deficiency in adults]. Problemy Endokrinologii. 2016;62(4):60-84. Russian. 12.Snopov SA. [Mechanisms of action of vitamin D on the immune system]. Meditsinskaia immunologiia. 2014;16(6):499–530. Russian. 13.Garcion E, Sindji L, Nataf S, et al. Treatment of experimental autoimmune encephalomyelitis in rat by 1,25–dihydroxyvitamin D3 leads to early effects within the central nervous system. Acta Neuropathol. 2003 May; 105(5):438–48. 14.Chailurkit LO, Aekplakorn W, Ongphiphadhanakul B. Regional variation and determinants of vitamin D status in sunshine–abundant Thailand. BMC Public Health. 2011 Nov 10;11:853. 15.Mutti DO, Marks AR. Blood Levels of Vitamin D in Teens and Young Adults with Myopia. Optom Vis Sci. 2011 Mar;88(3):377–82. 16.Rao P, Millen AE, Meyers KJ, Liu Z, Voland R, Sondel S, et al. The Relationship Between Serum 25–Hydroxyvitamin D Levels and Nuclear Cataract in the Carotenoid Age–Related Eye Study (CAREDS), an Ancillary Study of the Women's Health Initiative. Invest Ophthalmol Vis Sci. 2015 Jul;56(8):4221-30. 17.Bannur R, Voitovich AN, Larionova VI. [The role of the receptor for vitamin D and its genetic polymorphism in predicting the course of myopia in children]. Oftal’mol Vedomosti. 2010;3:27–33. Russian. 18.Beletskaya IS, Astakhov SYu, Karonova TL, et al. Pseudoexfoliative glaucoma and molecular genetic characteristics of vitamin D metabolism. Ophthalmology Journal. 2018;11(2):19-28. 19.Beletskaya IS, Karonova TL, Astakhov SYu. 25-Hydroxyvitamin D and matrix metalloproteinases-2, -9 level in patients with primary open angle glaucoma and pseudoexfoliative glaucoma/syndrome. Ophthalmology Journal. 2017;10(1):10-16. 20.Abdellah MM, Mohamed Mostafa E, Salama EH, Roshdy Mohamed E. Association of Serum 25-Hydroxyl Vitamin D Deficiency and Age-Related Cataract: A Case-Control Study. J Ophthalmol. 2019 Apr;2019:9312929. 21.Jee D, Kang S, Yuan C, Cho E, Arroyo JG. Serum 25–hydroxyvitamin D levels and dry eye syndrome: differential effects of vitamin D on ocular diseases. PLoS One. 2016 Feb 19;11(2):e0149294. 22.Jee D, Kim EC. Association between serum 25–hydroxyvitamin D levels and age–related cataracts. J Cataract Refract Surg. 2015;41(8):1705–1715. 23.Lin Y, Ubels JL, Schotanus MP, et al. Enhancement of vitamin D metabolites in the eye following vitamin D3 supplementation and UV–B irradiation. Curr Eye Res. 2012 Oct;37(10):871–8. 24.Lv Y, Yao Q, Ma W, et al. Associations of vitamin D deficiency and vitamin D receptor (Cdx–2, Fok I, Bsm I and Taq I) polymorphisms with the risk of primary open–angle glaucoma. BMC Ophthalmol. 2016;16:116. 25.Sanghera DK, Sapkota BR, Aston CE, Blackett PR. Vitamin D Status, Gender Differences and Cardiometabolic Health Disparities. Ann Nutr Metab. 2017;70(2):79–87. 26.Uro M, Beauchet O, Cherif M, Graffe A, Milea D, Annweiler C. Age–Related Vitamin D Deficiency Is Associated with Reduced Macular Ganglion Cell Complex: A Cross–Sectional High–Definition Optical Coherence Tomography Study. PLoS One. 2015 Jun 19;10(6):e0130879. 27.Yin Z, Pintea V, Lin Y, et al. Vitamin D enhances corneal epithelial barrier function. Invest Ophthalmol Vis Sci. 2011 Sep 21;52(10):7359-64. 28.Alsalem JA, Patel D, Susarla R, et al. Characterization of vitamin D production by human ocular barrier cells. Invest Ophthalmol VisSci. 2014; 55(4):2140–7. 29.Kheri B, Abdalla A, Osman M, Ahmed S, Hassan M, Bachuma G. Vitamin D deficiency and risk of cardiovascular diseases: a narrative review. Clin Hypertens. 2018 Jun 22;24:9. 30.Pupysheva AD, Kim EI. [Vitamin D and age-related macular degeneration]. Mezhdunarodnyi nauchno-issledovatelskii zhurnal. 2017;12 (66). Part 4:119–21. Russian. 31.Tucker ME. Vitamin D deficiency linked to diabetic retinopathy. Medscape Medical News. 2016 May28. Available at: http://www.medscape.com/viewarticle/863974. 32.Jung BJ, Jee D. Association between serum 25–hydroxyvitamin D levels and myopia in general Korean adults. Indian J Ophthalmol 2020 Jan;68(1):15-22. 33.Cho MC, Kim RB, Ahn JY, et al. Aqueous humor and serum 25-Hydroxyvitamin D levels in patients with cataracts. BMC Ophthalmol. 2020;20:6. 34.Grimm MOW, Thiel A, Lauer AA, Winkler J, Lehmann J, et al. Vitamin D and Its Analogues Decrease Amyloid–beta (Abeta) Formation and Increase Abeta–Degradation. Int J Mol Sci. 2017 Dec 19;18(12):2764. 35.Kwon JW, Choi JA, La TY. Serum 25–hydroxyvitamin D level is associated with myopia in the Korea national health and nutrition examination survey. Medicine (Baltimore). 2016 Nov; 95(46):5012. 36.Al-Horani H, Dayyih WA, Mallah E, Hamad M, Mima M, Awad R, et al. Nationality, gender, age, and body mass index influences on vitamin D concentration among elderly patients and young Iraqi and Jordanian in Jordan. Biochem Res Int. 2016;2:1–8. 37.Tideman JWL, Polling JR, Voortman T, Jaddoe AGU, et al. Low serum vitamin D is associated with axial length and risk of myopia in young children. Eur J Epidemiol. 2016;31:491–9. 38.Yazar S, Hewitt AW, Black LJ, McKnight CM, Mountain JA, et al. Myopia is associated with lower vitamin D status in young adults. Invest Ophthalmol Vis Sci. 2014 Jun 26;55(7):4552-9. 39.Yoo TK, Oh E, Hong S. Is vitamin D status associated with open–angle glaucoma? A cross–sectional study from South Korea. Public Health Nutr. 2014 Apr;17(4):833-43. 40.Goncalves A, Milea D, Gohier, et al. Serum vitamin D status is associated with the presence but not the severity of primary open angle glaucoma. Maturitas. 2015 Aug;81(4):470-4. 41.Briones TL, Darwish H. Vitamin D mitigates age–related cognitive decline through the modulation of pro–inflammatory state and decrease in amyloid burden. J Neuroinflammation. 2012 Oct 25;9:244. 42.Krefting EA, Jorde R, Cristoffersen T, Grimnes G. Vitamin D and intraocular pressure — results from a case–control and intervention study. Acta Ophthalmol. 2014 Jun;92(4):345-9.
|