J.ophthalmol.(Ukraine).2021;3:23-27.
|
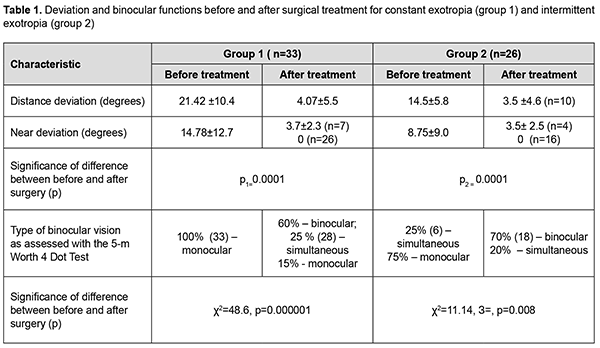
http://doi.org/10.31288/oftalmolzh202132327 Received: 09 February 2021; Published on-line: 29 June 2021 Stereopsis before and after surgical treatment for constant versus intermittent exotropia I. M. Boichuk, Alui Tarak SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine"; Odesa (Ukraine) E-mail: iryna.ods@gmail.com TO CITE THIS ARTICLE:Boichuk IM, Alui Tarak. Stereopsis before and after surgical treatment for constant versus intermittent exotropia. J.ophthalmol.(Ukraine).2021;3:23-27. http://doi.org/10.31288/oftalmolzh202132327 Background: Exophoria may be caused by congenital or acquired anomalies in orbital structure, ocular structure, extraocular muscle attachment and/or extraocular muscle location. Some researchers believe that the presence of stereopsis after treatment for strabismus indicates that a stable treatment outcome has been achieved and binocular vision regained. The state of stereopsis is believed to be an efficacy endpoint in the evaluation of strabismus surgery. Purpose: To assess stereopsis before and after surgery for constant versus intermittent exotropia. Material and Methods: Fifty-nine patients with constant or intermittent exotropia, aged 10 to 21 years, were included in the study. Of these, 33 (group 1) had constant exotropia and 26 (group 2), intermittent exotropia. They underwent surgery on one or both eyes. Visual acuity assessment, refractometry, and biomicroscopy were performed, near and distance angles of deviation were measured by Hirschberg's test and prism cover test, the color test was used to determine the type of binocular vision, and synoptophore, to examine fusion both before and after treatment. Stereoacuity thresholds were assessed with Lang-Stereotest II and Titmus Stereo Fly (circles and animals) tests at daylight at a viewing distance of 30 cm and a Huvitz CCP3100 Chart Projector was used to assess whether stereopsis was present at a 5-m distance. Results: After treatment, the magnitude of exotropia decreased in all patients, and the mean angle of deviation at near was 3.5±1.4 degrees, and at distance, 3.9±1.9 degrees. In addition, 70% of patients regained binocular vision. At baseline, neither patient in group 1 and only three patients in group 2 exhibited distance stereopsis. After treatment for strabismus, 11 patients in group 1 exhibited near stereopsis, and stereoacuity threshold as assessed by the Titmus Stereo Fly (circles and animals) test was 200-400 arc sec in 24.4% of patients of this group. In addition, in 80.8% of patients of group 2, the stereoacuity threshold was 1500 arc sec, and the stereoacuity normalized and was 200 arc sec as assessed by the circles subtest. That is, after surgery, stereoacuity thresholds decreased substantially, especially in group 2. Conclusion: After surgery, in 70-80% of cases, stereoacuity increased (stereoacuity thresholds decreased), indicating that the surgical treatment was effective and binocular functions were regained. Our preliminary results suppose that a preoperative near stereoacuity of 200 arc sec will be a favorable factor for improvement in binocular functions and stable orthotropia after surgery for intermittent exotropia. Ключові слова: розбіжна косоокість постійна, періодична, стан стереозору для далекої і близької відстані, хірургічне лікування Conflict of Interest Statement: The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript. Introduction Exotropia occurs less frequently than esotropia (with a prevalence ratio of approximately 1:3 [1]), and differs from other types of strabismus in that a change in the angle of deviation may occur at any time of the day or night. In addition, the angle of deviation may be larger at near (convergence insufficiency) or at distance (divergence excess). The mechanisms of these oculomotor abnormalities involve various degrees to which fusion and vergence are compromised, and the relation between accommodation and convergence [2-7]. Due to these reasons, it may be difficult to differentiate exophoria (latent exotropia) from apparent exotropia, and constant exotropia at distance from intermittent exotropia at distance. A change from exophoria to manifest exotropia is rather common. Exophoria may be caused by congenital or acquired anomalies in orbital structure, ocular structure, extraocular muscle attachment and/or extraocular muscle location [2, 3, 8-11]. Intermittent exotropia is most commonly (82-86%) due to convergence insufficiency or abnormalities of the central nervous system [6, 7]. Restoration of binocular fusion at distance and near after surgery for exotropia is observed in 40-95% of the patients [1, 12, 13]. There have been reports on the state of convergence, strabismus angle, fusional capacity, and type of binocular vision in exotropia [7, 14]. Stereopsis has been assessed with various tests in various groups of patients with exotropia, mostly after surgery for exotropia. The stereoacuity threshold in early surgery for congenital strabismus was of 1500 arc sec [4, 5, 15, 16], i.e., substantially above the normal range. Those authors believe that this indicated a persistent effect of surgery, a proper eye position. Near and distance stereoacuity thresholds have been reported for some forms of exotropia [7, 17-19]. It has been, however, not assessed, whether the presence or magnitude of stereoacuity threshold may influence the outcomes of conservative or surgical treatment for patients with exotropia. In addition, it is believed that clinicians should understand characteristics of various stereoacuity tests to utilize test data for a particular patient [6, 7, 20]. The purpose of this study was to assess stereopsis before and after surgery for constant versus intermittent exotropia. Material and Methods Fifty-nine patients with constant or intermittent exotropia, aged 10 to 21 years, were included in the study. Of these, 33 (group 1) had constant exotropia and mean BCVA of 0.83±(SD) 0.33, and 26 (group 2), intermittent exotropia and mean BCVA of 0.82±(SD) 0.35. In both groups, the refractive error ranged from -5.5D to +7.5D. Sixty-five percent of patients had a vertical component ranging from 0 to 3 degrees. In group 1, the angle of deviation measured at distance ranged from 11 to 35 degrees (mean value, 21.42±(SD) 10.4 degrees), and the mean value for the angle of deviation measured at near was 14.8±(SD) 12.7 degrees. In group 2, the angle of deviation measured at distance ranged from 9.7 to 20.4 degrees (mean value, 14.5±(SD) 5.8 degrees), and the mean value for the angle of deviation measured at near was 8.75±(SD) 9.0 degrees. The surgery was performed in one or both eyes in a routine manner [1, 12, 13]. Visual acuity assessment, refractometry, and biomicroscopy were performed, near and distance angles of deviation were measured by Hirschberg's test and prism cover test, the color test was used to determine the type of binocular vision, and synoptophore, to examine fusion both before and after treatment. Stereoacuity thresholds were assessed with Lang-Stereotest II and Titmus Stereo Fly (circles and animals) tests at daylight at a viewing distance of 30 cm, under conditions of best-corrected vision. In addition, a Huvitz CCP3100 Chart Projector was used to assess whether stereopsis was present at a 5-m distance. Statistica 8.0 (StatSoft, Tulsa, OK, USA) software was used for statistical analysis. Mean (M) and standard deviations (SD) were calculated for quantitative variables. The level of significance p ≤ 0.05 was assumed. Group results were compared using the chi-square test and Newman–Keuls multiple comparison test. The study followed the ethical standards stated in the Declaration of Helsinki, the European Convention on Human Rights and Biomedicine and relevant laws of Ukraine. Results After treatment, the magnitude of exotropia decreased in all patients, and the mean angle of deviation at near was 3.5±1.4 degrees, and at distance, 3.9±1.9 degrees. In addition, 70% of patients regained binocular vision. Table 1 presents pre-treatment and post-treatment deviation angles and binocular function data for patients with constant exodeviation and patients with intermittent exodeviation. The magnitude of deviation significantly decreased after surgical treatment (p =0.0001) (Table 1). Ocular alignment was obtained and binocular vision was regained following surgery by 71.2% of patients. Preoperatively, all patients with constant deviation and 11 patients with intermittent deviation (42.3%) failed distance stereoacuity testing.
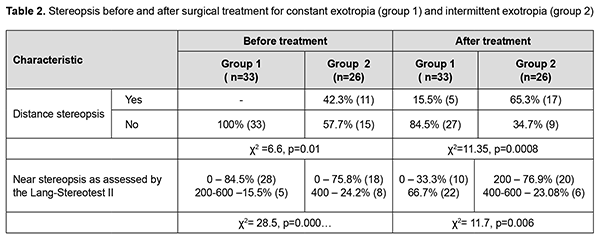
After treatment, stereoacuity improved in both groups (Tables 2 and 3). Particularly, five patients of group 1 and 17 (65.3%) of group 2 had distance stereopsis after treatment. In group 1, near stereoacuity thresholds were determined in 5 patients (15.5%) before treatment and in 22 patients (66.7%) after treatment, but stereoacuity thresholds were above the normal range. In group 2, near stereoacuity thresholds were within the normal range in 20 patients (76.9%) and above the normal range in 6 patients (23.08%) (Table 2). Therefore, before and after treatment, stereoacuity was generally better in patients of group 2 than in patients of group 1. After treatment, stereoacuity threshold was 200-400 arc sec.
Of note that, orthotropia (an absence of a manifest deviation) was achieved in individuals with both post-treatment distance stereopsis and a pre-treatment stereoacuity threshold at near of not more than 200 arc sec in three of the five patients. Table 3 presents pre-treatment and post-treatment stereoacuity, as assessed by the Titmus Stereo Fly test. At baseline, neither patient in group 1 and only 3 patients in group 2 exhibited distance stereopsis. After treatment for strabismus, near stereopsis was found in 11 patients of group 1, and, in 15.5% of patients of this group, stereoacuity threshold as assessed by the Titmus Stereo Fly (circles and animals) test was 200-400 arc sec. In addition, in 80.8% of patients of group 2, the stereoacuity threshold was 1500 arc sec, and, in 75.6% of patients of group 2, the stereoacuity normalized and was 200 arc sec as assessed by the circles subtest. That is, after surgery, stereoacuity thresholds decreased substantially, especially in group 2. That is, after surgery, stereoacuity thresholds decreased substantially, especially in group 2. Discussion It has been reported on the effects of some baseline characteristics (like convergence, angle of strabismus, presence of fusion, and type of binocular vision) on the outcomes of surgery for exotropia [5, 6, 19]. Stereopsis in exotropia has been assessed in various groups of patients using various tests and mostly after surgery, which makes it difficult to compare our results with previous studies. Although others did assess stereocuity thresholds in some forms of exotropia [21-24], it has been not assessed whether and in which way the stereoacuity at baseline influences the outcomes of surgical treatment for patients with exotropia. Therefore, in the current study, we found that, preoperatively, the percentages of patients failing distance stereoacuity testing and near stereoacuity testing were 100% and 75%, respectively, for the group with constant exotropia, and 15.5% and 75.8%, respectively, for the group with intermittent exotropia. In addition, after surgery, stereoacuity increased (stereoacuity thresholds as assessed by the Lang-Stereotest II decreased to 200-400 arc sec) in 24.4% of patients of group 1 and 75.6% of patients of group 2, indicating that the surgical treatment was more effective and binocular functions were regained, but more substantially in patients with intermittent exotropia. Our preliminary results suppose that a preoperative near stereoacuity of 200 arc sec will be a favorable factor for improvement in binocular functions and stable orthotropia after surgery for exotropia.
References 1.Von Noorden GK, Campos E. Binocular Vision and Ocular motility. Theory and Management of Strabismus. Mosby: St. Louis; 2002. p. 5-18. 2.Awaya S, Nozaki H, Itoh T, Hanada K. Studies of suppression in alternating constant exotropia and intermittent exotropia with reference to fusional background. In: Moore S, Mein J, Stockbridge L, eds. Orthoptics: Past, Present, Future. Miami, FIa: Symposia Specialists, 1976:531. 3.Awaya S, Sugawara M, Komiyama K, Ikeyama K. Studies on stereoacuity in four constant exotropes with good stereoacuity, with a special reference to the Titmus stereo test and EOG analysis. Nippon Ganka Gakkai Zasshi. 1979 May 10;83(5):425-30. Japanese. 4.Chavasse F. Worth's squint or the binocular reflexes and the treatment of strabismus. 7th ed. London: Bailliere Tindall and Cox; 1939. 5.Jung EH, Kim SJ, Yu YS. Factors associated with surgical success in adult patients with exotropia. J AAPOS. 2016 Dec;20(6):511-514. 6.Kim MK, Kim US, Cho MJ, Baek SH. Hyperopic refractive errors as a prognostic factor in intermittent exotropia surgery. Eye (Lond). 2015 Dec;29(12):1555-60. 7.Lang JI. Ein neuer Stereotest. Klin Mbl Augenheilk. 1983;182:373–5. 8.Kashchenko TP, Pospelov VI, Shapovalov SL. [Problems of oculomotor and binocular pathology] In: [Proceedings of the 8th Congress of Ophthalmologists of Russia]. Moscow, 1-4 Jun 2015. Moscow: MNTK “Eye Microsurgery” Publishing Center; 2005. p.740-1. Russian. 9.Bach-y-Rita P. Neurophysiology of eye movements: Control of Eye Movements. New York: Academic Press; 1971. 10.Ball A, Drummond GT, Pearce WG. Unexpected stereoacuity following surgical correction of long-standing horizontal strabismus. Can J Ophthalmol. 1993 Aug;28(5):217-20. 11.Beneish R, Flanders M. The role of stereopsis and early postoperative alignment in long-term results of intermittent exotropia. Can J Ophthalmol. 1994 Jun;29(3):119-24. 12.Avetisov ES. [Concomitant strabismus]. Moscow: Meditsina; 1977. Russian. 13.Avetisov ES, Tarastsova MM, Khukhrina LP. [Methods and results of studies on binocular vision in preschool children]. Oftalmol Zh. 1977;32(2):86-9. Russian. 14.Carpenter RHS. Movements of the eyes. London: Pion Limited (2nd ed), 1988. 15.Birch EE, Gwiazda J, Held R. The development of vergence does not account for the onset of stereopsis. Perception. 1983;12(3):331-6. 16.Bishop PO, Pettigrew JD. Neural mechanisms of binocular vision. Vision Res. 1986;26(9):1587-600. 17.Berard P. Prisms: their therapeutic use in strabismus. In: Knapp P, ed. International Strabismus Symposium: an evaluation of present status of orthoptics, pleoptics, and related diagnosis and treatment regimes. New York: Karger; 1968. p.339-44.Crossref 18.Goodwin RT, Romano PE. Stereoacuity degradation by experimental and real monocular and binocular amblyopia. Invest Ophthalmol Vis Sci. 1985 Jul;26(7):917-23. 19.Kim HJ, Choi DG. Clinical analysis of childhood intermittent exotropia with surgical success at postoperative 2 years. Acta Ophthalmol. 2016 Mar;94(2):e85-9. 20.Lang J. Strabismus. Thorofare, N J: Slack:1984. 21.Nishikawa N, Ishiko S, Yamaga I, Sato M, Yoshida A . Distance stereotesting using vision test charts for intermittent exotropia. Clin Ophthalmol. 2015 Aug 25;9:1557-62. 22.Na KH, Kim SH. Comparison of clinical features and long-term surgical outcomes in infantile constant and intermittent exotropia. J Pediatr Ophthalmol Strabismus. Mar-Apr 2016;53(2):99-104. 23.Yang M, Chen J, Shen T, Kang Y, Deng D, Lin X, et al. Single stage surgical outcomes for large angle intermittent exotropia. PloS one. 2016;11(2):e0150508. 24.Yang M, Chen J, Shen T, Kang Y, Deng D, Lin X, et al. Clinical characteristics and surgical outcomes in patients with intermittent exotropia: a large sample study in South China. Medicine (Baltimore). 2016 Feb;95(5):e2590.
|