J.ophthalmol.(Ukraine).2016;5:14-17.
|
https://doi.org/10.31288/oftalmolzh201651417 High-frequency electric welding of biological tissues versus diode laser photocoagulation as intraoperative retinopexy in vitrectomy for rhegmatogenous retinal detachment N.N. Umanets, Cand Sc (Med) Filatov Institute of Eye Diseases and Tissue Therapy, NAMS of Ukraine Odessa, Ukraine E-mail: n.umanets@mail.ru
Background: It is important to find an alternative retinopexy technique allowing for the exclusion of silicone oil (or gas) tamponade of the vitreous cavity from the vitrectomy procedure for rhegmatogenous retinal detachment (RRD). Materials and Methods: A retrospective non-randomized study was conducted and included 112 patients (112 eyes) with uncomplicated RRD. Retinopexy in the study group (53 patients, 53 eyes) and in controls (59 patients, 59 eyes) was performed using high-frequency electric welding of biological tissues (HFEWBT) and 810-nm laser irradiation, respectively. Results: Mean visual acuity increased to higher levels in the HFEWBT group than in controls at 2 months (0.29 versus 0.21, P = 0.035; this is due to the fact that we managed to avoid intraoperative tamponade in 30% of patients of the study group, thus enabling maintenance of clarity of the posterior lens capsule) and 12 months (0.41 versus 0.39, P > 0.05). Conclusions: High-frequency electric welding of biological tissues (a) is a safe and efficient method for obtaining a firm chorioretinal adhesion, (b) can be used in the clinical practice for intraoperative retinopexy at the time of vitrectomy in patients with uncomplicated RRD, and (c) can ensure retinal re-attachment at the long-term follow-up in as much as 96% of such cases. Key words: high-frequency electric welding of biological tissues, retinal detachment, vitrectomy
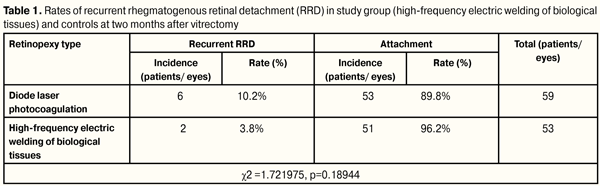
Introduction Retinal detachment is a severe ocular disorder resulting in a loss of visual function. Rhegmatogenous retinal detachment (RRD) incidence has been reported to be between 6.3 and 17.9 per 100,000 [1]. Vitrectomy is the most efficient treatment for RRD, and involves the removal of the altered vitreous gel, flattening the retina, performing retinopexy to prevent retina from tearing away, and filling the vitreous cavity with a tamponading agent [2-4]. The most common type of retinopexy is laser photocoagulation [5]. Given the fact that formation of a firm chorioretinal scar requires approximately 10 days after laser photocoagulation, a tamponade of the vitreous cavity is essential for the creation of chorioretinal adhesion [6-8]. In current clinical practice, expansile gas/air mixtures of various concentrations and silicone oils of different densities are used as an ocular endotamponade [9-10]. Although the tamponade force exerted by the gas against the retina is high, its effect is limited in time, and any re-detachment will require an urgent surgical treatment. The use of gases is limited in children and in patients with severe systemic diseases having difficulties with maintaining a specific position of the body for a long postoperative period. In addition, flying or traveling to high altitudes is contraindicated while the gas bubble is present in the eye [11]. Silicone oil as a tamponade agent in RRD patients, however, also has some disadvantages. Not only the tamponade force exerted by silicon oil against the retina is comparatively low, but the patient requires an additional procedure for the removal of this oil from the eye [12]. Moreover, perisilicone proliferation, secondary ocular hypertension, cataract progression and degenerative ocular changes are frequent following silicone oil endotamponade [13]. Therefore, it is important to find an alternative retinopexy technique allowing for an immediate and firm chorioretinal adhesion as well as for the exclusion of silicone oil (or gas) tamponade of the vitreous cavity from the vitrectomy procedure. We have previously found experimentally that (1) high-frequency electric welding of biological tissues (HFEWBT) with upgraded high-frequency current generator EK- 300M1 can be used for retinopexy, and (2) exposure of the chorioretinal complex to electric current (voltage, 14-16 V; current, up to 0.1 A; frequency, 66.0 kHz; exposure time, 1.0-2.0 s) results in a two times higher chorioretinal adhesion compared that achieved with diode endolaser photocoagulation in the presence of the vitreous [14-15]. In addition, we have established optimal current patterns for achieving similar effects in the clinical setting in the presence of various substances (air, perfluorodecalin) in the vitreous cavity [16]. The study purpose was to compare the efficacy (i.e., anatomic and visual outcomes) of vitrectomy with HFEWBT retinopexy versus vitrectomy with diode endolaser photocoagulation for rhegmatogenous retinal detachment. Materials and Methods A retrospective non-randomized study was conducted and included 112 patients (112 eyes) with uncomplicated RRD. Retinopexy in the study group (53 patients, 53 eyes) and in controls (59 patients, 59 eyes) was performed using high-frequency electric welding of biological tissues (HFEWBT) and 810-nm laser irradiation, respectively. Exclusion criteria were single eye patients, presence of giant retinal tears, disinsertion from the ora serrata, or retinal detachment in both eyes. The mean duration of RRD was two weeks. Baseline visual acuity was accurate projection of light to 0.1. Pneumotonometry readings ranged from 16.0 to 20.0 mmHg. Patients were divided into two groups, Group 1 (HFEWBT retinopexy) involving 53 patients (53 eyes; 33 women (62.3%) and 20 men (37.7%); mean age, 55.1±10.9 years) and Group 2 (810 nm endolaser retinopexy; controls) involving 59 patients (59 eyes; 31 women (52.5%) and 28 men (47.5%); mean age, 57.7±10.3 years). Preoperative examination included autokeratorefractometry, pneumotonometry, visual acuity assessment (using the modified Shevalev’s Charts), biomicroscopy, ophthalmoscopy, and perimetry. Each patient underwent a 20G three-port subtotal pars plana vitrectomy with the use of a wide-field OMS-800 OFFISS (Topcon, Japan) operating microscope. Surgical technique After subtenon anesthesia (5.0 mL of 2% lidocaine hydrochloride), conjunctivotomy was placed in the superior temporal, superior nasal, and inferior temporal quadrants of the ciliary body, and sclerotomy was performed. An irrigation cannula was inserted through the inferotemporal sclerotomy and secured in place with a “U” suture. A core vitrectomy was performed at 1500-2500 cuts/min and at vacuum level of 400-600 mm Hg. This was followed by excision of the posterior hyaloid over 360?. Subsequently, a peripheral vitrectomy was performed (2500-5000 cuts/min; vacuum level, 150-250 mm Hg) with scleral depression. Pneumohydraulic reattachment of the retina was achieved in the control eyes. Two or three rows of endolaser photocoagulation burns were placed around the retinal tear in a confluent fasion. Gas/air mixture (20% SF6 or 30% C3F8) was used for endotamponade of the vitreous cavity. In the HFEWBT retinopexy group, our proprietary retinal flattening method (patent of Ukraine) with perfluorodecalin was used intraoperatively to facilitate complete drainage of subretinal fluid. Intraoperative retinopexy was performed by applying spot burns of up to 1 mm sequentially in two rows along the edge of the retinal tear. Thereafter, perfluorodecalin was removed and replaced for a balanced salt solution. The adequacy of the chorioretinal adhesion formed along the edge of the retinal tear was examined intraoperatively. If the adhesion was adequate, no intraoperative endotamponade of the vitreous cavity was performed. Otherwise, fluid-gas exchange and tamponade of the vitreous cavity was performed at the site of a break in the adhesion, with sterile air, and either 30% SF6 or 20% C3F8, depending on the break location, used as a tamponade agent. Results Patients of Group 1 were comparable to those of Group 2 in terms of baseline clinical and functional status, with best corrected visual acuity ranging from accurate projection of light to 0.1. Given a substantial difference in baseline visual acuity among patients, they were divided into four visual acuity categories as follows: (1) accurate projection of light (8 patients of Group 1 and 9 patients (15.1%) of Group 2); (2) accurate projection of light to 0.1 (23 patients (43.4%) of Group 1 and 31 patients (52.5%) of Group 2); (3) 0.1 to 0.3 (13 patients (24.5%) of Group 1 and 9 patients (15.3%) of Group 2); and (4) 0.3 to 1.0 (9 patients (17.0%) of Group 1 and 10 patients (16.9%) of Group 2). At baseline, the mean visual acuity in Group 1 was 0.16 (0.06), and in Group 2 was 0.17 (0.04), with no statistically significant intergroup difference (P = 0.63). The extent of detachment was 1, 2, 3 and 4 quadrants in 6 patients (11.3%), 16 patients (30.2%), 17 patients (32.1%), and 14 patients (26.4%), respectively, of Group 1, and in 3 patients (5.1%), 14 patients (23.7%), 9 patients (15.3%), and 33 patients (55.9%), respectively, of Group 2 (P = 0.011). Macula detachment was present in 37 patients (69.8%) of Group 1 and 47 patients (79.7%) of Group 2 (P = 0.22). Retinal breaks were located superiorly and anteriorly in 26 patients (49.1%) and 27 patients (50.9%), respectively, of Group 1 and in 39 patients (66.1%) and 20 patients (33.9%), respectively, of Group 2 (P = 0.068). Mild lens opacity, aphakia and IOL were present in 49 patients (92.5%), 1 patient (1.9%), and 3 patients (5.7%), respectively, of Group 1, and in 48 patients (81.4%), 2 patients (3.4%), and 9 patients (15.3%), respectively, of Group 2 (P = 0.21). Vitrectomy resulted in a complete retinal attachment in all cases (112 eyes), and no intraoperative complications were observed in any patients treated. Operating time ranged from 30 minutes to 50 minutes. It is noteworthy that we managed to exclude intraoperative tamponade in 19 patients (35.8%) of Group 1. During postoperative days 1-3, local retinal detachment secondary to adhesion failure was observed in 2 of these cases, which required for fluid-gas exchange with 20% С3F8. The adhesion failure along the edge of the retinal tear was observed intraoperatively in 34 patients (64.2%), which required the tamponade with sterile air, 20% С3F8 and 30% SF6 in 4 eyes (7.5%), 20 eyes (37.7%), and 10 eyes (18.9%), respectively. At day 1 after surgery, the visual acuity in non-endotamponade patients and endotamponade patients of Group 1 was 0.1 to 1.0 and accurate projection of light, respectively. At the end of vitrectomy, tamponade of the vitreous cavity with a gas-air mixture, including either 20% С3F8 or 30% SF, was performed in all patients of Group 2 (47 eyes (74.5%) and 12 eyes (25.5%), respectively); in these eyes, mean visual acuity at the discharge was accurate projection of light. At the 2 month follow-up, retinal re-attachment and recurrent retinal detachment was observed in 51 eyes (96.2%) and 2 patients (3.8%), respectively, of Group 1, and in 53 eyes (89.8%) and 6 patients (10.2%), respectively, of Group 2, with no statistically significant intergroup difference (P = 0.18) (Table 1).
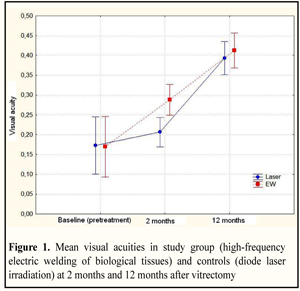
Patients with recurrent RRD underwent reoperation for RRD, with removal of epiretinal membranes, flattening the retina with sterile air, and diode endolaser photocoagulation of the edges of retinal tears with subsequent tamponade of the vitreous cavity with 20% С3F8. Subsequently, at the follow-up visits over a 12-month period, consistent improvement in anatomic outcome was demonstrated in 52 patients (98.1%) of Group 1, and in 59 patients (98.3%) of Group 2. Mean visual acuities (vision of light perception or better) in two RRD groups at baseline (preoperatively), at 2 months and at 12 months after vitrectomy are presented in Fig. 1. Fig. 1 demonstrates that, in spite of similar baseline visual acuities among the two groups, at 2 months after vitrectomy, the mean visual acuity in Group 1 was 0.29±0.02, and in Group 2 was 0.21±0.02, with a statistically significant intergroup difference (P = 0.035). At 12 months, visual acuity in Group 1 and in Group 2 improved to 0.41±0.02 and 0.39±0.03, respectively, and the improvement was statistically significant, although the intergroup difference at this time point was not statistically significant (P = 0.61). Most probably, the intergroup difference in visual acuity at 2 months was associated with a lower rate of cataract in eyes undergoing high-frequency electric welding of biological tissues. As it was mentioned, we managed to exclude intraoperative tamponade in 30% of patients of Group 1, thus enabling maintenance of clarity of the posterior lens capsule.
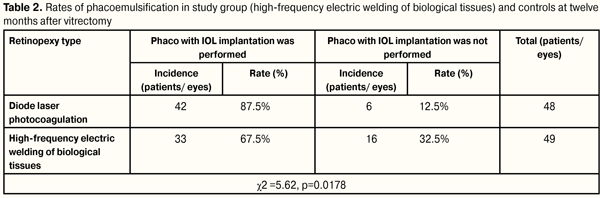
We analyzed the frequency of performing phacoemulsification in the study groups (Table 2). Table 2 demonstrates that during 12 months of follow-up, phacoemulsification was performed in patients of Group 2 more often than in those of Group 1 (42 eyes (87.5%) versus 33 eyes (67.5%)), and the difference was statistically significant (P = 0.017).
Conclusions First, high-frequency electric welding of biological tissues (a) is a safe and efficient method for obtaining a firm chorioretinal adhesion, (b) can be used in the clinical practice for intraoperative retinopexy at the time of vitrectomy in patients with uncomplicated RRD, and (c) can ensure retinal re-attachment at the long-term follow-up in as much as 96% of such cases. Second, at 2 months and 12 months after vitrectomy with high-frequency electric welding of biological tissues for RRD, mean visual acuity improved to 0.29 and 0.41, respectively, which is better than after vitrectomy with diode laser photocoagulation (0.21 and 0.39, respectively), although the intergroup difference at 12 months was not statistically significant. Last, the use of with high-frequency electric welding of biological tissues for retinopexy provided for the exclusion of gas/air mixture tamponade of the vitreous cavity from the vitrectomy procedure in 30% of RRD cases, thus enabling a 20% reduction in the frequency of performing phacoemulsification. References 1.Mitry D, Charteris DG, Fleck BW, et al. The epidemiology of rhegmatogenous retinal detachment: geographical variation and clinical associations. Br J Ophthalmol. 2010 Jun;94(6):678-84 2.Kovalev AI. [Transvitreal surgery for prevention and treatment of traumatic retinal detachments: clinical studies]. [Cand Sc (Med) Thesis]: Odessa: Filatov Institute of Eye Disease; 1987. 194 p. Russian 3.Shishkin MM, Kulikov AN, Churashov SV. [Modern vitreous and retinal detachment surgery]. In: [Danilichev VF, editor. Modern ophthalmology: A guide for doctors]. St Petersburg: Piter; 2000. p340-86. Russian 4.Heimann H., Bartz-Schmidt KU, Bornfeld N, et al. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment: a prospective randomized multicenter clinical study. Ophthalmology. 2007 Dec;114(12):2142–54 5.Smiddy WE, Hernandez E. Histopathologic results of retinal diode laser photocoagulation in rabbit eyes. Arch Ophthalmol. 1992 May;110(5):693-8 6.Zauberman H. Tensile strength of chorioretinal lesions produced by photocoagulation,diathermy, and cryopexy. BrJOphthalmol. 1969;53:749-752 7.Kita M, Negi A, Kawano S, et al. Photothermal, cryogenic, and diathermic effects of retinal adhesive force in vivo. Retina. 1991;11(4):441-4. 8.Yoon YH, Marmor MF. Rapid enhancement of retinal adhesion by laser photocoagulation. Ophthalmology. 1988 Oct;95(10):1385-8 9.Chang S, Lincoff HA, Coleman DJ, et al. Perfluorocarbon gases in vitreous surgery. Ophthalmology. 1985 May;92(5):651-6 10.Hilton GF, McLean EB, Brinton DA, Eds. Retinal Detachment: Principles and Practice. 2nd ed. American Academy of Ophthalmology: San Francisco; 1995 11.Lincoff H, Weinberger D, Stergiu P. Air travel with intraocular gas. II. Clinical considerations. Arch Ophthalmol. 1989 Jun;107(6):907-10 12.Charles S. Vitreous microsurgery. Baltimore: Williams & Wilkins; 1987 13.Honavar SG, Goyal M, Majji AB, et al. Glaucoma after pars plana vitrectomy and silicone oil injection for complicated retinal detachments. Ophthalmology. 1999 Jan;106(1):169-76 14.Pasyechnikova N, Rodin S, Naumenko V, et al. Pilot experimental investigation of the electric welding for the retinopexy . 9th EURORETINA congress, 5-7 May, 2009, Nice, France 15.Pasyechnikova NV, Umanets NN, Artemov AV, et al. [High-frequency electric welding of the tissues of the eyeball posterior part (modified generator EK-300M1) with the application of the original mono- and bipolar set of instruments]. Oftalmol Zh. 2012;2:45-9 16.Umanets NN, Pasyechnikova NV, Naumenko VA, Ptashchenko FA. [Determination of electric current threshold parameters for high-frequency electric welding of the retina in experiment and based on two-dimensional numerical simulation depending on the intraocular contents (vitreous, perftordekalin, air)]. Oftalmol Zh. 2013;5:83-8
|