J.ophthalmol.(Ukraine).2016;4:3-10.
|
https://doi.org/10.31288/oftalmolzh20164310 Efficacy of different amniotic membrane transplantation techniques in patients with inflammatory and degenerative pathology of the cornea E. V. Sereda, a post-graduate student G. I. Drozhzhina, Dr Sc (Med), Prof. T. B. Gaidamaka, Dr Sc (Med) E.V. Ivanovskaia, Cand Sc (Med) V.L. Ostashevskii, Cand Sc (Med) O.N. Ivanova, Cand Sc (Med) B.M. Kogan, Cand Sc (Med) Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine Odessa, Ukraine E-mail: elsereda08@gmail.com
Introduction. Due to its unique properties, amniotic membrane transplantation took its place in reconstructive surgery of ocular surface. The standard technique for amniotic membrane transplantation does not exist. Purpose. To compare the efficacy of different amniotic membrane transplantation techniques in patients with inflammatory and degenerative pathology of the cornea, according to archival patient's cases. Material and Methods. The analysis of 65 archival patient's cases, who underwent amniotic membrane transplantation was made. Three amniotic membrane transplantation technique were used: inlay (graft transplantation), onlay (biological covering), sandwich (combined technique). After the operation, a bandage soft contact lens was put on the corneal surface with fixed amniotic membrane. In the case of amniotic membrane transplantation combined with blepharorrhaphy contact lens was not used. Results. Our study showed high efficacy of amniotic membrane transplantation in patients with different pathologies of the cornea (recurrent pterygium, bullous form of endothelial-epithelial corneal dystrophy), keratitis (bacterial, neurotrophic, autoimmune and herpetic) and corneal burns. In 62 patients (95.4%), positive therapeutic effect was obtained with corneal epithelialization activation, elimination of inflammation and pain, and the absence of pterygium recurrences. It was found that among the patients who had underwent an inlay-technique of amniotic membrane transplantation, the highest efficacy was noted in patients with herpetic and bacterial ulcers. In the group of patients undergone an onlay-technique, the highest efficacy was noted in patients with endothelial-epithelial corneal dystrophy and neurotrophic keratitis and in patients with a sandwich-technique, the highest efficacy was in patients with autoimmune corneal ulcers. Conclusions. There is no one opinion about the best surgical technique of amniotic membrane transplantation. That's why the pilot study on the amniotic membrane transplantation efficacy and the effect on the course of inflammation in the corneal tissue depending on type of its fixation is of scientific and practical interest. Key words: аmniotic membrane, cryopreservation, graft technique, biological covering.
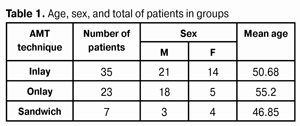
Although the first ophthalmological use of amniotic membrane (AM) took place more than 70 years ago, amniotic membrane transplantation (AMT) has only become of common use in patients with various pathology of the anterior eye segment since 1995 [1-4]. In recent years, due to its unique properties, AMT has taken its place in the reconstructive surgery of the ocular surface. Clinical studies have shown that AMT facilitates epithelialization and epithelial differentiation on the ocular surface [9,11,13]. High level of neurotropic agents makes AM an ideal substrate for ocular surface epithelium reconstruction [15]. Suppression of TGF-beta signaling in corneal and conjunctival fibroblasts in vitro can explain the anti-scarring effect of AM achieved in the treatment of various ocular surface diseases [10]. Hanada К., Solomon A. et al. have shown that in vitro use of AMT decreases the activity of various growth factors and pro-inflammatory cytokines. As a rule, inflammation is reduced significantly after AM transplantation [6,14]. Y. Hao et al have determined that epithelial and mesenchymal cells of AM contain strong antiangiogenic factors: endostatin, thrombospondin-1, and all four Tissue Inhibitors of Metalloproteinase (TIMPs). Besides, AM forms a physical barrier preventing inflammatory mediators and activators of angiogenesis from penetrating in the pathological focus. To date, there is no a manufacturer producing AM for ophthalmic use in Ukraine. Since donor material if of a great deficiency in Ukraine and there is a great number of patients needed to keratoplasty treat (more than a third of patients with keratoplasty indicated), the presence of domestic amniotic membrane can be alternative material for keratoplasty treatment and can significantly improve the quality of surgical service for corneal disease patients. According to the data of the literature, various AMT techniques have been developed and are used for corneal pathology. In persistent corneal epithelial defects, two-dimensional corneal defects, and surface keratitis with depth of 1/3 stromal thickness, AMT can be used as either biological covering of the whole corneal surface with AM episcleral fixation or lamellar AM transplantation with corneal tissue fixation within affected area. Amniotic membrane can be used in various cases as a substrate for affected eye tissue replacing, as a kind of “small patch” (biological dressing), or as their combination [8,12,16]. There is no standard AMT technique. There are a great number of contradictory reports concerning the right way to place the AM on the ocular surface. AM can be sutured to the ocular surface with the epithelial basement membrane facing up and stromal side facing down to the eye (preferred technique) or stromal side of the amnion facing up. The stromal side of the amniotic membrane is sticky similar to vitreous, and the side of the epithelial membrane is shiny and non-sticky. Afterwards, amniotic membrane is carefully distributed on the ocular surface and cut to the required size and form [5,10]. The purpose of the present study was to compare the efficacy of various AM transplantation techniques for inflammatory and degenerative pathology of the cornea according to archival patient cases. Material and Methods Analysis of 2012-2015 archival patient's cases showed that AMT had been performed in 65 patients of Department of Corneal Pathology of the Eye at the Filatov Institute. Amniotic membrane cryopreserved at -196°С (amniotic platex) was obtained from NASU Institute of Cryobiology and Cryomedicine Issues. AMT indications were persistent epithelial defects and corneal ulceration resistant to traditional therapy as well as III-IV stage recurrent pterygium. AMT was performed to stimulate corneal regeneration and corneal surface epithelization, to suppress inflammation and angiogenesis as well as a barrier in pterygium surgery. A total number of patients comprised 42 men (64.6%) and 23 women (35.4%). Patient’s age averaged 51.89 (±17.6 S.D.). AMT success criteria were: 1.Complete corneal surface epithelization 2.Corneal inflammation management 3.Pain management 4.No conjunctivalization of the cornea Surgery was performed using three various techniques: inlay (lamellar transplantation), onlay (biological covering), and sandwich (a combined technique). In all cases, amniotic membrane was placed on the corneal surface with the epithelium side facing up. Preoperatively, the corneal surface was cleaned off necrotic masses and detritus; AM socket was formed in case of deep stromal defects. In all cases, the corneal surface was treated with a preservative and if indicated with anti-inflammatory and antifungal agents. In the inlay technique, 2 to 4 layers of AM were placed on the formed socket and AM was sutured to the defect margin using eight interrupted 10-0 nylon sutures. In some cases AMT was performed in combination with other operations; thus, three patients underwent glaucoma surgery and ptegrium was removed in seven patients. The purposes of operative intervention were medical and tectonic in 19 cases, medical in 9 cases, and barrier in 7 cases. In the onlay technique, AM was placed on the surface of the cornea engaging the limbal area and sutured to episclera using eight interrupted 8/00 silk sutures. In some cases, AMT was performed in the combination with other operations: four patients underwent blepharorrhaphy, two patients underwent glaucoma surgery and one patient was performed lamellar keratoplasty. The purpose of the surgeries was medical in 16 cases and medical and tectonic in 7 cases. The sandwich technique was a combination of the two described above when amniotic graft sutured to the corneal tissue was covered with its AM with episcleral fixation. In one case AMT was combined with blepharorrhaphy. The purpose of the surgeries was medical in 5 cases and medical and tectonic in 2 cases. After surgery, the corneal surface with AM was covered with a bandage therapeutic soft contact lens until complete epithelialization of the corneal surface. In cases when AMT was combined with blepharorrhaphy, soft contact lenses were not used. Table 1 demonstrates the data on the general characteristics of patient in groups.
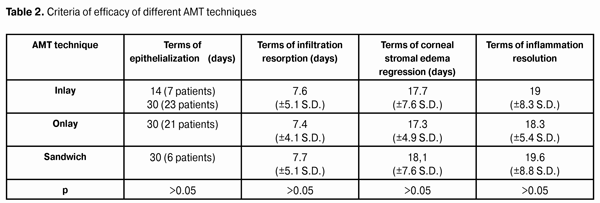
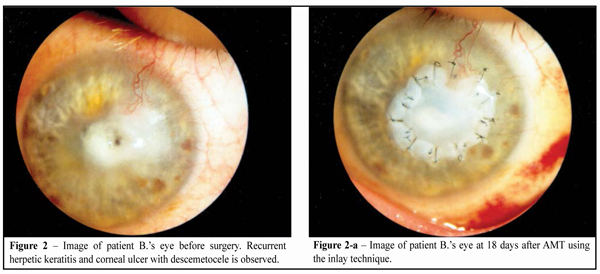
Results The efficacy of amniotic membrane transplantation using the inlay technique (35 eyes) AMT was performed due to such corneal pathologies as follows: recurrent pterygium (n=7), recurrent herpetic keratitis (n=1), and recurrent tuberculous keratitis (n=1), complicated by descemetocele; bacterial keratitis (n=1), and corneal ulcer (n=25). Corneal ulcer etiology was classified as herpetic (n=6), neurotrophic (n=2), autoimmune (n=3), bacterial (n=10), and mixed (n=4). The size of ulcerous defects was 2.0 to 5.0 mm in diameter. Corneal ulcer was complicated by descemetocele formation, perforation of the cornea, and extensive lysis of corneal tissue in 11, 6, and 2 cases, respectively. 10 patients (29%) had concomitant diseases of the eye, among which prevailed myopia and glaucoma (8.6%) as well as dry eye syndrome, cataract, and degenerative vascular opacity. Preop visual acuity equaled light perception with the accurate projection in sixteen patients (47.5%), 0.01 to 0.08 in ten patients (28.4%), 0.1 to 0.5 in four patients (11.6%), and 0.85 to 1.0 in five patients (14.3%). At time of hospital discharge, moderate corneal stromal edema was noted in 14 patients (40%). AM lysis was noted in 5 patients (14.3%) with bacterial corneal ulcer and neuritrophic keratitis. The membrane remained preserved on the corneal surface in 30 patients (85.7%). The membrane was semi-transparent, blurred, and transparent in 30 (85.7%), 3 (8.6%), and 2 (5.7%) cases, respectively. Intraocular pressure (IOP) was within the normal range in all patients during the postoperative period. Early complications noted at terms between 7 days and 3 months after AMT were as follows: perforation of the cornea developed at day 10 after AMT in one pateient with corneal ulcer and presence of purulent exudates in the anterior chamber wherefore he was performed penetrating keratoplasty; lysis of amniotic graft at 3 months was seen in a patient after AMT in conjunction with pterygium removal due to bacterial corneal ulcer development; and AM lysis was noted at 7 days after AMT in a patient with neurotrophic corneal ulcer and descemetocele, wherefore he was performed lamellar keratoplasty. During long-term follow-up period (1.5 years), one patient underwent lamellar penetrating keratoplasty due to the recurrence of herpetic keratitis and development of corneal ulcer with descemetocele. The corneal surface was epithelialized at 14 days after AMT in 7 patients (20%) and at 30 days after AMT in 23 patients (65.7%). AM lysis epitheliopathy was noted in 5 patients (14.3%) at 5 to10 days after AMT. Infiltration of the corneal stroma and stromal edema disappeared at 7.6 (±5.1 S.D.) and 17.7 (±7.6 S.D.) days, respectively. In this group, inflammation signs were reversed at 19 (±8.3 S.D.) days (Table 2). No conjunctivalization of the cornea was noted in all patients.
Thus, according to the study performed, AMT using the inlay technique was most effective for patients with bacterial and herpetic ulcers (Fig. 2, 2a).
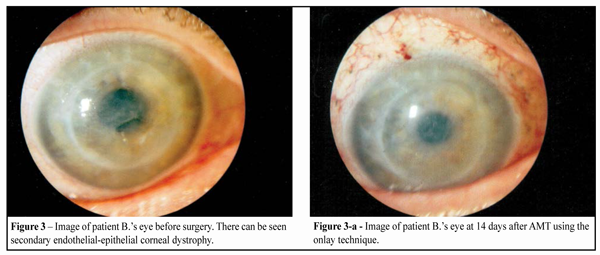
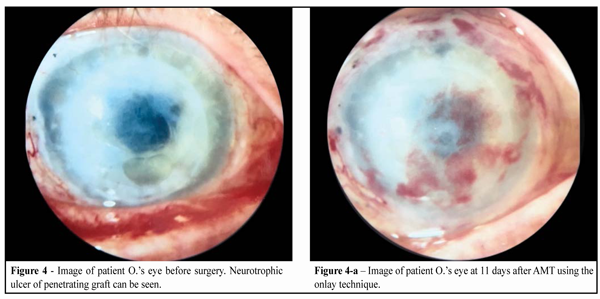
The efficacy of amniotic membrane transplantation using the onlay technique (23 eyes) Corneal pathologies due to which AMT was performed were as follows: bullous endothelial-epithelial corneal dystrophy (n=6); corneal ulcer, chemical burn outcome (n=3); lamellar graft lysis, Lyell's syndrome (n=1); and various keratitis (n=11). Keratitis etiology was classified as herpetic (n=4), neurotrophic (n=5), autoimmune (n=2), and bacterial (n=2). Corneal ulcers were noted in 4 cases including one with micro perforation. 6 patients (26.4%) had concomitant diseases of the eye such as dry eye syndrome, myopia, cataract, glaucoma, and diabetic retinopathy. Preop visual acuity was light perception with the accurate projection in twelve patients (52.2%), 0.01 to 0.06 in ten patients (43.4%), and 1.0 in one patients. At time of hospital discharge, moderate, apparent and no edema was noted in 13 (56.5%), 1, and 9 (39.1%) patients, respectively. Complete lysis of AM was noted in two patients (8.8%) with bacterial corneal ulcer and extensive corneal neurotrophic erosion. The membrane was preserved on the corneal surface in 15 (65.2) patients and was partially lyzed in 6 cases (26.0%). Of these six, in 3 patients there was neurotrophic keratitis as chemical corneal burn outcome and in the rest there was autoimmune keratitis and extensive corneal erosion against the background of epithelial-endothelial dystrophy (EED). The membrane was semi-transparent and transparent in 21 (91.2%) and 2 (8.8%) cases, respectively. Visual acuity at time of hospital discharge was light perception with the correct projection in 15 (65.2%) patients, 0.02-0.06 in 6 (26.0%) patients, and 0.12-0.14 in 2 patients. Thus, vision acuity after AMT increased in 6 (26.0%) patients and decreased in 2 (8.8%) patients. IOP was within the normal range in all patients during the postoperative period. Remote complications developed in 2 cases (8.8%), the first one was perforation of the cornea in a patient with extensive cornial erision against the background of EED at 1 year after AMT wherefore step-by-step penetrating keratoplasty was performed; the second one was bullous changes in a patient with EED of the cornea at 6 months after AMT wherefore AM retransplantation using the onlay technique was performed. Pain management was noted in all patients with EED of the cornea at 2 to 3 days. Complete epithelialization of the corneal surface was noted in 21 (91.2%) patients at 30 days after AMT, epitheliopathy was noted at 5 to 10 days in 2 (8.8%) patients with AM lysis. Infiltration of the corneal stroma and stromal edema disappeared at 7.4 (±4.1 S.D.) and 17.3 (±4.9 S.D.) days, respectively. Inflammation signs were reversed in this group at 18.3 (±5.4 S.D.) days (Table 2).
Thus, according to the study performed, AMT using the onlay technique was most effective for patients with endothelial and epithelial dystrophy of the cornea (Fig. 3, 3a) and neurotrophic keratitis (Fig. 4, 4a)
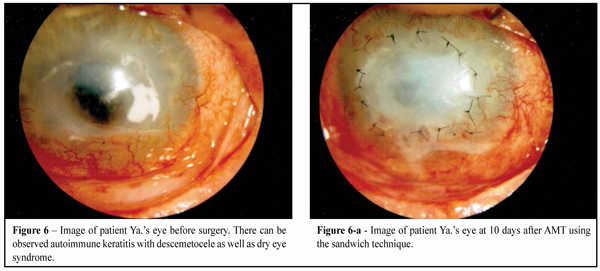
The efficacy of amniotic membrane transplantation using the sandwich technique (7 eyes) Among corneal pathologies due to which AM transplantation was performed prevailed autoimmune keratitis (85.7%). 1 patient (14.3%) had bacterial corneal ulcer. In two cases ulcers were complicated by the presence of descemetocele. As for concomitant diseases, dry eye syndrome was noted in one case. At time of hospital admission, the visual acuity was equal to light perception with the accurate projection in 5 patients (71.4%) and 0.03-0.5 in 2 patients (28.6%). AM remained preserved on the corneal surface in 6 patients (85.7%). Complete lysis of the membrane was noted in 1 patient with Lyell's syndrome and corneal ulcer. AM was blurred in one patient and semi-transparent in 6 patients (85.7%). At the time of discharge, visual acuity was equal to light perception with the correct projection in 4 patients (57.1%), 0.02-0.07 in 2 patients (28.6%), and 0.2 in 1 patient. Thus, visual acuity after AMT increased in 2 patients and decreased in 1 patient (14.3%). IOP at the postoperative period was within the normal range. At 2 weeks after AMT in the Lyell's syndrome and corneal ulcer patient there was noted AM and the natural cornea lysis with corneal perforation development, due to which he was performed penetrating keratoplasty with graft covering with the conjunctiva and blepharorrhaphy. At the long-term follow-up period, autoimmune keratitis was recurrent in one patient with Lyell's syndrome; therefore penetrating keratoplasty in conjunction with corneal ulcer blepharorrhaphy was performed. Corneal surface epithelialization was achieved at 30 days in 6 patients (85.7%). Corneal erosion due to AM lysis was noted at 14 days in one patient. The infiltration of the corneal stroma and stromal edema disappeared at 7.7 (±5.1 S.D.) and 18.1 (±7.6 S.D.) days, respectively. Inflammation signs were reversed in this group at 19.6 (±8.8 S.D.) days (Table 2). Thus, according to the study performed, AMT using the sandwich technique was most effective for patients with autoimmune corneal ulcers (Fig. 5, 5a, 6-6a)
It should be noted that ulcerous defects of the cornea in patients with autoimmune keratomalacia were of irregular shape: semilunar, oval, or triangular when horizontal size was greater than vertical. In such patients, due to membrane flexibility, the use of AM transplantation made it possible quite easy to model the amnion graft according to the shape and size of the defects, not touching the healthy tissue of the cornea.
Conclusion The present study revealed the high efficacy of AM transplantation in patients with variable ocular surface diseases including recurrent pterygium, bullous form of endothelial-epithelial dystrophy of the cornea, bacterial, neurotrophic and autoimmune keratites, and corneal burns. Positive therapeutic effect was achieved in 62 patients (95.4%) regardless of diseases etiology; acceleration of corneal surface epithelialization, inflammation and pain management, and the absence of pterygium recurrence were noted. It should be noted that the inlay technique was most effective for bacterial keratitis and pterygium patients, the onlay technique was most successful for patients with neurotrophic keratitis and endothelial-epithelial dystrophy of the cornea, and the sandwich technique was most effective for autoimmune keratitis patients. Since there is no common opinion on AMT surgical techniques to date and there are a great number of contradictory papers on the optimal technique, experimental research on studying the efficacy of AMT effect on the course of inflammation depending on its fixation type is of great scientific and practical interest.
References
|