J.ophthalmol.(Ukraine).2021;4:57-60.
|
http://doi.org/10.31288/oftalmolzh202145760 Received: 01 January 2021; Published on-line: 16 August 2021 The relation between Eyelid Tumors and Demographic Variable Meisam Akhlaghdoust 1, 2, Saeid Safari 1, 2, Poorya Davoodi 3, 4, Shaghayegh Soleimani 5, Ehsan Ebadian 3, 6 1 Functional Neurosurgery Research Center, Shohada Tajrish Comprehensive Neurosurgical Center of Excellence, Shahid Beheshti University of Medical Sciences; Tehran (Iran) 2 Functional Neurosurgery Research Center, Universal Scientific Education and Research Network (USERN); Tehran (Iran) 3 University of Padua; Padua (Italy) 4 Pars Advanced and Minimally Invasive Medical Manners Research Center, Pars Hospital, Iran University of Medical Sciences; Tehran (Iran) 5 School of Paramedical Sciences, Tehran Medical Sciences, Islamic Azad University; Tehran (Iran) 6 Tehran Medical Sciences Islamic Azad University; Tehran (Iran) E-mail: safari.s@sbmu.ac.ir TO CITE THIS ARTICLE: Meisam Akhlaghdoust, Saeid Safari, Poorya Davoodi, Shaghayegh Soleimani, Ehsan Ebadian. The relation between Eyelid Tumors and Demographic Variable. J.ophthalmol.(Ukraine). 2021;4:57-60. http://doi.org/10.31288/oftalmolzh202145760 Aims: This study evaluated the relationship between demographic variables, location, histopathologic results with Eyelid Tumors in Labbafinejad hospital in Tehran from 2010 to 2020. Methods and Material: The t-test and analysis of variance were used for comparison of normally distributed variables among groups. Results: The study was performed on 97 men and 115 women, in which we found 88 cases of benign tumors and 124 cases of malignant tumors. The mean age of the patients was 51.04± 22.9 years ranged between 1- 89. The topography analysis of lesions showed the frequency of locations: 98 cases at the lower eyelid, 112 cases at the upper eyelid, and 2 on both sides, 107 cases at the right eyelid, 101 cases at the left eyelid, and 4 in both eyelids. We realized that basal cell carcinoma was the most frequent malignancy reported, followed by squamous cell carcinoma, whereas intradermal nevus and dermoid cyst made up most of the benign lesions, respectively. Our data also demonstrated a significant difference in the number of men diagnosed over women with basal cell carcinoma. Conclusions: In this study, 54.8% of lesions were malignant, found mostly in men. The top two types of malignant tumors were basal cell carcinoma and squamous cell carcinoma, and the most frequent benign lesions were intradermal nevus and dermoid cyst, respectively. Key words: basal cell carcinoma; dermoid cyst; eyelid; intradermal nevus; squamous cell carcinoma
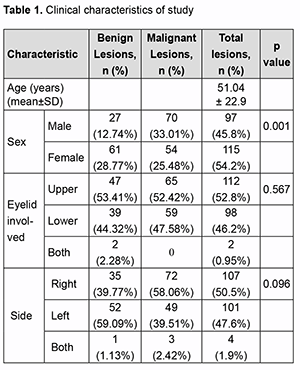
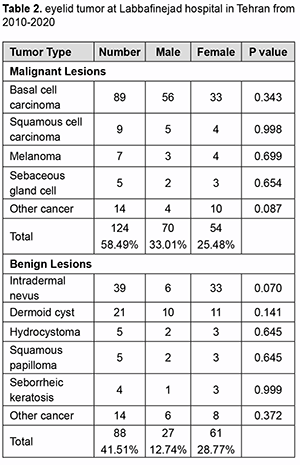
Introduction Eyelid tumors are the most frequent neoplastic lesions in the field of ophthalmology. Among these, skin cancers are a particular concern in sun-exposed older patients, with an estimated 60,000 malignant eye-lid tumors diagnosed yearly in the United States. Eyelid neoplastic pathology is very polymorphic and mostly based on different types of skin cancer, mainly including basal cell carcinoma, squamous cell carcinoma, accessory glands carcinomas, and malignant melanoma. Many cutaneous and eyelid diseases are quite similar because of the common ontogenetic origin. Statistically, 90% of skin cancers arise from the head and neck, and 10% of these are located in eyelid structures [1]. As mentioned above, eyelid tumors make up the biggest part of total neoplastic le-sions among all ophthalmologic neoplasms, including different kinds of benign and malignant tumors. It is shown in multiple recent studies that the amount of sun exposure and, more specifically, Ultra Violet light exposure has a direct relation with the risk of developing different types of skin cancers [2]. In some other studies, authors com-pared the incidence of the most frequent skin cancer, basal cell carcinoma (BCC), in Polar Regions with equatorial geographic regions of the world. Higher incidence of BCC in equatorial regions strengthens this direct relation be-tween skin tumors and sun exposure [3, 4]. However, it is seen that patients show more apprehension about orbital and periorbital lesions including eyelid tumors, compared to other sorts of injuries. The important thing to know is that benign tumors are vastly more than malignant tumors among all eyelid neoplastic lesions. Eyelid tumors stand for 15% of all malignancies in the facial region and 5–10% of total cutaneous tumors of the body. [5,6] Patients over 60 years old are seen to be more sus-ceptible to develop eyelid tumors. According to recent studies, most malignant tumors grow in the lower eyelid and medial canthus, while benign lesions are more frequently seen in the upper eyelid and lateral canthus [7-10]. Despite the polymorphic clinical and histopathological aspects, the most frequent benign tumor is squamous papilloma, while the most common malignant eyelid tumor is basal cell carcinoma, which is known to be the most common malignancy in 80-95% of all eyelid cancer patients in the United States and Europe [10, 11]. Although the prevalence of eye metastasis (uveal metastasis) singly transcends the metastases to the orbit, eye-lid, and other periocular structures (ocular adnexa), caused damages to these adnexal tissues are apparently consid-erable [12-14]. According to recent studies, among all cases developing orbital tumors, 1 to 13% are originally meta-static lesions. It is estimated that 2 to 4.7% of patients suffering from systemic cancer may develop orbital metas-tasis [14-18]. Unpleasantly, the percentage of orbital metastatic tumors in orbital and periocular tissues is escalating annually [14-16]. Most of these orbital metastatic tumors are carcinomas and among the population, elderly aged more than 75 years old are the most susceptible to develop these sorts of tumors [19, 20]. All these have the respon-sibility for an early diagnosis, which is the prognostic key of malignant lesions. As we mentioned above, although the death rate is comparatively low, morbid consequences are apparently considerable. Founding an effective and affordable method with the lowest recurrence contingency for the elimination of the tumor is the purpose of the new researches. This study was aimed to describe the incidence, presentation, and epidemiology of eyelid tumors diagnosed in Labbafinejad hospital in Tehran from 2010-2020 and the relativity between eyelid tumors and demo-graphic characters. Materials and Methods This study was a retrospective analysis of eyelid tumors in which the records of all patients with eyelid lesions admitted to Labbafinejad Hospital between January 2010 and September 2020 were reviewed. Patient age, gender, distribution of lesions, location, clinical diagnosis, and the histopathological result of tumors were analyzed. Com-parison of normally distributed variables among groups was performed using t-tests and analysis of variance. Results The study comprised 212 cases, in which we found 88 benign tumors and 124 cases of malignant tumors. The mean age of the patients’ group was 51.04± 22.9 years with a range between 1- 89-year-old. The topography anal-ysis of lesions showed the frequency of locations: 98 cases at the lower eyelid, 112 cases at the upper eyelid, and 2 on both sides, 107 cases at the right eyelid, 101 cases at the left eyelid, and 4 in both eyelids (Table 1).
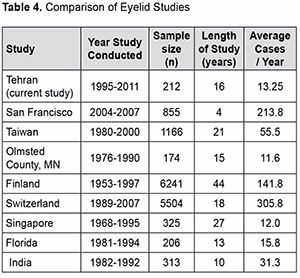
Discussion To our knowledge, this is one of the few studies analyzing the distribution of eyelid lesions in a richly diverse ethnic Iranian population. Studies referenced in this paper retrieved their data from a variety of sources, including national and local cancer registries as well as hospital pathology laboratory data (Table 2). The authors still believe that this study shows an interesting overview of data from a busy, community hospital caring for a diverse urban population that is important for ophthalmologists and other physicians. The authors report an increased incidence of basal cell carcinoma in the female population. Our study confirms that the incidence of malignant eyelid lesions rises with age.
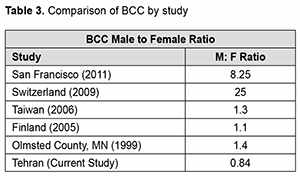
The topography analysis of lesions revealed the distribution and frequency of tumors’ locations: 98 cases at the lower eyelid, 112 cases at the upper eyelid, and 2 on both sides, 107 cases at the right eyelid, 101 cases at the left eyelid, and 4 in both eyelids (Table 1). Similarly, in most of the previous data, malignant tumors developed more commonly in the lower eyelid than the upper eyelid. [1, 5, 7-9]. In agreement with m of both the er published studies, basal cell carcinoma was the most common malignancy reported. It should be mentioned that some recent studies carried out in eastern Asia revealed that in their commu-nity, sebaceous gland carcinoma incidence rate is much higher compared with basal cell carcinoma [11]. In agreement with some recent studies in Saudi Arabia, Brazil, and North America, our data demonstrated a sig-nificant difference in the number of men diagnosed over women with basal cell carcinom, whereas, in some other studies, an equal male/female distribution was mentioned [2, 3, 9, 13, 21-25]. We believe that this may be due to the higher use of sunscreen by women, the use of occlusive makeup or sunscreen containing makeup in women, and the culture of sunbathing and water sports among men in the Iranian community. Results of a 19-year study in Ankara, Turkey, shows that 73.1% of eyelid tumors are benign while 25.2% repre-sents malignant signs [1]. Bonavolonta G et al. also found that 68% of eyelid neoplastic lesions were benign, while malignant tumors contributed 32% of the total eyelid lesions [17]. Another older study in Ankara, Turkey, indicated an absolute predominance of benign tumors from malignant ones, representing 92.5% of all cases [26]. We believe that the high incidence of malignant tumors compared to benign tumors in our study may be mainly because the hospital we gathered our data from is a tertiary care center and a referral hospital for ophthalmology patients. Many trials studied the incidence of eyelid tumors with different histopathological types. A large casuistry study by Deprez et al. included 5504 cases, indicated that 86% were benign tumors, the most frequent being squamous cell papilloma (26%) seborrheic keratosis (21%), melanocytic nevus (20%), hidrocystoma (8%), and xantho-ma/xanthelasma (6%). In the same study, malignant neoplasms were made up of basal cell carcinoma (86%), fol-lowed by squamous cell carcinoma (7%) and sebaceous carcinoma (3%) [27]. Sha-Sha Yu et al. reviewed 2228 cases retrospectively from 2002 to 2015, showing that 13.1% of eyelid lesions were malignant, which mainly made up of basal cell carcinoma (56.5%), sebaceous carcinoma (34.6%), squamous cell carcinoma (3.8%) and lymphoma/plasmocytoma (1.7%) [5]. Another retrospective study recorded in five years (2000–2004) reviewed 53 (17.8%) inflammatory conditions, 212 (71.4%) benign eyelid tumors, and 32 (10.8%) malignant eyelid tumors, included 13 sebaceous gland carcinomas, 12 basal cell carcinomas, three malignant mel-anomas, two squamous cell carcinomas, one apocrine adenocarcinoma, and one metastatic carcinoma. [28] One of the recent retrospective studies analyzed 851 eyelid tumors over 30 years, curiously showed a much higher rate of malignant tumors among all neoplastic eyelid lesions. It showed that 351 (41.2%) tumors were malignant, whereas 500 (58.8%) lesions were benign. Malignant tumors were mostly basal cell carcinoma (86%), squamous cell carcinoma (7%), and basosquamous cell carcinoma (7%). Benign neoplasms were made up of cysts (20%), sebor-rheic keratosis (18%), nevus (13%), and papilloma (13%) [29]. Squamous carcinomas are the second common cause of malignant neoplasms at the eyelid structure, represent-ing 5–10% of all eyelid malignant tumors [11]. The tumoral incidence per 100 000 people is around 0.09–2.42% [30]. We must again mention that our study was performed on the data of a tertiary referral hospital that would nor-mally deal with more cases that are malignant rather than benign ones, and this would affect the distribution of neoplastic tumors. Accordingly, the actual incidence of benign tumors may be higher than what we have measured. However, we attempted to decrease this possible bias by studying on a large group for a long period so that we can ensure that our study can represent a restrained and acceptable epidemiologic study in the Iranian community.
Conclusion The aim of our study was to describe the incidence, presentation, and epidemiology of eyelid tumors and relativ-ity between eyelid tumors and demographic characters in the Iranian community. As measured, basal cell carcino-ma was the most common malignancy reported. Our data demonstrated a significant difference in the number of men diagnosed over women with basal cell carcinoma. We also observed an increased incidence of basal cell carcinoma in the female population. Our study also confirmed that the incidence of malignant eyelid lesions rises with age. The major outcomes of our study are to warn about the increase of eyelid malignancies over recent years, demanding more therapeutic and preventing techniques to slow down this rise, and most importantly, the need for more extensive studies in this field to realize other possible demographic causative factors. References 1.Eren MA, Gunduz AK. Demographic features and histopathological diagnosis in primary eyelid tumors: results over 19 years from a tertiary center in Ankara, Turkey. Int J Ophthalmol 2020;13(8):1287-1293. 2.Szewczyk M, Pazdrowski J, Golusinski P, et al. Basal cell carcinoma in farmers: an occupation group at high risk. Int Arch Occup Environ Health 2016;89(3):497-501. 3.Shi Y, Jia R, Fan X. Ocular basal cell carcinoma: a brief literature review of clinical diagnosis and treatment. Onco Targets Ther 2017;10:2483-2489. 4.Situm M, Buljan M, Bulat V, Lugovic Mihic L, Bolanca Z, Simic D. The role of UV radiation in the development of basal cell carcinoma. Coll Antropol 2008;32 Suppl 2:167-70. (https://www.ncbi.nlm.nih.gov/pubmed/19138022). 5.Yu SS, Zhao Y, Zhao H, Lin JY, Tang X. A retrospective study of 2228 cases with eyelid tumors. Int J Ophthalmol 2018;11(11):1835-1841. DOI: 10.18240/ijo.2018.11.16. 6.Yin VT, Merritt HA, Sniegowski M, Esmaeli B. Eyelid and ocular surface carcinoma: diagnosis and management. Clin Dermatol. 2015 Mar-Apr;33(2):159-69. 7.Pe'er J. Pathology of eyelid tumors. Indian J Ophthalmol 2016;64(3):177-90. 8.Yu SS, Zhao Y, Zhao H, Lin JY, Tang X. A retrospective study of 2228 cases with eyelid tumors. Int J Ophthalmol 2018;11(11):1835-1841. 9.Hamada S, Kersey T, Thaller VT. Eyelid basal cell carcinoma: non-Mohs excision, repair, and outcome. Br J Ophthalmol 2005;89(8):992-4. 10.Mohite AA, Johnson A, Rathore DS, et al. Accuracy of clinical diagnosis of benign eyelid lesions: Is a dedicated nurse-led service safe and effective? Orbit 2016;35(4):193-8. 11.Kaliki S, Bothra N, Bejjanki KM, et al. Malignant Eyelid Tumors in India: A Study of 536 Asian Indian Patients. Ocul Oncol Pathol 2019;5(3):210-219. 12.Kaliki S, Jajapuram SD, Maniar A, Mishra DK. Ocular and Periocular Tumors in Xeroderma Pigmentosum: A Study of 120 Asian Indian Patients. Am J Ophthalmol 2019;198:146-153. 13.Marzuka AG, Book SE. Basal cell carcinoma: pathogenesis, epidemiology, clinical features, diagnosis, histopathology, and management. Yale J Biol Med 2015;88(2):167-79. (https://www.ncbi.nlm.nih.gov/pubmed/26029015 14.Ahmad SM, Esmaeli B. Metastatic tumors of the orbit and ocular adnexa. Curr Opin Ophthalmol 2007;18(5):405-13. 15.Allen RC. Orbital Metastases: When to Suspect? When to biopsy? Middle East Afr J Ophthalmol 2018;25(2):60-64. 16.Eldesouky MA, Elbakary MA. Clinical and imaging characteristics of orbital metastatic lesions among Egyptian patients. Clin Ophthalmol 2015;9:1683-7. 17.Bonavolonta G, Strianese D, Grassi P, et al. An analysis of 2,480 space-occupying lesions of the orbit from 1976 to 2011. Ophthalmic Plast Reconstr Surg 2013;29(2):79-86. 18.Magliozzi P, Strianese D, Bonavolonta P, et al. Orbital metastases in Italy. Int J Ophthalmol 2015;8(5):1018-23. 19.Szturz P, Vermorken JB. Treatment of Elderly Patients with Squamous Cell Carcinoma of the Head and Neck. Front Oncol 2016;6:199. 20.Garcovich S, Colloca G, Sollena P, et al. Skin Cancer Epidemics in the Elderly as An Emerging Issue in Geriatric Oncology. Aging Dis 2017;8(5):643-661. 21.Al Wohaib M, Al Ahmadi R, Al Essa D, et al. Characteristics and Factors Related to Eyelid Basal Cell Carcinoma in Saudi Arabia. Middle East Afr J Ophthalmol 2018;25(2):96-102. 22.Lara F, Santamaria JR, Garbers LE. Recurrence rate of basal cell carcinoma with positive histopathological margins and related risk factors. An Bras Dermatol 2017;92(1):58-62. 23.Mohammad EA, Mansour M, Parichehr K, Farideh D, Amirhossein R, Ahmad SA. Assessment of clinical diagnostic accuracy compared with pathological diagnosis of basal cell carcinoma. Indian Dermatol Online J 2015;6(4):258-62. 24.Saleh GM, Desai P, Collin JR, Ives A, Jones T, Hussain B. Incidence of eyelid basal cell carcinoma in England: 2000-2010. Br J Ophthalmol 2017;101(2):209-212. 25.Domingo RE, Manganip LE, Castro RM. Tumors of the eye and ocular adnexa at the Philippine Eye Research Institute: a 10-year review. Clin Ophthalmol 2015;9:1239-47. 26.Gundogan FC, Yolcu U, Tas A, et al. Eyelid tumors: clinical data from an eye center in Ankara, Turkey. Asian Pac J Cancer Prev 2015;16(10):4265-9. 27.Deprez M, Uffer S. Clinicopathological features of eyelid skin tumors. A retrospective study of 5504 cases and review of literature. Am J Dermatopathol 2009;31(3):256-62. 28.Pornpanich K, Chindasub P. Eyelid tumors in Siriraj Hospital from 2000-2004. J Med Assoc Thai 2005;88 Suppl 9:S11-4. (https://www.ncbi.nlm.nih.gov/pubmed/16681045). 29.Asproudis I, Sotiropoulos G, Gartzios C, et al. Eyelid Tumors at the University Eye Clinic of Ioannina, Greece: A 30-year Retrospective Study. Middle East Afr J Ophthalmol 2015;22(2):230-2. 30.Burgic M, Iljazovic E, Vodencarevic AN, et al. Clinical Characteristics and Outcome of Malignant Eyelid Tumors: A Five-Year Retrospective Study. Med Arch 2019;73(3):209-212. 31.Mehdizadehkashi K, Chaichian S, Mehdizadehkashi A, et al. Visual acuity changes during pregnancy and postpartum: a cross-sectional study in Iran. J Pregnancy 2014;2014:675792. 32.Chaichian S, Mehdizadehkashi K, Pazouki A, Jafarzadehpour E, Akhlaghdoust M, Sheikhvatan M. Hyperopic Shift in Obese Patients After Bariatric Surgery: A Clinical Trial. Bariatric Surgical Practice and Patient Care. 2018 Dec 1;13(4):156-62. No conflict of interest was declared by the authors Received 01.01.21
|