J.ophthalmol.(Ukraine).2018;1:26-30.
|
https://doi.org/10.31288/oftalmolzh201812630 Howell Modified Test for qualitative and quantitative assessment of near phoria A.V. Kriuchko, ophthalmologist Optic Rehabilitation Center OKTAR; Poltava (Ukraine) E-mail: lkkz@ukr.net TO CITE THIS ARTICLE: Kriuchko AV. Howell Modified Test for qualitative and quantitative assessment of near phoria. J.ophthalmol.(Ukraine).2018;1:26-30. https://doi.org/10.31288/oftalmolzh201812630 Introduction. During a routine optometric examination, much attention is paid to a state of accommodation, convergence, and their interaction. Purpose. To improve the Howell test for near phoria with the possibility of qualitative and quantitative assessment of ocular muscle balance for near. Materials and Methods. During a routine optometric examination, 78 patients with mild and moderate myopia were examined for near phoria using the Modified Howell Test (MHT) and the dissociated test with prisms as a control. Results. Mean near heterophoria values were 1.37 ± 0.48 prism diopters by the MHT and 1.39 ± 0.48 prism diopters by the control test with prisms, the difference was insignificant (p<0.05). Normal values of near phoria with complete correction were found in 24.4% of cases. Acceptable values of shifts on either side were found in 30.7% of cases. Exophoria was in 2.6%. Esophoria was found in 42.3% of cases. The absence of differences in examination using the HMT and the control test with prisms was found in 39.8% of cases, taking into account standard deviation of ±1 prism diopters in 68% of cases. Deviation of ±2 prism diopters was found in 23.1%; ±3 and above prism diopters in 8.9%. The means of differences between the tests was 1.03±0.12 prism diopters. Conclusions. The Modified Howell Test can be used for qualitative and quantitative measurements of near phoria during the optometric examination. The phoria tests for near phoria consistently characterize a state of muscular balance of eyes. Key-words: binocular vision, phoria, phoria tests, Howell test Introduction When examining patients with refraction anomalies, it is critical not only to determine visual acuity and refraction but also to assess a state of accommodation, convergence, and a character of binocular interactions. So, accommodative lag and near esophoria are considered to be important factors for myopia progression in childhood [1]. Accommodation assessment tests including assessment of absolute reserve of accommodation, relative volume and reserve of accommodation, dynamic retinoscopy, evaluation of accommodation response using cross grading etc. are quite widely used in a routine optometric practice [4]. Tests for binocular vision assessment are performed in conditions of ‘soft’ or ‘hard’ haploscopy (dissociation). ‘Hard’ dissociation is achieved by means of completely separated visual fields using red and green light filters, the Maddox cylinder; ‘softer’ dissociation is achieved by polarization filters or prisms. Tests without central fixation for both eyes are used to assess motor fusion; sensory fusion is tested using polarization tests with common central fixation for each eye [4]. To implement in the optometric practice phoria assessment tests, especially for near distances, requires certain skills while assessment results are not always definite. Polarization tests for near are rare; that’s why different modifications of the Schober test and the Maddox wing test as well as the von Graefe prism-dissociation test using vertical and horizontal lines are commonly used [4]. Recently, the Howell test has been spread abroad for evaluation of both distance and near phoria [8]. Traditionally, it is a card with a scale with even numbers (in blue) to the left of “zero” and odd numbers (in yellow) to the right. A downward pointing arrow is at the ‘zero’ level [4]. Likewise the von Graefe’s test, to induce dissociation the vertical prism is placed in front of one eye and a shift of the top arrow as to the bottom row shows heterophoria, the value of which is specified by placing a horizontal prism in front of the fellow eye to compensate the shift. The scale numbers are calibrated for the distance of 3 m (test for distance) and 33 cm (test for near) and tentatively determine the value of the compensating prism. According to a number of papers [7, 8], the Howell test is more repeatable than the von Graefe test and gives less exophoric results. However, it is not always convenient to use the Howell test in the practice, which was the reason for its modification. The purpose of the present paper was to modify the Howell test for qualitative and quantitative assessment of near phoria as well as to compare the results of testing the ocular muscle balance for near in patients with mild and moderate myopia using the modified Howell test and the test with compensating prisms.
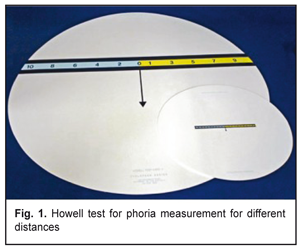
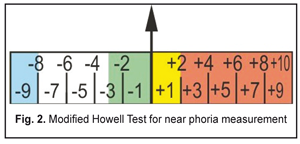
Material and Methods The study included 78 patients (156 eyes), aged 7 to 43 (at average 17±1 years), with mild and moderate myopia, 68 patients (M±m=–1.09±0.09D) and 10 patients (M±m=–4.69±0.29D), respectively, including those aged 7-10 (n=20), 11-17 (n=34), and 18 and over (n+24). There were 33 males and 45 females. It was a prospective, single-center, comparative study. Each patient was performed an optometric examination including visual acuity test; objective and subjective refraction test; evaluation of absolute and relative accommodation reserves; assessment of negative part of relative accommodation and binocular accommodation response; cross-grading test at 40 cm distance (2.5D). The state of vergence was assessed using the modified Howell test (MHT) by numbers on the test scale card placed on the phoropter holder board for near tests; as controls, phoria values of all patients were double-checked using horizontal prisms of the phoropter. Analysis of variance was used to process the data obtained. Results and Discussion The point of the modification for the traditional Howell test was as follows (Figure 2). All brands of modern computer phoropters presented in the Ukrainian market have a dissociating horizontal prism of 6 prism diopters located base up in front of the right eye while the image of the right figure of the test is shifted downwards. To unify the method, when examining with a trial frame, the prism is also recommended to be always placed in front of the right eye base up. In this regard, the arrow in the modified test is upwards.
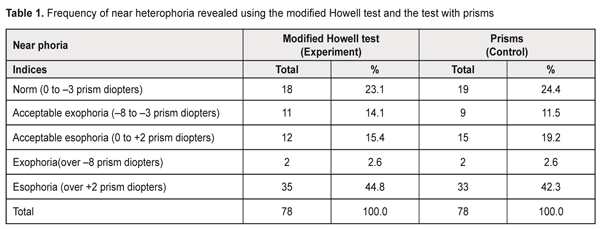
When the image is doubled by the prism, the arrow of the bottom figure points at the scale of the top figure; when heterophoria occurs: positive numbers to the right of zero indicate esophoria, and negative numbers to the left of zero indicate exophoria. The next step of the modification was to highlight in different colors the scale ranges for normal, acceptable, and pathological values. The normative value for near phoria at a 40 cm test distance (2.5D) is exo 3.0 prism diopters ± 5.0 prism diopters [9]. Based on this, the normal values for near phoria were ranged within –3.0 to 0.0 prism diopters and marked in green color on the test’s scale. The acceptable esophoria values were ranged within 0.0 to 2.0 prism diopters and colored in yellow while the acceptable exophoria values were ranged within –3.0 to –8.0 prism diopters and marked in white. The pathological values for esophoria and exophoria were ranged over 2.0 prism diopters (red color) and over -8.0 prism diopters (blue color), respectively. Thus, qualitative assessment of near phoria is available when performing the test, which considerably fastens the further examination. The arrow of the bottom figure pointing at the green scale range indicates the norm, so phoria measurements can be finished by this. The arrow pointing at the yellow or white ranges of the top scale indicates the acceptable values of esophoria and exophoria, respectively, and the further specification of the value using horizontal prisms are left to the specialist’s discretion. The arrow pointing at the red or blue range requires the further specification of the heterophoria values using horizontal prisms base-out and base-in for esophoria and exophoria, respectively. Since these values do not exceed the ranges of 10 prism diopters, the length of the test scale could be shortened, which made it more convenient to use. Finally, the modification concerned the scale of the test card itself. Unlike the traditional test, the exophoria range in our test is marked with negative numbers for perception convenience. Considering the conditions of near phoria measurement at distance of 40 cm (2.5D), theoretically, a test scale pitch of 1 prism dioper must be equal to 4 mm (according to the similarity of triangles rule: 1 prism diopter supposes the point displacement of 1 cm aside at the 1 m distance; at the distance of 0.4 m, this displacement is 0.4 cm). Similar calculation is used, for instance, in the Maddox cylinder test for near. However, when using near phoria compensating prisms, the shift of images is approximately twice less than the computed value. So, Goss DA and colleagues have reported that ‘Morris found an average difference of 1.2Δ more exo when he used 2Δ BO (a 2 prism dioper lens based-out) with the modified Thorington test. The fact that the phoria did not change the same amount as the power of the prism placed in front of the eye might be explained in part on the basis of prism effectivity. Due to prism effectivity, the effect of a prism on eye position for a near point object is less than the labeled power of the prism’ [7]. During the trial application of the new test for near phoria assessment we obtained similar results. This was a reason to decrease a scale graduation interval to 2 mm by 1 prism diopter in the modified Howell test in order to obtain more precise results with compensating prisms. It should be admitted that the issue of scale calibration is still controversial and requires further deep investigation. Eventually, the modified Howell test was placed on the screen for vision testing and on a near test holder board of a computer phoropter. And comparative studies of near phoria with correction were performed in patients with mild and moderate myopia, most of who applied for the first time. Data on near heterophoria revealed are given in Table 1. The values of heterophoria revealed using the MHT and the control test with prisms corresponded to the normal distribution (by the method of percentage deviation of values from standard deviation [2]) so the comparison of groups was carried out according to the paired Student t-test for dependent samples [2].
The mean value (M±m) of near heterophoria was 1.37±0.48 and 1.39±0.48 prism diopers for the MHT and the control prism test, respectively, the difference was insignificant (р<0.05); that is why, hereafter, for describing the detected optical setting of the eyes, we used values of the control test as generally accepted in the optometric practice. The normal values of near phoria with complete correction were observed in 24.4% of cases; the acceptable values on either side were in 30.7%, therefore, the acceptable value of shift of the eyes for near was 55.1%. Exophoria accounted for only 2.6%; in most cases, 42.3%, esophoria was detected. The distribution of near heterophoria due to a myopia degree is given in Table 2.
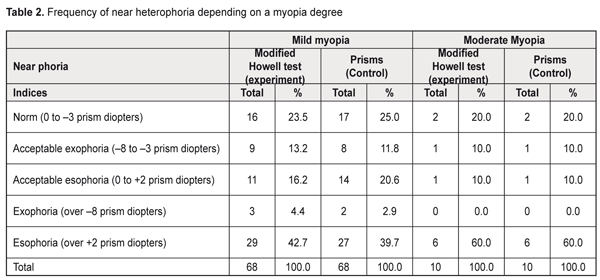
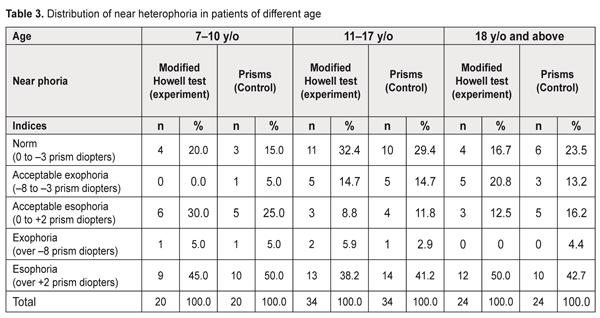
The patients with moderate myopia were more often to reveal clinically significant heterophoria compared to mild myopia, 60% vs. 42.6%, respectively; however, a small-sized sample does not allow for approving these data for sure. Data on near phoria measurement in patients of different age are given in Table 3.
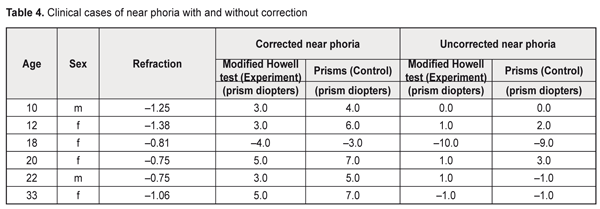
The normal and acceptable values of near phoria are more common with an increase of age (45% for 7-10 years; 50% for 11-17 years; 52.9% for 18 and over, according to the prism test), which can be explained by development of binocular interactions on the growth as well as by more clear answers of the patients with the increase of years. The prevailing type of heterophoria in all the examined was esophoria (50% for 7-10 years, 50% for 11-17 years, 42.7% for 18 and over according to the test with prisms). However, it should be noted that near phoria measurements were carried out with complete correction for distance and most of the patients did not use permanent spectacle or contact lens correction or applied for the first optometric examination. A much lesser value of convergence was noted when measuring near phoria in such patients without correction; that is why when significant abnormalities in the position of the eyes are revealed, near phoria measurement without correction is necessary in order to consider induced esophoria which is known to significantly decrease when wearing spectacles or contact lenses. As an example, Table 4 demonstrates data on near phoria with and without complete correction in 6 patients of different age with clinically significant heterophoria.
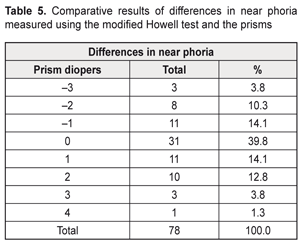
Since the main purpose of the present paper was to compare the proposed modified Howell test to the traditional phoria measurement using prisms, we compared the findings obtained using the two tests in the same patients during the optometric examination. Differences in heterophoria values between the modified and control tests occurred both increasingly and decreasingly and corresponded to the normal distribution law. Grouped data on differences between the two methods are given in Table 5.
Difference with a minus mark means that the control prism test showed lower values of heterophoria than the modified Howell test; a plus sign means heterophoria values were higher when using the control prism test compared to those obtained using the modified test. Totally, the absence of differences was detected in 39.8% of cases; difference with standard deviation of ±1 prism diopter [3] was in 68%. Standard deviation in difference of 2 prism diopters was in 23.1%; 3 and above prism diopters in 8.9%. The mean difference between the tests (M±m) was 1.03±0.12 prism diopters. Since the both phoria measurement tests show a certain difference in the values of the same patient [7, 8], the proposed modified Howell test gives results quite comparable to those of the near phoria measurement using prisms. Conclusion
We propose the modified Howell test for qualitative and quantitative assessment of near phoria to be implemented into the optometric practice; the test can be carried out using both a phoropter and a trial frame with a set of diagnostic prisms. The ability to quickly assess the muscular balance of the eyes using a color test scale for normal, acceptable values, and significant deviations considerably saves the time of the optometrist. The results of the near phoria measurements using the modified Howell test are comparable to those obtained by the traditional test using dissociating vertical and compensating horizontal prisms. References
|