J.ophthalmol.(Ukraine).2018;5:56-59.
|
https://doi.org/10.31288/oftalmolzh201855659 Received: 29 June 2018; Published on-line: 26 October 2018 Relationship between severity of HIV infection and ocular pathology in patients with pulmonary tuberculosis I.N.Voronova1, V.M. Khokkanen2, S.I. Sanaeva1, M.V. Zhemkova1 1 St Petersburg City Tuberculosis Dispensary; St. Petersburg (Russia) 2 Mechnikov North-West State Medical University; St. Petersburg (Russia) E-mail: anirilas@yandex.ru TO CITE THIS ARTICLE: Voronova IN, Khokkanen VM, Sanaeva SI, Zhemkova MV. Relationship between severity of HIV infection and ocular pathology in patients with pulmonary tuberculosis. J.ophthalmol.(Ukraine).2018;5:56-59. https://doi.org/10.31288/oftalmolzh201855659
Background: Pulmonary tuberculosis most commonly develops and often becomes generalized among HIV-infected patients. HIV-positive individuals present extra-pulmonary forms of tuberculosis twice as often as HIV-negative individuals. Purpose: To determine the frequency of ocular pathology and the relationship between ocular pathology and CD4 cell count in HIV-positive patients with tuberculosis. Materials and Methods: Three thousand and eighty four patients with pulmonary tuberculosis including 320 (10.4%) patients co-infected with HIV underwent examination at the City Tuberculosis Dispensary between 2014 and 2016. Results: Allergic or toxic retinal vasculitides and peripheral focal chorioretinitis of tuberculous etiology in either active or inactive inflammatory phase were most common ocular disorders among HIV-positive patients with marked immune deficiency. In these patients, median CD4 cell count was ≤200-300 cells/mm3 compared to the norm of 1600 cells/mm3. Keywords: HIV, ocular tuberculosis, CD4 cells
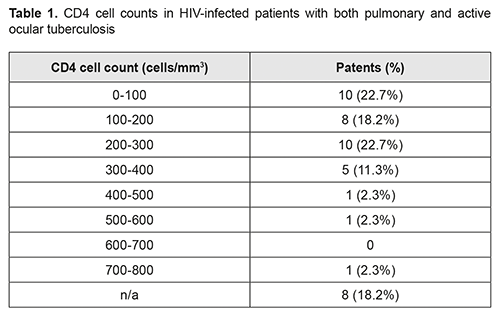
Introduction Tuberculosis is the most common opportunistic infection and often becomes generalized among HIV-infected patients. The WHO has reported that about one third of all HIV-infected patients develop tuberculosis that is an immediate cause of death in 30% of patients with HIV. HIV infection is believed to cause destabilization of immunity and contributes to conversion from inactive to active tuberculosis [1]. Active tuberculosis may up-regulate HIV replication, leading to accelerated progression of HIV to AIDS [2]. The annual risk of developing pulmonary tuberculosis in HIV-positive individuals is 5 to 10%, whereas the lifetime risk of developing tuberculosis in HIV-negative individuals is ≤10%. Tuberculosis may develop at any stage of HIV. Clinical course and manifestations of tuberculosis depend on the stage of HIV infection. The course of tuberculosis in patients with early HIV infection (stages 2B-4B as per the classification of Pokrovskii) is not substantially different from that in individuals without HIV. The picture of tuberculosis in patients with late HIV infection (stages 4B to 5 as per the classification of Pokrovskii) resembles that of primary tuberculosis tending to become highly generalized, with marked exudative inflammation and involvement of the lymphoid tissue. Extra-pulmonary forms of tuberculosis have been found to occur twice as often in patients with early HIV infection as in those with late HIV infection [3]. Extra-pulmonary tuberculosis in the presence of HIV infection manifests itself primarily as injuries to the lymphoid tissue, serous effusion and military tuberculosis [4], and less commonly as injuries to the central nervous system, gastrointestinal tract, bones and joints [5]. The association between CD4 T cell counts and incidence of extra-pulmonary tuberculosis in HIV-infected patients has been demonstrated. Extra-pulmonary tuberculosis was found in 13.5% of HIV-infected patients with a mildly reduced immune status against 71.8% of those with severely reduced numbers of CD4 T cells [6]. In addition, lymph node tuberculosis was most common, and was diagnosed in 69.2% of HIV-infected patients with generalized tuberculosis. Moreover, ocular tuberculosis was diagnosed in 3.5% of HIV-infected patients with generalized tuberculosis, with a median CD4 cell count of 246.4 cells/mm3 compared to the normal cell count of 600-1900 cells/mm3. Materials and Methods Three thousand and eighty four patients with pulmonary tuberculosis including 320 (10.4%) patients co-infected with HIV underwent examination at the St Petersburg City Tuberculosis Dispensary between 2014 and 2016. The mean age of the co-infected patients ranged from 30 to 40 years, and most (74%) of them were men. Patients underwent routine eye examination. In addition, they underwent ocular coherence tomography (Cirrus HD-OCT 5000; Carl Zeiss Meditec, Jena, Germany). Moreover, special techniques (tuberculin tests, test therapy, immunological and biochemical studies, etc.) were used for diagnosing ocular tuberculosis [7]. Of the 3084 patients with tuberculosis, 2364 (76.6%) were found to have an ocular pathology. Results Of the 320 HIV-co-infected patients, 179 (55.9%) were found to have an ocular pathology. It is noteworthy that none of these 179 individuals had ocular complaints. Ocular abnormalities, if any, were found during a mandatory eye screening (conducted in accordance with the Decree of the RF Ministry of Health No.109, of 21 March 2009). Active ocular tuberculosis was found in 44 (24.6%) of the HIV-co-infected patients with an ocular pathology. Blood was tested for CD4 cell counts at admission to the in-patient setting of the TB dispensary. In addition, HIV-1 viral load test was conducted to measure the number of HIV-1 RNA copies in a sample of blood. HIV-infected patients with both pulmonary and active ocular tuberculosis most commonly had ≤ 300 cells/mm3 CD4 cell counts, and 22.7% of them had ≤ 100 cells/mm3 CD4 cell counts (Table 1).
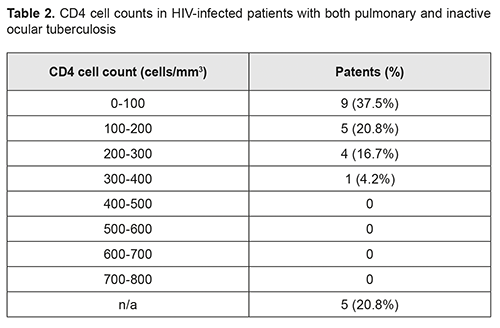
0-100 cells/mm3 was the most common CD4 cell count range among HIV-infected patients with both pulmonary and inactive ocular tuberculosis (Table 2).
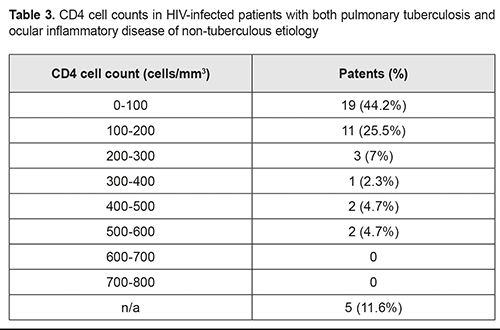
HIV-infected patients with both pulmonary tuberculosis and ocular inflammatory disease of non-tuberculous etiology most commonly had 0-100 cells/mm3 or 100-200 cells/mm3 CD4 cell counts (Table 3).
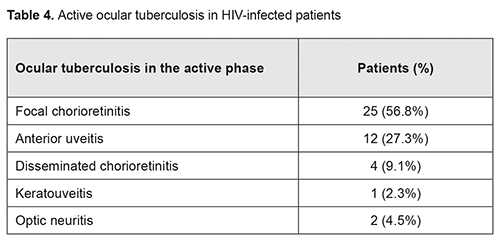
The vast majority of HIV-infected patients were not on antiretroviral therapy at the time of eye screening. Allergic or toxic retinal vasculitides take a special place among ocular disorders in patients co-infected with HIV and TB, and was found in 32 (17.9%) of 179 patients. Retinal vasculitis with infiltrated or disseminated pulmonary tuberculosis in the presence of reduced (≤100 cells/mm3) CD4 cell counts completely corresponded to the severity of the underlying disease. Focal chorioretinitis was found in 25 (56.8%) of the 44 patients with active ocular tuberculosis, with the extreme retinal periphery being the most common site. In addition, it most commonly did not cause reduced visual acuity. Anterior uveitis was the second most common (12 (27.3%) patients), while keratouveitis was the least common (1 (2.3%) patient) ocular pathology in patients with active ocular tuberculosis (Table 4).
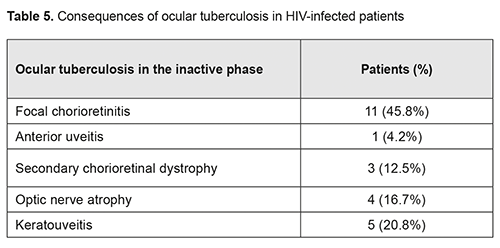
Inactive ocular tuberculosis was found in 24 (13.4%) patients. In these patients, focal chorioretinitis was the most common ocular pathology (11 (45.8%) patients), followed by anterior keratouveitis (5 (20.8%) patients) and optic nerve atrophy (4 (16.7%) patients) (Table 5).
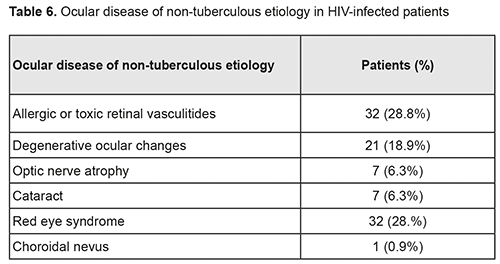
Of the HIV-co-infected patients with an ocular pathology, 111 (62%) had an ocular disease of non-tuberculous etiology, with allergic or toxic retinal vasculitides and red eye syndrome (dry eye, chronic blepharitis and chronic conjunctivitis) being most common (both 32/111 (28.8%) patients), followed by degenerative ocular changes (21/111 (18.9%) patients), optic nerve atrophy of traumatic or toxic etiology (71/111 (6.3%) patients) and complicated cataract (71/111 (6.3%) patients) (Table 6). Choroidal nevus was least common (1/111 (0.9%) patient).
Conclusion First, an ocular pathology of either tuberculous or non-tuberculous etiology was found to be more common in patients with a low (200-300 cells/m3 and lower) CD4 count compared with those with a high (>300 cells/m3) CD4 count. Second, peripheral focal chorioretinitis was the most common form of ocular tuberculosis in eyes of HIV-infected patients with tuberculosis. Third, tuberculous allergic retinal vasculitides reflected the severity of the underlying disease in patients co-infected with HIV and tuberculosis. Finally, active ocular tuberculosis was found in 24.6% of the TB/HIV-co-infected patients with an ocular pathology.
References
|