J.ophthalmol.(Ukraine).2018;5:49-51.
|
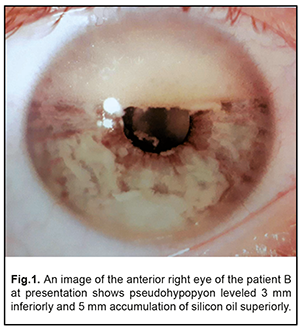
https://doi.org/10.31288/oftalmolzh201854951 Received: 17 August 2018; Published on-line: 26 October 2018 Vitrectomy in an eye with unsuspected retinoblastoma N.F. Bobrova, Dr. Sc. (Med.), Prof.; V.V. Vit, Dr. Sc. (Med.), Prof.; T. A. Sorochynska, Cand. Sc. (Med.); A.V. Artemov, Cand. Sc. (Med.); T.V. Romanova, Cand. Sc. (Med.); T.I. Komarnytska SI “The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine”; Odessa (Ukraine) E-mail: filatov.detskoe7@gmail.com TO CITE THIS ARTICLE: Bobrova NF, Vit VV, Sorochinskaia TA, Artemov AV, Romanova TV, Komarnitskaia TI. Vitrectomy in an eye with unsuspected retinoblastoma. J.ophthalmol.(Ukraine).2018;5:49-51. https://doi.org/10.31288/oftalmolzh201854951 Background. Retinoblastoma (Rb) cases with atypical clinical manifestations, which lead to error diagnosis and inadequate treatment, have become more frequent over the last years. Purpose. To describe and to analyze a clinical picture, diagnostics, and treatment of vitrectomy performed in an eye with unsuspected Rb resulted in pre-operational diagnostic error. Material and Methods. A patient B., aged 5 years 7 months, with unsuspected Rb in the right eye was performed pars plana vitrectomy in local health facilities. Results. After vitrectomy, pseudohypopyon, silicone oil, and cataract were observed in the anterior chamber of the right eye. Ultrasound scanning was not informative due to a shadowing effect of the silicone oil in the vitreous. Fine needle aspiration of pseudohypopyon revealed a great number of cells, supposedly, of retinoblastoma or retinal lymphoma. It was magnetic resonance tomography that could reveal the signs of tumor. The right eye was enucleated. Pathohistological examination showed undifferentiated multifocal Rb with tumor nodules in the optic nerve in equator and with 1-2.0 mm invasion in the choroid in the optic nerve within the cribiform plate. Adjuvant polychemotherapy (carboplatin-etoposide-vincristine protocol) and gamma-ray teletherapy were prescribed to prevent hematogenous metastasis and orbital recurrence of retinoblastoma. Conclusions. Vitreactomy in the eyes with untreated Rb contributes to tumor cell seeding in the numerous eye structures and can affect the survival. Keywords: unsuspected retinoblastoma, vitrectomy, pseudohypopyon, enucleation Retinoblastoma (Rb), a malignant tumor in the retina, is the most common intraocular tumor in children, though it is quite rare in the general clinical practice, occurring in 1 of 15-20 thousand live births [1, 2, 3, 4]. A classic clinical picture of Rb is leukocoria; the presence of a white-grey tumor nidus on the eye fundus with dilated vessels, as a rule, does not cause difficulties in diagnostics. Meanwhile, Rb cases with atypical clinical manifestations, including pseudohypopyon, pseudouveitis, retinal detachment, vitreous opacities and hemorrhages, secondary glaucoma etc., have become more frequent over the last years [6, 7]. Vitrectomy for rhegmatogenous retinal detachment in eyes with Rb has started to be discussed in the literature quite recently; retinal detachments develop more frequently after intraarterial chemotherapy, which is, according to Shields [8], mostly related to rapid tumor regression. A few new publications disquiet by the possibility of tumor recurrence in response to intraocular intervention, even in cases with complete regression of retinoblastoma and when regression has been deemed stable for 6-12 months [9, 10]. Vitrectomy in a case of error diagnosis, i.e. in the presence of active untreated tumor, is described in an extremely small number of observations and raises a major concern due to the possibility of tumor spreading. Having regard to the above, a case of vitrectomy in an eye with unsuspected retinoblastoma, which was under our observation, is of significant scientific and practical interest for understanding the further processes occurring in the eye after surgical intervention. The purpose of the paper was to describe and to analyze a clinical picture, diagnostic and curative measures in a case of vitrectomy which had been performed in the eye with unsuspected Rb due to pre-operational diagnostic error. Material and Methods A child B., aged 5 years and 7 months, having received conservative and surgical treatment (pars plana vitrectomy) in another eye clinic, was urgently hospitalized for suspected Rb at the Pediatric Ophthalmology Department of the Filatov Institute on 6 July 2018. The following procedures were performed: • detailed history taking • analysis of medical records provided • biomicroscopy and ophthalmoscopy in both eyes under general anesthesia • ultrasound scanning of anterior and posterior segments of both eyes • magnetic resonance tomography of the head and both ocular orbits • fine needle aspirate biopsy of the anterior chamber content with cytological examination • enucleation of the affected eye using the technique of high-frequency electric welding (HFEW) of biological tissues [11] which was followed by pathohistological examination to detect the character of tumor, tumor spreading and invasion into the retina, choroid, optic nerve, anterior chamber aqueous humour, iris, ciliary body, anterior chamber angle, vitrectomy ports, episclera, Tenon's space, and orbit • abdominal ultrasound examination • fluorography examination • sternal puncture • lumbar puncture • complete biochemical examination of the peripheral blood • examinations by pediatrician and oncohematologist Results and Discussion The child’s parents noted the occurrence of leukocoria in May 2017 and visual acuity loss was detected in August 2017 by a local ophthalmologist who referred the child with suspected retinal tumor (Coats’ disease) to a clinical center. Thereat, the child was followed up and examined for TORCH infections (negative); the patient received anti-inflammatory treatment with corticosteroids parabulbarly. On 14 December, at the same place, the child was performed subtotal pars plana vitrectomy, partial retinectomy, local endolaser photocoagulation, and silicone tamponade for uveitis in the right eye. According to the discharge record, after floating opacities in the vitreous had been removed, a tumor was revealed in the inferior retina, at 6 o’clock; the tumor was completely removed using partial retinoctomy and thorough endolaser photocoagulation, which was followed by light silicone oil tamponade due to inferior focal location and surgical sites. Postoperative period was within normal limits. A month later, the child was re-examined at the clinical center and fluorescent angiography and retinoscopy revealed no pathological changes. On 7 June 2018, the child’s parents applied to the Filatov Institute due to altered appearance of the operated eye and the child was urgently hospitalized for suspected retinoblastoma at the Pediatric Ophthalmology Department. Clinician-observed: Visual acuity was decreased to light perception with correct light projection; palpatory intraocular pressure was within norm. The right eye was quiet with the transparent cornea; pseudohypopyon as layers of intensively white membranous formations of up to 3 mm was noted at the anterior chamber bottom; the silicone oil was accumulated as small bubbles with a horiantal level of up to 5 mm. The iris had dilated vessels and neovascularization; the pupil was slowly dilated; the lens was opaque in terms of posterior capsule cataract type (Fig. 1); the ocular fundus was not ophthalmoscopically detected.
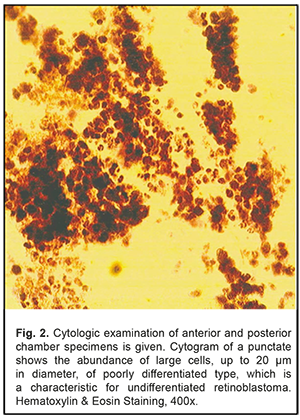
Ultrasound scanning was not informative for understanding the state of the posterior eye due to a shadow effect of the silicone oil in the vitreous. However, along the whole circular length of the posterior chamber and under the ciliary body there were revealed punctuate and fibrous structures of hypo-/iso-echoicity; from the nasal side in the equatorial area, there was a local parietal thickened membranous structure, which, supposedly, was retinal detachment. Taking into accountant the presence of pseudohypopyon on the quiet eye, Rb was suspected although the hypopyon picture was not characteristic for Rb because it was not of a cellular texture. On 12 June 2018, fine needle aspirate biopsy (FNAB) of the anterior chamber content was made. During the intervention, the fibrous membranous formations, which were partially managed to aspirate, kept emerging from the posterior chamber. After the needle had been removed, a small amount of silicone oil escaped from the long corneal tunnel, which could indicate elevated intraocular pressure. Cytological examination of the contents of the anterior and posterior chambers revealed the presence of a great amount of cells (Fig. 2) which were similar to those in retinoblastoma or retinal lymphoma but it was impossible to differentiate them.
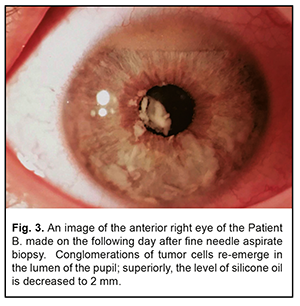
Although white fibrous formations continued emerging from the posterior chamber into the anterior one even in the postoperative period, it was difficult to make a decision on enucleating the eye since the tumor was not visualized (Fig. 3).
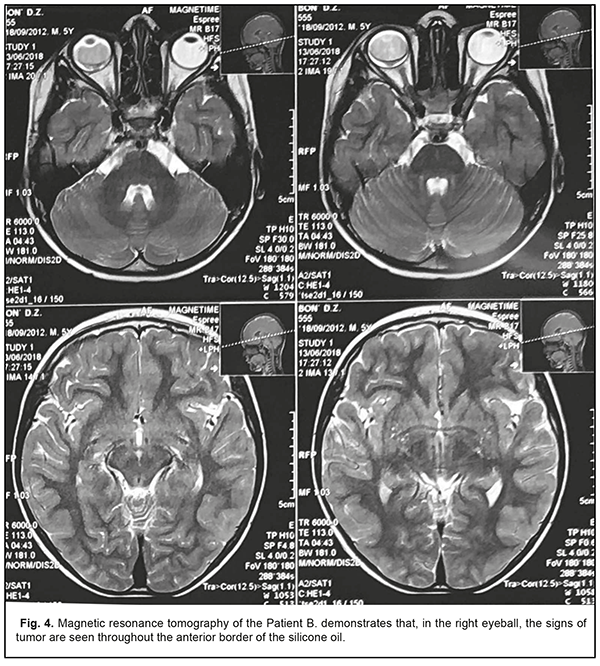
Magnetic resonance tomography, which was performed on 13 June 2018, satisfied the doubts. So, the signs of neoplasm were revealed in the right eye throughout the posterior border of the silicone oil (Fig. 4); the thickness of ocular nerves was similar on both sides (0.5 sm); no focal cerebral changes were revealed.
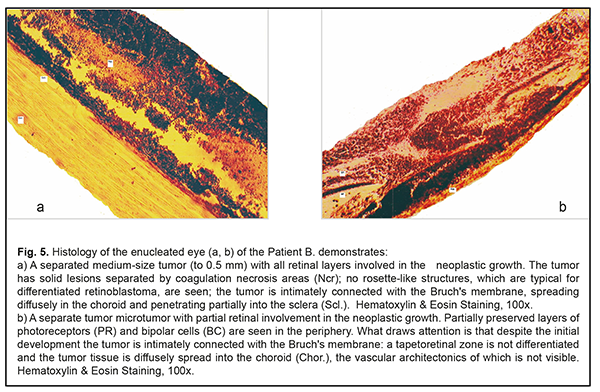
On 14 June 2018, the right eye was enucleated using HFEW of the biological tissues [11] and the implant (Ekoflon, 20.0 mm) was inserted. The surgery and postoperative period were without abnormalities. Pathohistological examination of the enucleated eye showed multifocal retinoblastoma (an undifferentiated type) with the presence of tumor nodules in the optic disc in the posterior and anterior equatorial area; tumor cells implanted into the ciliary processes, anterior chamber angle, and anterior iris surface. The Rb invasion was into the choroid (a 12- mm node) and the optic nerve (within the cribiform plate). No Rb invasion was noted along the vitrectomy ports (Fig. 5 a, b).
General examinations, including general blood test, biochemical blood test, abdominal ultrasound examination, fluorography examination, sternal puncture, and lumbar puncture, showed the absence of pathological abdominal alterations and of metastatic lesion despite a significant space of time (6 months) between vitrectomy and enucleating the Rb eye. Upon consultation with Natali Casoux, President of European Ophthalmic Oncology Group, the child was prescribed polychemotherapy (PCT), a CEV protocol: carboplatin, etoposide, vincristine, to prevent hematogenous metastasis and right orbit gamma-ray teletherapy to prevent orbital growth of retinoblastoma. It was impossible to give simultaneously two treatments since the child had an expressed enterotoxic response to the first course of PCT. Therefore, external irradiation was postponed temporarily. The second and third PCT courses, the CEV protocol with a decreased dose of vincristine, were without complications. The child is followed up and, at the present time, is in good health; the right postenucleating implant is without specific findings (Figure 6).
The most common for Rb is the multifocal growth when blastic lesions appear in more than one site in the retina. According to the direction of RB growth there are endophytic and exophytic patterns of retinoblastoma growth. An endophytic tumor grows forward into the vitreous. An exophytic tumor extends beneath the retina, mainly in the subretinal space and causes retinal detachments. Histological macroscopic examination often reveals both patterns of Rb growth in different sites of the retina. In such cases, the diagnostics is not a problem since ophthalmoscopy and ultrasound scanning examinations reveal one or several “plus-tissue” foci [5]. Rb diagnostics is challenging, as a rule, in so-called infiltrative tumor growth when the tumor cannot be revealed and the retina is displaced and thickened due to retinal tumor cell proliferation [6, 7]. This pattern of Rb growth was, likely, in the case described. In the literature, there are quite poor data on the intraocular tumor extension and life prognosis after vitrectomy in eyes with undiagnosed Rb. Stevenson et al [12] have reported of three patients who referred as months went by after vitreal biopsy in the eyes with unsuspected Rb. In all three cases, enucleation was performed without following adjuvant chemo- or radiotherapy. Afterwards, Rb recurred in all three cases: in the orbit (2 cases) and in the lymph gland (1 case); wherefore aggressive chemotherapy and radiotherapy were assigned. The authors have concluded that preventive therapy is required after enucleation due to extremely poor life prognosis in metastatic Rb. The greatest number of vitrectomy with unsuspected Rb, 11 cases, have been collected and reported by Shields C. Et al [13]. Excluding one three-year-old child, those were children aged from 4 to 16 with monolateral retinoblastoma. Pre-operative diagnoses included vitreous hemorrhage in seven patients, including that with retinal detachment in three eyes; toxocariasis in two patients; toxoplasmosis in one patient; endophthalmitis in one patient. Rb was revealed during vitrectomy in two patients and, as such, single-step enucleation was performed; on cytologic examination of the vitrectomy specimen in eight patients in most cases; and during the follow up visit only in one patient. Thus, the author-reported interval between vitrectomy and Rb diagnosis ranged from 0 to 210 days with the mean interval of 23 days. All eyes with diagnosed Rb were enucleated. Pathohistological examination showed poorly differentiated Rb in ten patients in most cases with mainly an infiltrative pattern of Rb growth in nine patients. Retinoblastoma invasion was recorded in the episclera (two eyes), anterior chamber (seven eyes), iris (five eyes), ciliary body (five eyes), choroid (three eyes), and optic nerve (four eyes). No Rb invasion was noted in the vitrectomy ports, Tenon’s fascia, and orbit. A similar pattern of Rb invasion in the ocular structures was found in our case described. In addition, based on pathohistological examination, although the tumor was completely excised and all vitreous tumor clones were removed, surgical intervention did not result in healing but, contrary, caused internal tumor cell seeding throughout the eye. According to Xun-da JI [14], the rinsing liquid motion in Rb vitrectomy contributes to spread, penetration, and invasion of Rb cells in invisible eyeball portions such as ciliary processes, anterior iris surface despite the complete removal of visible vitreous clones. With the purpose of prophylaxis the authors have recommended to integrate anticancer agents, melphalan particularly, in the content of the vitrectomy rinsing liquid with achieving its certain concentration in the vitreous cavity as well as to give subconjunctival injections of anticancer agents around sclerotomy in order to reduce the risk of tumor cell metastasis. All children after enucleation by Shields C.L. et al [13] were delivered adjuvant treatment consisting in adjuvant polychemotherapy, radiotherapy, or their combination. During the mean follow-up of 7 years (range, 0.2–24 years), 10 children are alive with none experienced metastasis. However, one patient who had referred after the development of metastatic retinoblastoma died 24 months later despite aggressive chemotherapy and radiotherapy. Most Rb cases are known to reveal within the first three years and more frequently between the first and second years. In older children, Rb is less common and is characterized by clinical polymorphism as it was, likely, both in our case and in observations reported by Shields C. et al. [13]. Alongside this, atypical Rb forms can be observed in older children and even in adults. Thus, a case of Rb in a 29-year-old man was described by Kovalevskii et al in 1971 [15]. Taking the patient's medical history, saying that the patient’s daughter had died of belateral Rb, it was possible to make a correct provisional diagnosis and to perform enucleation. Abramson et al. [16] have found that metastasis developed in 5% of cases among the patients diagnosed Rb before the age of 2 while the older patients with Rb, diagnosed between 2 and 7 years, developed metastasis in 19% of cases. The poorest live prognosis, according to authors, was for patients diagnosed between two and seven years both because of late diagnosis and as consequence of a more frequent infiltrative tumor growth pattern which masks a true diagnose. Conclusion It must be admitted that vitrectomy in eyes with untreated Rb precludes from curing tumors but, just the other way round, contributes to intraocular seeding and can affect the survival. Rb can have an atypical clinical picture and be newly diagnosed in older children, which demands heightened “oncoawareness” from ophthalmologists of all professional qualifications. Suspicious and unclear pathological changes in the vitreous and the retina require consultations in a specialized centre to exclude the diagnosis of Rb. In Ukraine, such a center is Department of Pediatric Ophthalmic Pathology in the Filatov Institute where vast clinical experience in ophthalmic diagnosis and treatment of Rb has been gathered for over 70 years.
If, in special cases, intraocular interventions are recommended during the treatment of the eye with suspected ocular tumor, it is necessary to perform urgent cytologic examination of the anterior chamber, subretinal fluid, and vitreous specimens to determine the presence and character of vital tumor cells as well as to reduce the interval between surgical intervention and enucleation of the Rb eye followed by adjuvant PCT and/or radiotherapy in accordance with histopathological findings.Vitrectomy in an eye with unsuspected retinoblastoma
References
|