J.ophthalmol.(Ukraine).2018;3:17-21.
|
https://doi.org/10.31288/oftalmolzh201831721 Changes over treatment in total clinical symptom scores in patients with traumatic keratitis V.M. Sakovych1, Dr Sc (Med), Prof., T.O. Ostrikova2, Ophthalmologist 1 Dnipropetrovsk Medical Academy at the Health Ministry of Ukraine, Dnipro (Ukraine) 2 Dnipropetrovsk Clinical Hospital for Railway Employees, Branch of the PJSC Ukrzaliznytsia’s Healthcare Center Dnipro (Ukraine) E-mail: ostrikovatana@gmail.com TO CITE THIS ARTICLE: Sakovych VM, Ostrikova TO. Changes over treatment in total clinical symptom scores in patients with traumatic keratitis. J.ophthalmol.(Ukraine).2018;3:17-21. https://doi.org/10.31288/oftalmolzh201831721 Background: Since corneal tissue hypoxia develops in patients with traumatic keratitis, investigation of changes over treatment in clinical symptom scores in patients with traumatic keratitis undergoing adjunctive hyperbaric oxygenation (HBO) is of practical value. Purpose: To investigate changes over treatment in clinical symptom scores in patients with traumatic keratitis undergoing adjunctive HBO. Material and Methods: Sixty-nine patients (69 eyes; age, 18 years to 75 years) with traumatic keratitis were included in this study. Patients of the HBO group (33 eyes) received HBO therapy including 40-minute daily sessions in the OKA HBO chamber (operating in the 1.2 ATA mode) for 6 to 10 days as an adjunct in a comprehensive program of keratitis care. Changes over treatment in clinical symptom scores were investigated using the scale we developed. Results: By the end of treatment, in the HBO group, the total mean clinical symptom score was 39.4% lower, and mean scores related to corneal fluorescein staining, corneal edema, inflammatory conjunctival injection and inflammatory infiltration were 40%, 59.09%, 18.2%, and 40%, respectively, lower than in controls (p < 0.01). At the end of treatment, mean BCVA in the HBO group was 30.51% higher than in controls (p < 0.001). Conclusion: The use of adjunctive HBO contributed to substantial improvements in clinical symptom scores and BCVA in patients with traumatic keratitis. Keywords: traumatic keratitis, adjunctive hyperbaric oxygenation
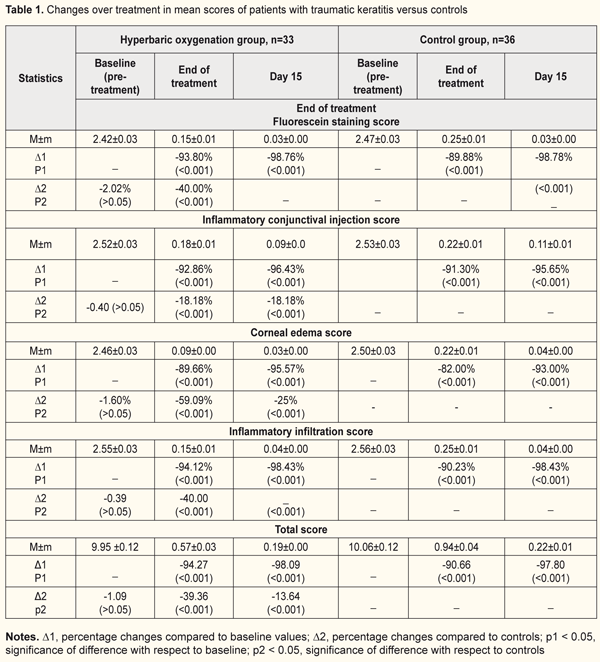
Introduction Ocular trauma and its consequences can result in loss in capacity for labor and are a major contributor to the incidence of disability among young individuals [1]. In Ukraine, the prevalence of ocular trauma was estimated to be 24.5 per 100,000 population and the incidence was found to be high in all the regions [2]. The rate of complications secondary to ocular trauma has been reported to be as high as 22.5% to 30% depending on the age group [2]. Complications (like keratitis, recurrent corneal erosion, corneal opacities and ulcers) secondary to ocular trauma are common despite the use of current treatment strategies [3]. Severe traumatic keratitis usually requires in-patient treatment [4]. Therefore, the treatment strategies for traumatic corneal injuries need further development. Significant changes in etiology of traumatic keratitis due to the wide and uncontrolled use of antibiotics and antibacterial agents for prevention and treatment of the disease, and issues related to drug bioavailability, targeted transport to the pathological site, toxicity and side effects, duration of drug action, stability of formulation under physiological conditions, and inflammation-associated tissue hypoxia necessitate the search for and development of new treatment methods [5, 6]. Hyperbaric oxygenation (HBO) has been reported to be promising for treating inflammations of various origins [8]. HBO therapy not only improves tissue microcirculation and alleviates the consequences of tissue hypoxia, but also positively effects anaerobic conjunctival flora, modulates the immune status, provides sedative effect, enhances tolerance to allergens, activates reparative processes in tissues, and enhances the effect of some medications (including re-epithelizing agents) which allows reducing the dose and duration of treatment. New findings on the methods used to treat keratitis will pave the way to optimized therapy and improved treatment outcomes [7]. The optimum choice of therapy should be based on the patient's clinical characteristics, with strict adherence to laboratory protocol observed to ensure accurate results of specific diagnostic tear fluid tests relevant to the disease. Therefore, the study topic is important because of high prevalence of traumatic keratitis and the need for enhancement of diagnosis and treatment methods. The study purpose was to improve clinical characteristics in traumatic keratitis patients undergoing adjunct oxygenation. Materials and Methods Sixty-nine patients (69 eyes; age, 18 years to 75 years; 70% men and 30% women) with traumatic keratitis were involved in this study. They were divided into the HBO group (33 patients) and the control group (36 patients). All patients received antibacterial therapy, mydriatics, antiallergic agents, tissue therapy, vitamins and Emoxypine. Patients of the HBO group were administered adjunctive HBO therapy over 40 minutes daily for 6 to 10 days. During each 40-minute session, the patient was treated inside the OKA-MT HBO chamber operating in the 1.2 ATA mode. A routine eye examination included visual acuity assessment, slit-lamp biomicroscopy of the anterior segment structures, and ophthalmoscopy. In addition, assessment of corneal re-epithelization through fluorescein staining was performed. Throughout the study, the clinical characteristics were scored. We examined changes in the scores over time in patients of both groups. The scale used for scoring inflammatory response consisted of five categories: inflammatory infiltration, inflammatory injection of the conjunctiva, corneal edema, inflammatory infiltration of the superficial cornea, and corneal fluorescein staining. Categories were scored as follows according to previous studies [3, 4, 8]: Corneal fluorescein staining (0, no local staining; 1, punctate corneal staining, < 1.0 mm in diameter; 2, < 3 mm in diameter; 3, > 3 mm in diameter); Inflammatory injection (0, pale pink conjunctiva, physiologically normal; 1, mild pericorneal injection; 2, moderate pericorneal injection; 3, marked pericorneal injection); Corneal edema (0, no corneal edema and the whole cornea is transparent; 1, local corneal epithelial edema at the inflammation site (mild corneal edema); 2, local epithelial edema with involvement of superficial stromal layers (moderate corneal edema); 3, local edema involving both superficial and deep stromal layers (marked corneal edema)); and Inflammatory infiltrates (0, no infiltration; 1, punctate infiltrates, < 1.0 mm in diameter; 2, < 3 mm in diameter; 3, > 3 mm in diameter). The scores at different time points were included in the medical records. Results The patients in the HBO group demonstrated a corneal fluorescein staining score that was practically similar to that of the controls at baseline (between-group score percentage difference, 2.02%; p > 0.05; Table 1), whereas their post-treatment corneal fluorescein staining scores were better than those of the controls (p < 0.001). Thus, after treatment, in the HBO group, corneal fluorescein staining score decreased by 93.80% (from 2.42±0.03 to 0.15±0.01) compared with a decrease of 89.88% (from 2.47±0.03 to 0.25±0.01) in the controls (p < 0.001), and was 40% lower than in the controls. By day 15 after treatment, re-epithelization was almost complete in both groups (p > 0.05). The mean time for complete resolution of fluorescein staining in the HBO group was 3.22±0.04 days versus 7.43±0.08 days in the controls (p < 0.001).
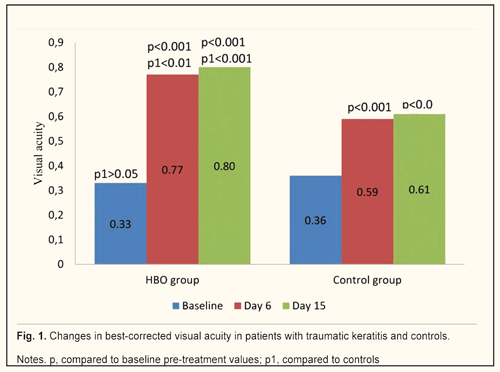
It is noteworthy that, in both groups, corneal edema improved over time. Thus, by the end of treatment, corneal edema score decreased by 93.64% in the HBO group, compared with a decrease of 91.20% in the controls (p < 0.001). Although at baseline, mean corneal edema scores were similar (between-group score percentage difference, 1.06%; p > 0.05), by the end of treatment, mean corneal edema score in the HBO group was 59.09% lower than in the controls (p < 0.001). The mean time for complete resolution of corneal edema in patients treated with HBO was 4.95±0.06 days versus 8.45±0.08 days in the controls (p < 0.05). At baseline, moderate or marked conjunctival injections were present in most affected eyes of both groups, without a significant difference between groups (p > 0.05). By the end of treatment, conjunctival injection score significantly decreased by 92.86% (p < 0.001), from 2.52±0.03 to 0.18±0.01, in the HBO group, and by 91.30% (p < 0.001), from 2.53±0.03 to 0.22±0.01, in the controls. In addition, after treatment, the difference in conjunctival injection score between groups was statistically significant (p < 0.001). The mean time for complete resolution of conjunctival injection in patients treated with HBO was 5.39±0.06 days versus 8.45±0.08 days in the controls (p < 0.05). The data on changes over treatment in inflammatory infiltration scores in patients with traumatic keratitis give evidence for marked corneal inflammation in most patients of both groups. Mean baseline inflammatory infiltration scores were statistically comparable between patients of the HBO group and controls (2.55±0.03 vs 2.56±0.03, p > 0.05). After treatment, in the HBO group, inflammatory infiltration score decreased by 94.12% compared with a decrease of 90.23% in the controls (p < 0.001). Although at baseline, mean inflammatory infiltration scores were similar (between-group score percentage difference, 0.4%; p > 0.05), by the end of treatment, mean inflammatory infiltration score in the HBO group was 40.0% lower than in the controls (p < 0.001). At the end of follow-up (day 15), the difference in inflammatory infiltration score between groups was also statistically significant (p < 0.05). The mean time for resolution of inflammatory infiltrates in the HBO group was 5.87±0.06 days versus 8.79±0.08 days in the controls (p < 0.05). The changes over treatment in total scores for clinical symptoms in patients with traumatic keratitis are evidence of an improvement in the status of the affected eyes in patients of both groups. The improving trend was maintained throughout treatment: corneal fluorescein staining was the only score that was significantly different between the HBO group and controls (2.42±0.03 and 2.47±0.03, respectively) at baseline, whereas by the end of treatment, all the category scores were significantly different between the groups. Mean baseline total scores were statistically comparable between patients of the HBO group and controls (9.95±0.12 vs 10.06±0.12, p > 0.05). By the end of treatment, the mean total scores decreased by 94.27% (to 0.57±0.03) in the former group and by 90.66% (to 0.94±0.04) in the latter group (between-group score percentage difference, 39.36%; p < 0.01). The difference in clinical symptom scores between groups was not statistically significant (p > 0.05). In both groups, mean BCVA gradually improved over treatment (Fig. 1); however, the visual function was significantly better in patients of the HBO group. By the end of treatment, mean BCVA significantly increased by 133.6% (i.e., 2.3-fold; p < 0.001), in the HBO group, and by 63.89% (i.e., 1.6-fold; p < 0.001) in the controls. At day 15, in both groups, no patient had BCVA worse than 0.1. In addition, at day 15, compared to baseline, mean BCVA increased 2.4-fold in the HBO group, and 1.7-fold in the controls (p < 0.001). At the end of treatment, mean BCVA in the HBO group was 30.51% higher than in the control group (p < 0.001).
Direct linear correlations were observed between mean BCVA and objective symptom scores, specifically, inflammatory infiltration score (ґ=0.513, р < 0.05), inflammatory injection score (ґ=0.536, р<0.05), corneal edema score (ґ=0.573, р < 0.05), and corneal fluorescein staining score (ґ=0.593, р < 0.05) in patients of the HBO group. Therefore, our findings demonstrate the clear positive effect of adjunctive HBO on the corneal status in the patients. Conclusion First, by the end of treatment, mean BCVA increased 2.3-fold (p < 0.001) in the HBO group and 1.6-fold (p < 0.001) in the controls. At day 15, mean BCVA was 29.5% higher in the former than in the latter group (p < 0.001). Second, by the end of treatment, mean total scores decreased by 94.27% (to 0.57±0.03) in the former group and by 90.66% (to 0.94±0.04) in the latter group (between-group score percentage difference, 39.36%; p < 0.01). Third, the presence of correlations between improvements in visual acuity and the method of treatment for traumatic keratitis reflects the pathogenetic role of objective symptoms in the pathogenesis of this disease and underscores the need for HBO therapy. Finally, the findings presented support the idea that HBO can be used as a valuable adjunct to conventional therapy for management of traumatic keratitis. References 1.Gundorova RA, Stepanov AV, Kurbanova NF. [Current ophthalmic traumatology]. Moscow: Meditsina, 2007. Russian. 2.Chudniavtseva NA. [Restorative treatment of patients with eye traumas complicated by iridodialysis]. Oftalmol Zh. 2010;1:102-5. Russian. 3.Petrunia AM, Faruk IS. [Efficacy of lypophlavon in the comprehensive treatment for traumatic keratitis]. Oftalmol Zh. 2006;3:102-4. Russian. 4.Sakovich VN, Nikitchina TS, Shcherbakov BD. [Use of phlogenzym in the treatment for herpetic keratitis]. Oftalmologiya. Vostochnaya Evropa. 2012;2:141-5. Russian. 5.Gusova MK. [Toxic damage to the optic nerve secondary to alcohol intoxication]. [Abstract of Cand Sc (Med) Thesis]. Moscow: Russian Medical Postgraduate Education Academy; 2008. 15 pp. Russian. 6.Eliseeva EV. [Hyperbaric oxygenation in ophthalmology: Tutorial]. Karaganda; 2010. Russian. 7.Kuz’minov OD, Lukich VI. [Use of HBO in ophthalmology]. Bul. hiperbaricheskoi biologii I meditsiny. 2001;1-4:76-85. Russian 8.Znamenskaia MA, Rykov SA. [Herperic eye injuries]. In: Znamenskaia MA, editor. [TORCH infections in obstetrics and neonatal care]. Kyiv: Standart Digital Print; 2008. Russian. 9.Beda DI. [Age-related macular degeneration management including the use of hyperbaric oxygenation]. [Abstract of Cand Sc (Med) Thesis]. Krasnoyarsk: State Medical Academy; 2010. 118 pp. Russian 10.Verkman AS. Role of aquaporin water channels in eye function. Exp Eye Res. 2003 Feb;76(2):137-43. 11.Wilson SE, Mohan RR, Mohan RR, et al. The corneal wound healing response: cytokine-mediated interaction of the epithelium, stroma, and inflammatory cells. Prog Retin Eye Res. 2001;20:625-37.
|