J.ophthalmol.(Ukraine).2018;1:31-35.
|
https://doi.org/10.31288/oftalmolzh201813135 Comparing outcomes of treatments with ETRANS-based electrical stimulation versus electrical phosphene stimulation in patients with accommodative dysfunction Shakir Dukhayer, MD, N.M. Bushuyeva, Dr Sc (Med), V.S. Ponomarchuk, Dr Sc (Med), Prof., N.I. Khramenko, Cand Sc (Med) Filatov Institute of Eye Diseases and Tissue Therapy Odesa (Ukraine) E-mail: bushuyevan@gmail.com TO CITE THIS ARTICLE: Dukhayer Shakir, Bushuyeva NM, Ponomarchuk VS, Khramenko NI. Comparing outcomes of treatments with ETRANS-based electrical stimulation versus electrical phosphene stimulation in patients with accommodative dysfunction. J.ophthalmol.(Ukraine).2018;1:31-5. https://doi.org/10.31288/oftalmolzh201813135
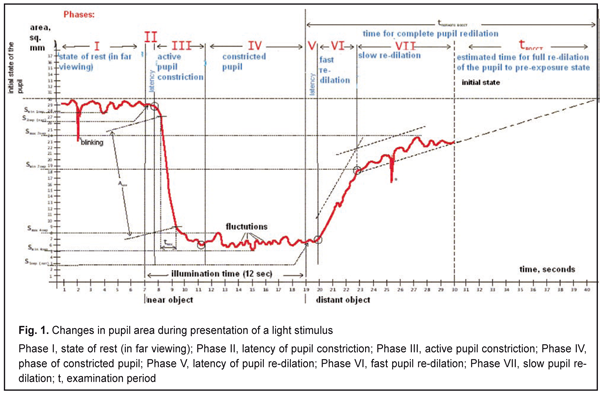
Purpose: To investigate the influence of ocular electrical stimulation (either ETRANS-based or electrical phosphene stimulation (EPS)) on the accommodative, convergence and pupillary system in patients with accommodative dysfunction using objective computerized pupillography. Materials and Methods: Of a total of 59 low myopic children and adolescents with accommodative spasm included in the study, 39 underwent ocular electrical stimulation with the use of ETRANS apparatus, and 20 underwent EPS of the eye. The computerized pupillographer OK-2 was used to obtain images of direct response, consensual response and accommodative convergence response. Results: ETRANS-based electrical stimulation and EPS imposed a unidirectional effect on patients with accommodative dysfunction, with mean percentage improvement in uncorrected visual acuity of 33% and 49%, respectively, and 2.86 times and 4.1 times increases, respectively, in mean accommodative reserve, compared to baseline. In addition, minimum pupil area (after presentation of the stimulus for accommodative convergence), delay in pupillary contraction and active pupillary contraction time decreased by 13%, 10.7%, and 11.5%, respectively, after ETRANS-based electrical stimulation, and active pupillary contraction time decreased by 27% after EPS. Keywords: accommodative dysfunction, low myopia, electrical stimulation, ETRANS, electrical phosphene stimulation, computerized pupillography Introduction Accommodative abnormalities can cause changes in the function of accommodation, convergence and pupillary system [1-6]. Various electrical stimulation techniques (e.g., those of L.E. Cherikchi, V.S. Ponomarchuk, and R. Nagmushi) have been successfully used to treat accommodative dysfunction. It has been demonstrated that along with improvement in visual acuity and increase in accommodative reserves, this approach results also in improvements in light, color and electrical sensitivity of the eye and in ocular blood flow. The authors of these techniques have considered the potential mechanisms of electrical stimulation, in which an improvement in nerve fiber conduction plays a key role. A direct effect of electric stimulation of the eye on the very accommodative, convergence and pupillary response, however, has not been investigated yet. In Ukraine, with the introduction of a domestically produced computerized pupillographer, objective registration of changes in pupillary responses, including the response to accommodative stimulus, has become possible. This allows a clinician to derive a choice of treatment strategy for accommodative dysfunction. The purpose of the study was to investigate the influence of ocular electrical stimulation (either ETRANS-based or electrical phosphene stimulation (EPS)) on the accommodative, convergence and pupillary system in patients with accommodative dysfunction using objective computerized pupillography. Materials and Methods Fifty-nine low myopic patients with accommodative spasm were included in the study. Of these, 39 underwent ocular electrical stimulation with the use of ETRANS apparatus, and 20 children and adolescents underwent EPS of the eye. All patients underwent visual acuity, refractive error and accommodative reserve (AR) measurements, and determination of accommodation and convergence zones with the PORZ apparatus prior to and post treatment. In addition, they had direct ophthalmoscopy and underwent investigation of the tone of autonomous nervous system using Kerdo index. A specially developed computerized pupillographic technique (Information Bulletin No. 4, Declarative Patent of Ukraine №6,231 A61F 9/00 issued 15.04.2005 [6]) was used to investigate pupillary response under the following conditions: continuous video filming duration, 30 seconds; background illumination in the room, 10 lux; distance to the test object ranged from 10 cm (at the near point of accommodative convergence) to 100 cm (with the patient gazing at a far object); test-object (LED) radiation range, 0.5 mW; duration of test-object luminescence at the long-distance point of accommodative convergence, 12 sec; background illumination source, three infra-red LEDs (30 mW) equispaced on a circle at 3 cm from the pupil surface. The methodology of the investigation was as follows: the patient put on a headpiece with IR video cameras, fixed his eyes on a test object located at a distance of 100 cm, and the object was shifted 10 cm and returned to initial position in 10 sec. Video pupillography for each of the two eyes was recorded during this procedure. The percentage measurement error of OK-2 pupillographer was 1%. The pupillary area measurement accuracy was ±0.2 mm2. The measurement accuracy for latency periods of pupil constriction and re-dilation was ±0.05 sec. Figure 1 shows a plot of changes in the pupil area during presentation of a light stimulus.
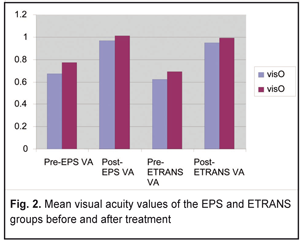
Ponomarchuk and colleagues from the Centre for Eye Function Improvement and Diagnosis of the Filatov Institute, in collaboration with Shtorm Research Institute developed a proprietary-designed therapeutic ocular electric stimulator Fosfen for EPS in 1995. In the current study, the EPS treatment methodology involved the stepwise determination of a phosphene current threshold separately for each patient’s right and left eyes. Transpulpebral electrical stimulation (with an active electrode placed over the centre of the closed eyelid) was performed in both eyes simultaneously using five-pulse trains of 10-ms square-wave pulses with 20-Hz frequency. Both eyes were treated simultaneously, regardless of whether or not the pathological process was binocular. The treatment course consisted of 10 to15 daily 10-minute sessions. Electrical stimulation (with the use of ETRANS apparatus) was performed by the technique of Lebedev [7-8] which had been developed at the Institute for Physiology, St. Petersburg, in 1987, and since then has been successfully used by anesthesiologists, surgeons, otolaryngologists and other medical specialists [7-8]. However, in out ETRANS-based procedure, the current was one half of that used by Lebedev. DC pulses or AC pulses (0.6 mA to 1.5 mA, 78 Hz) of phosphene current threshold were applied to the head electrode (cathode), with two other electrodes (anodes) placed at the mastoid processes behind the ears. The treatment course consisted of 3 daily 15-minute sessions (Information Bulletin No. 1, Declar. Pat. of Ukraine №11,639 A61F 9/00, A61H 31/00 issued 16.01.2006 [9]). Statistical analyses were conducted using Statistica 8 (StatSoft, Tulsa, OK, USA) software. The parametric Student t test was used for unpaired comparisons. The level of significance p ≤ 0.05 was assumed. Data are presented as mean ± standard deviation (SD). Results and Discussion Of the 20 patients (6 boys and 13 girls) of the EPS group, 11 were aged 6 to 9 years, and 9 were aged 10-17 years. Of these 20 patients, 5 were emmetropes, and 5 children had accommodative spasm. Of the rest 10 patients, 9 were low myopes, and one was a low hypermetrope. In the EPS group, the uncorrected far VA (UFVA) and best-corrected far VA (BFVA) far ranged from 0.2 to 1.2 and from 1.0 to 1.2, respectively. In addition, in the right eyes, mean UFVA improved from 0.67±0.35 to 0.91±0.35 after treatment (P = 0.04), whereas in the left eyes, mean UFVA improved from 0.77±0.29 to 1.01±0.29 after treatment (P = 0.01). Furthermore, after treatment, the mean percentage improvement in uncorrected near VA (UNVA) visual acuity was 33% and UNVA varied from 0.9 to 1.0. In the ETRANS group (39 low myopic adolescents with accommodative dysfunction; age, 14 to 18 years), the UCVA for far distance varied from 0.17 to 1.2, and the BCVA varied from 1.0 to 1.2. In addition, in the right eyes, mean visual acuity was 0.62±0.30 before treatment, and improved to 0.95±0.14 after treatment (P < 0.04), and in the left eyes, mean visual acuity was 0.69±0.30 before treatment, and improved to 0.99±0.104 after treatment (P < 0.05). Furthermore, after treatment, the mean percentage improvement in UNVA was 49.2% and UNVA varied from 0.9 to 1.0. Figure 2 presents mean visual acuity values of the groups before and after treatment.
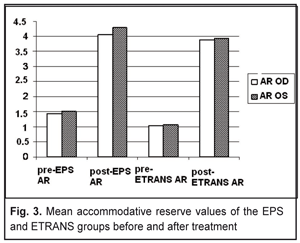
Accommodation reserve (AR) was measured by the technique of Dashevsky. In the EPS group, in the right eyes, mean AR was 1.43 ± 1.37 D before treatment, and improved to 4.06 ± 1.7D after treatment (P = 0.01), and in the left eyes, it was 1.51 ± 1.64 D before treatment, and improved to 4.28 ± 1.96 D after treatment (P = 0.0009). In this group, mean AR increased 2.86 times. In the ETRANS group, in both eyes, mean AR (as measured by the technique of Dashevsky) was 1.05 ± 0.3 D before treatment, and improved to 3.9 ± 0.27D after treatment (P < 0.05); mean AR increased 4.1 times. Figure 3 presents mean AR values of the EPS and ETRANS groups before and after treatment.
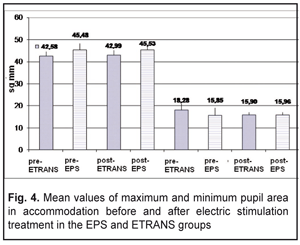
Therefore, both groups demonstrated a beneficial effect of electric stimulation on visual acuity and accommodative reserve. A beneficial effect of 3 daily 15-minute sessions of electric stimulation using the ETRANS apparatus was observed up to 6 months. The computerized pupillographer was used to obtain images of direct response, consensual response and accommodative convergence response, which made it possible to construct relevant response charts. Post-treatment changes in pupillography-derived data (maximum pupillary area, minimum pupillary area (Fig. 4), time of active contraction of the pupil, delay time and pupil re-dilation time (in accommodative convergence after presenting a stimulus) in patients of the EPS and ETRANS groups are of particular interest. The bar chart (Fig. 4) demonstrates mean maximum pupil area (ETRANS group, 42.99±3.04 mm2; EPS group, 45.53±3.45 mm2) and mean minimum pupil area (ETRANS group, 18.28 ±2.24 mm2; EPS group, 15.96±1.97 mm2) during pre-treatment accommodative convergence with the patient’s gaze shifted from the point placed at a distance of 1 m from the patient to the stimulus presented at a distance of 10 cm. In addition, the bar chart demonstrates mean maximum pupil area (ETRANS group, 42.58±2.14 mm2; EPS group, 45.48±2.85 mm2) and mean minimum pupil area (ETRANS group, 15.9±1.68 mm2; EPS group, 15.85±1.48 mm2) during post-treatment accommodative convergence. Therefore, compared to baseline, the mean minimum pupil area during accommodative convergence was found to decrease by 13% (P < 0.05) in the ETRANS group after treatment.
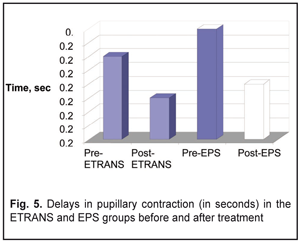
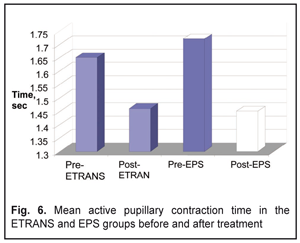
The amount of pupillary contraction latency period (delay in pupillary contraction) needs to be taken into account when illuminating the pupil or when having the patient gazing at a near object with active accommodative convergence. Figure 5 demonstrates data on delays in pupillary contraction before and after treatment. In the ETRANS and EPS groups, delays in pupillary contraction were 0.28±0.05 sec and 0.3±0.06 sec, respectively, before treatment, and decreased by 10.7 % (0.25±0.06 sec, P < 0.05) and by 13.3% (0.26±0.06 s, P < 0.05), respectively, after treatment (Fig. 5). In addition, active pupillary contraction time during accommodative convergence decreased by 11.5 % (P < 0.05) and by 27% (P < 0.05), respectively, after treatment (Fig. 6).
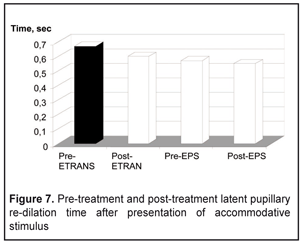
Post-treatment reduction in latent pupillary re-dilation time was more substantial in the ETRANS group than in the EPS group (10% versus 7%, Figure 7).
Therefore, both types of electric stimulation exert a unidirectional effect on pupil area (thus resulting in pupillary contraction) as well as on time-related characteristics of changes in pupillary size, with reductions in pupillary contraction time and pupillary re-dilation time. A negative correlation was observed between amount of accommodative reserve and pupillary width (r = -0.33; P < 0.05) as well as between the former and fusion reserve assessed with PORZ apparatus (r = -0.31; P < 0.05). A positive correlation was found between pupillary re-dilation time and frequency of reductions in pupillary area (r = 0.72; P < 0.05). Conclusion
ETRANS-based electrical stimulation and electrical phosphene stimulation (EPS) imposed a unidirectional effect on patients with accommodative dysfunction. EPS exerts an effect on photoreceptors of the retina and of the optic nerve. The use of ETRANS-based electrical stimulation results in stimulation of Edinger–Westphal nuclei in the reticular formation. After EPS and after ETRANS-based electrical stimulation, mean percentage improvement in uncorrected visual acuity was 33% and 49%, respectively, and mean accommodative reserve increased 2.86 times and 4.1 times, respectively. In addition, minimum pupillary area (after presentation of the stimulus for accommodative convergence), delay in pupillary contraction and active pupillary contraction time decreased by 13%, 10.7%, and 11.5%, respectively, after ETRANS-based electrical stimulation, and active pupillary contraction time decreased by 27% after EPS.
References
|