J.ophthalmol.(Ukraine).2022;3:63-64.
|
http://doi.org/10.31288/oftalmolzh202236364 Received: 05.07.2021; Accepted: 16.09.2021; Published on-line 15.06.2022 Branch retinal vein occlusion on Coats disease during COVID-19 infection: a case report Leopoldo Garduño Vieyra, Dr.; Dr. Raúl Rúa Martínez, Dr; Bruno Flores Escobar, Dr. Clínica Oftalmología Garduño; Irapuato, Guanajuato (México) E-mail: ruamartinez@yahoo.es TO CITE THIS ARTICLE:Leopoldo Garduño Vieyra, Raúl Rúa Martínez, Bruno Flores Escobar. Вranch retinal vein occlusion on Coats disease during COVID-19 infection: a case report. J.ophthalmol.(Ukraine).2022;3:63-4. http://doi.org/10.31288/oftalmolzh202236364 Background. The COVID-19 virus infection can develop ocular manifestations. Purpose. To report a case of a coats disease patient who was evaluated one week before as part of a routine retinal consultation and later had COVID-19 with sudden loss of vision on one eye. Material and Methods. the affected eye had a visual acuity of 20/400. At fundus examination was found abnormal tortuous vasculature, hemorrhages, branch retinal vein occlusion and macular edema. It was confirm with fluorescein angiography and optical coherence tomography. Results. With a combined therapy of intravitreal Aflibercept, periocular triamcinolone and focal laser was recovery the visual acuity to 20/20. Conclusion. There are few cases describes on literature, but a sudden loss of vision during a COVID-19 infection must be early detected and treated to achieve a better visual acuity recovery. Key words: covid-19, Coats disease, branch retinal vein occlusion, retina, virus Introduction The 2019 coronavirus (COVID-19) is an RNA virus belonging to the coronaviridae family. This virus infection can cause atypical pneumonia and acute respiratory distress syndrome with notable mortality rates. That is why it was considered a world pandemic [1]. COVID-19 as other viral infectious diseases such as Dengue and Chikungunya has ocular manifestation. The most common is conjunctivitis, but it has found retinal complications too [2, 3]. Those retinal manifestations are related to coagulopathy that had been well documented [2]. Stroke is associated with COVID-19 because of its hypercoagulability and thromboembolic tendency, then it can happen in the eye [4]. Those coagulation disorders are common in COVID-19 patients, but most frequently in severe infection cases. Studies refer a diffuse endothelial damage on different part of the body. In these patients, blood hypercoagulability and prothrombin and thromboplastin time alterations has been found [5]. Retinal manifestation occur due complement activated thrombotic microangiopathy and hypercoagulable state. This causes retinal artery and vein occlusions. The common mechanisms for development of retinal vein occlusion include arteriosclerosis, hypercoagulability, vasculitis secondary to systemic inflammation or a combination of all. A hypercoagulable state result in venous thromboembolism or causing retinal vasculitis secondary to thrombo-inflammatory cascade. Theses mechanisms cause endothelial cell dysfunction, breakdown in the inner blood retinal barrier and increased capillary permeability and subsequent development of macular edema [6]. We reviewed the literature and cannot find a Coats case with a retinal occlusion during the COVID-19 diseases. That is why this case is presented. Case report A 43-year-old male patient came to the consultation to a routine exam for his Coats disease. Coats disease was diagnosed more than 5 years ago and stays in stage 1 with 20/20 visual acuity in both eyes. One week after the routine consultation the patients began with fever and acute respiratory disease. The positive COVID-19 infection was confirmed by a positive polymerase chain reaction analysis of sputum samples. In addition, the patient suffered acute loss of vision in the right eye four days after the beginning of general symptoms (Pic. 1 – see cover page 3).
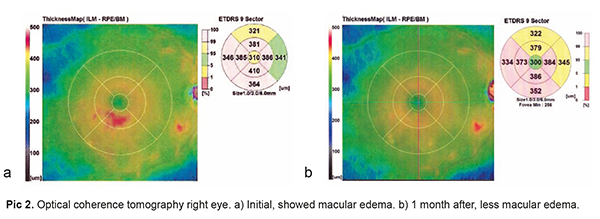
The ophthalmological examination shows a visual acuity of 20/400 in the right eye and 20/20 in the left eye. Biomicroscopy confirmed the anterior segment between normal limits in both eyes. At right eye (RE) fundus examination, tortuosous vasculature, hemorrhages and inferior temporary branch retinal vein occlusion, mild macular edema were shown. The left eye fundus examination was normal (Pic. 2 – see cover page 3).
The optical coherence tomography (OCT) in RE showed predominant inferior and temporary mild macular edema. The fluorescein angiography showed tortuous vasculature intraretinal hemorrhages and leakage of inferior temporary arcade (Pic. 3 – see cover page 3).
The situation was explained to the patients and they signed their informed consent authorizing their treatment. The initial treatment consisted of intravitreal anti-vascular endothelial growth factor injection of aflibercept and periocular injection of triamcinolone. Focal laser treatment on inferior temporary quadrant was done 2 weeks after. Another aflibercept injection was done in the second and third month. In the third month the visual acuity was 20/20 in the eye affected, without hemorrhages neither neovascularization. The OCT showed a normal macular thickness. Discussion Eye autopsy of patients with severe COVID-19 infection has demonstrated a diffuse small vessel thrombosis thought to be caused by complement-mediated microvascular injury, with platelet-fibrin microthrombi regularly found in venules, arterioles, and capillaries.1 Retinal biopsy of 14 deadth patients revealed RNA viral of COVID-19 on 3 of them [1, 7]. Dilated fundus examination on covid-19 patients with retinal occlusions: revealed a hyperemic optic nerve head, macular thickening, tortuous vasculature, and diffusely scattered intraretinal hemorrhages, subtle cotton wool spots and microhemorrhages [1]. The most frequent findings at fluorescein angiography (FA) in these patients are tortuous vasculature, vessel wall staining, neovascularization, leakage, and non-perfusion areas [2]. At OCT, is common to find cystoid macular edema [1]. Marinho did an OCT study on 12 patients during acute stage COVID-19 at a hospital. All patients showed hyper-reflective lesions at the level of ganglion cell and inner plexiform layers more prominently at the papillomacular bundle. Four patients presented subtle cotton wool spots and microhaemorrhages along the retinal arcade [3]. A study has been made on 83 COVID-19 patients. The objective was measure retinal mean venous diameter by OCT. It suggests that the mean venous diameter was maximum at the beginning of the immune response and the inflammatory mediators’ levels are high in blood. The study cannot determine whether the retinal damage is due directly to the direct action of the virus on the retina, or by the patient’s auto immune response [5]. Rayal report a central retinal vein occlusion patient during COVID that was treated with intravitreal antivascular endothelial growth factor injections of bevacizumab [2]. Umed present a branch retinal vein occlusion during a COVID-19 infection that require hospitalization and its FA revealed dilated and tortuous retinal veins in inferior and superonasal quadrants with showed significant vessel wall staining and leakage in late phases suggestive of extensive phlebitis [1]. on this case report the patient was treated with oral methylprednisolone and anti-vascular endothelial growth factor (anti-VEGF) of Ranibizumab [1]. A literature search was conducted and found several studies reporting isolated cases or small series of retinal vascular occlusions during Covid 19 disease. No report of retinal occlusion was found in a patient with Coats disease during his Covid 19 disease. For this reason, it was considered important to recover this case.
References 1.Umed Sheth J, Narayanan R, Goyal J, Goyal V. Retinal vein occlusion in COIV-19: a novel entity. Indian Journal of Ophthalmology. 2020;68(10):2291-3. 2.Raval N, Djougarian A, Lin J. Central retinal vein occlusion in the setting of COVID-19 infection. Journal of Opthalmic Inflammation and Infection. 2021;11(10). 3.Marinho PM, Marcos AAA, Romano AC, Nascimento H, Belfort Jr R. Retinal findings in patients with COVID-19. The Lancent. 2020;395:1609-10. 4.Sunny Ch, Callie KL. Central retinal artery occlusion in patients with COVID-19: imaging for underlying causes. Radiology.2020;300:E315-6. 5.Invernizzi A, Torre A, Parrulli S, Zicarelli F, Schiuma M Colombo V, et al. Retinal findings in patients with COVID-19: results from the SERPICO-19 study. E Clinical Medicine. 2020;100550. 6.Venkatesh R, Gurram Reddy N, Agrawal S, Pereira A. COVID-19 associated central retinal vein occlusion treated with oral aspirin. BMJ Case Rep. 2021;14:e242987. 7.Casagrande M,Fitzek A, Puschel K, Aleshcheva G, Schultheiss HP et al. Detection of SARS-CoV-2 in human retinal biopsies of deceased COVID-19 patients. Ocular Immunology and Inflammation. 2020;28(5):721-25.
Information about authors and disclosure of information Corresponding Author: Dr. Bruno Flores Escobar brnfelm9@gmail.com Author’s contribution: All authors approve the manuscript and agree with what is expressed in it. Funding support: No sponsor was necessary, nor do they have an agreement with any specific brand. Conflict of Interest: Authors do not have conflict of interest in this article.
|