J.ophthalmol.(Ukraine).2016;2:19-22.
|
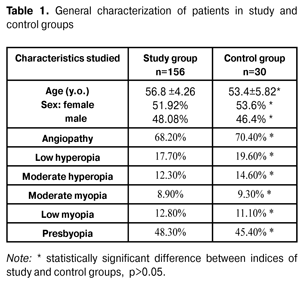
https://doi.org/10.31288/oftalmolzh201621922 Relationship between electroretinogram records and clinical signs in patients with various stages of primary open-angle glaucoma L.M. Stotska, Cand of Sc (Med) I.B. Linnyk-Chokova, Cand of Sc (Med) S.B. Slobodyanyk, Cand of Sc (Med) V.L. Kushnir, MD A.O. Nevska, MD Filatov Eye Disease and Tissue Therapy Institute Odessa (Ukraine) E-mail: odjusa@email.ua Introduction. Lately, a much attention has been paid to studying the retina in patients with primary open angle glaucoma (POAG). The essence of the process has been reported to be an accelerated death of ganglion cells in the retina and retinal axons, comprising the optic nerve, as well as neuroglia, providing optic nerve repair, involved in the pathological process. The purpose of the present paper was to study the relationship between electroretinogram records and clinical signs in patients with various stages of primary open-angle glaucoma. Material and Methods. 358 eyes of 186 patients with POAG and patients with POAG to be confirmed underwent complex clinical and neurophysiological examination at SI “The Filatov Institute of Eye Diseases and Tissue Therapy”. Results. It is known that negative a-wave potential displays response in photoreceptor cells of the outer retinal layer and positive b-wave characterizes bioelectrical activity of the second order neurons of the retina (bipolar cells with possible contributions of horizontal and amacrine cells) and Muller glia cells whilst 30 and more Hz stimulation can be responded by cones only. Therefore, according to our data, initial glaucoma patients have lesions in outer and inner retinal layers as early as initial stages of glaucomatous process. The most apparent pathological changes in neurophysiological process are observed in photoreceptor cells of the outer retinal layer, including cone elements of the retina. Conclusion. As pathological process is growing, more correlations are observed; therefore, pathological changes affect corresponding retinal elements and result in a decrease of differential light sensitivity of the retina, central visual acuity defects, an increase of IOP, and a decrease of optic nerve excavation width; and this is the evidence of pathogenetic character of these neurophysiological alterations in the retina. Key words: primary open-angle glaucoma, electroretinogram, photoreceptor cells, inner retinal layer Background Glaucoma is one of the most common and serious diseases worldwide and at the same time it is one of the most difficult conditions in terms of pathogenesis and diagnostics. A number of scientists tend to believe that a term of “glaucoma” includes a wide range of diseases and conditions, that it is not a separate disease but a group of diseases with similar signs [4]. Until recently, the main signs of glaucoma included changes in the optic nerve head (ONH) and progressing visual field defects. As a rule, the only result of glaucoma is a bilateral irreversible vision loss. Glaucoma is the second cause of complete blindness [6]. Systemic action and local risks play an important role in the development of the disease, but pathological and physiological knowledge of this issue is not enough. The only way to solve the problem is to provide early diagnostics and treatment to overcome risk factors for glaucoma development [1, 9]. Lately, a much attention has been paid to studying the retina in patients with primary open angle glaucoma (POAG). The essence of the process has been reported to be an accelerated death of ganglion cells in the retina and retinal axons, comprising the optic nerve, as well as neuroglia, providing optic nerve repair, involved in the pathological process [3, 7, 8]. The state-of-art clinical methods of investigation, such as scanning laser polarimetry and optical coherent tomography, record structural changes at different levels in the retina and optic nerve [2, 7]. A neurophysiological method of electroretinigraphy is not specific for glaucoma, but it enables to study morphological and functional state of the retina, to detect pathological changes at the term of pre-clinical signs of the diseases [5]; that is of a great importance for studying its pathogenesis and for early diagnostics. Foreign and Ukrainian ophthalmologists have paid a little attention to the role of pathological changes in the retina in the clinical course of the disease in patients with various POAG stages [3, 8]. The purpose of the present paper was to study the relationship between electroretinogram records and clinical scores in patients with various stages of primary open-angle glaucoma. Material and Methods 358 eyes of 186 patients with POAG and patients with POAG to be confirmed underwent complex clinical and neurophysiological examination at SI “The Filatov Institute of Eye Diseases and Tissue Therapy”. 298 eyes of 156 POAG patients with different stages of glaucomatous process comprised a study group including 81 women (51.92%) and 75 men (48.08%). The average age was (56.8±4.26) years old. Depending on the PAOG stage, the patients of the study group were divided into 4 subgroups as follows: subgroup I, pre-glaucoma, 42 patients (84 eyes); subgroup II, initial glaucoma, 48 patients (96 eyes); subgroup III, developed glaucoma, 36 patients (56 eyes); subgroup IV, advanced glaucoma, 30 patients (53 eyes). Patients with absolute glaucoma and high ametropia were excluded from the study. Subgroup pre-glaucoma (suspect glaucoma) consisted of patients, whose findings were not within the normal ranges by one or two indices. We analyzed results of rheoophthalmography, OCT, tonometry, tonography on the presence of interocular asymmetry or daily tonometry data difference of more than 3-4 Mmhg. A control group included 60 eyes of 30 patients without POAG and was comparable in age, sex, ametropia rate, the presence of somatic diseases (Table 1).
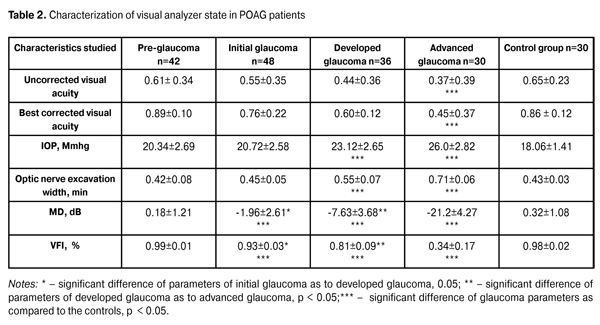
None of patients in the study and control groups had optic nerve disease, macular dystrophy, hypertensive retinopathy, ocular media opacity, diabetes mellitus, craniocerebral trauma, acuit and chronic disorders of cerebral circulation. Each patient underwent examinations as follows: visometry, tonometry, tonography, refractometry, biomicroscopy, direct and reverse ophthalmoscopy, optical coherence tomography by "OPTOPOL" (SOCT Copernicus, Poland), and rheophthalmography. Visual field assessment was performed using Humphrey 750-і Visual Field Analyzer ("Carl Zeiss", the USA) and Central 30-2 test, designed to study the central visual field within 30?. Mean Deviation (dB) (MD) of differential light sensitivity of the retina and Visual Field Index (%) (VFI) were used to assess the presence of visual field defects; the former is the difference between test findings and age norms for each visual field point studied and the latter displays the state of total visual function of patients comparing to age norms and the norm is 100 %. Electroretinography (ERG) responses were obtained using RETIscan electrophysiological diagnostic system (Roland Consult, Germany) to diagnose the presence of pathological process in the retina. We recorded Full-field ERG (Ganzfeld ERG; ffERG) and 30 hz Flicker ERG; the former is mass bioelectrical response of the entire retina and the latter is to test a response arising from the cones. The records obtained were compared to those of the control group and those described in the literature [10], taking into account normal parameters of the ERG system used. Statistic analysis of the data obtained was performed using Statistica 10 software package with calculating mean value, standard deviation, р<0.05 statistical significance (paired test with bilateral distribution), as well as nonparametric Mann–Whitney test, ?-square analysis and Spearman test. Results and Discussion Table 2 demonstrates the data on clinical characteristics of patients of the study group and of the controls as criteria for diagnostics and the disease course. Thus, we observe the significant difference in such characteristics as IOP, optic disc excavation width, MD and VFI parameters in patients with developed POAG and advanced POAG. Significant difference between characteristics of initial glaucoma and developed glaucoma as well as between initial glaucoma and the controls was noted only in computed perimetry data. No significant differences was noted in characteristics between pre-glaucoma and initial glaucoma and between pre-glaucoma and the controls.
We used Spearman's rank correlation coefficient (SRCC) to analyze data on general characteristics and ERG records and revealed correlations between them. According to ERG and computed perimetry (CP) data of suspect glaucoma patients, Spearman's rank correlation coefficient was 0.53±0.009 between local ERG b-wave and MD parameters, –0.48±0.002 between ffERG a-wave and CP MD and 0.56±0.005 between N1- P1 parameters and MD. In initial glaucoma patients, SRCC was equal to 0.32±0.03 between a-wave parameters according to ffERG records and mean deviation differential light retinal sensitivity parameters; and SRCC between flicker ERG Pi1 and VFI parameters was -0.33±0.02. In developed glaucoma patients, SRCC was equal to -0.46±0.01 between ffERG a-wave and IOP parameters, -0.12±0.044 between parameters of ffERG b-wave and ON excavation width, 0.51±0.004 between ffERG b-wave and IOP and 0.41±0.034 between flicker ERG P1 and IOP parameters. No correlation was revealed between ffERG and 30 Hz ERG records and clinical characteristics of visual analyzer functional state in advanced glaucoma patients. It is known that negative a-wave potential displays response in photoreceptor cells of outer retinal layer and positive b-wave characterizes bioelectrical activity of the second order neurons of the retina (bipolar cells with possible contributions of horizontal and amacrine cells) and Muller glia cells whilst 30 and more Hz stimulation can be responded by cones only. Therefore, according to our data, initial glaucoma patients have lesions in outer and inner retinal layers as early as initial stages of glaucomatous process. The most apparent pathological changes in neurophysiological process are observed in photoreceptor cells of the outer retinal layer, including cone elements of the retina. Conclusion Correlations between characteristics of outer retinal layer photoreceptor cells (cones and rods), the second order neurons (bipolar cells with possible contributions of horizontal and amacrine cells) and Muller glia cells and clinical parameters of visual analyzer functional sate was determined in patients with different stages of glaucomatous process using ERG neurophysiological method for the first time in the clinical practice. As pathological process is growing, more correlations are observed; therefore, pathological changes affect corresponding retinal elements and result in a decrease of differential light sensitivity of the retina, central visual acuity defects, an increase of IOP, and a decrease of optic nerve excavation width; and this is the evidence of pathogenetic character of these neurophysiological alterations in the retina. References 1.Zavgorodnyaya NV, Pasechnikova NV. [Primary glaucoma. A new look at an old problem]. Zaporozhzhye. 2010:192. Russian. 2.KachanT., Marchanka L., BirichТ., Dalidovich A., MushtinaT., Verenich A. Comparative study of the optical coherence tomography and scanning laser polarimetry in glaucomatous optic neuropathy diagnosis and monitoring. Oftalmologiia. Vostochnaia Evropa. 2014;4(23):186-91. Russian. 3.Stotska LM, Stotska LS. Peculiarities of chromatic optic canals activity at different stages of primary glaucoma. Oftalmol Zh. 2013;6:22-25. Russian. 4.Choplin NT, Lundy DS. [Glaucoma]. Moscow: Logosfera; 2011. 354 p. Russian. 5.Shamshinova AM, Andreeva TM. [Clinical physiology of vision]. Moscow; 2006. 956 p. Russian. 6.Quigley HA, Broman A. The number of people with glaucoma worldwide in 2010 and 2020. Br. J. Ophthalmol. 2006;90:262–7. 7.Ozturker Zeynep, Sezin Erkul, Dilek Turkmen, Kadir Eltutar. The relationship between central corneal thickness, topographic parameters of optic nerve head and retinal nerve fiber layer thickness in primary angle glaucoma. 11 th EGS Congress. Nice, 2014:139. 8.Valladares AM, Amoros NP, Cortes AC, Morollon JP, Moreno IF. Validity of ganglion cell–inner plexiform layer thickness measurement in the diagnosis of preperimetric glaucoma:correlation with retinal nerve fiber layer thickness. Glaucoma Unit of Albacete, Albacete – Spain. 11 th EGS Congress. Nice, 2014:133. 9.Ammari Wafa, Anis Mahmoud,Sameh Mbarek, Bechir Jelliti, Sana Kochtali,Riadh Messaoud,Moncef Khairallah. Epidemiology and factors of progression of open–angle glaucoma. CHU – Tunisia. 11 th EGS Congress. Nice. 2014. 37. 10.Wu DeZheng, Liu Yan Atlas of testind and clinical application for Roland Electrophysiolodiсal Instrument. Beigind science and technology Press: China; 2006.5–19
|