J.ophthalmol.(Ukraine).2018;6:19-22.
|
http://doi.org/10.31288/oftalmolzh201861922 Received: 11 September 2018; Published on-line: 30 December 2018 Choroidal thickness in patients with progressive and stabilized POAG M.V. Panchenko, Prof, Dr Sc (Med), I.G. Duras, Cand Sc (Med), O.M. Honchar, Cand Sc (Med), D.O. Prykhodko, MD, A.S. Pereiaslova, MD, L.G. Avilova, MD Kharkiv National Medical University; Kharkiv (Ukraine) E-mail: panchenko0802@gmail.com TO CITE THIS ARTICLE: Panchenko MV , Duras IG, Honchar OM, Prykhodko DO, Pereiaslova AS, Avilova LG.Choroidal thickness in patients with progressive and stabilized POAG. J.ophthalmol.(Ukraine).2018;6:19-22. http://doi.org/10.31288/oftalmolzh201861922
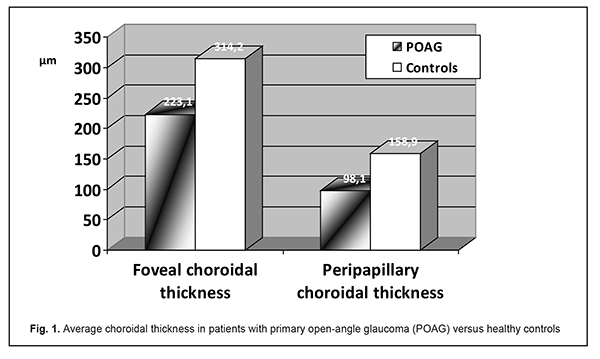
Purpose: To investigate choroidal thickness in patients with progressive and stabilized primary open-angle glaucoma (POAG). Materials and Methods: Forty-nine patients (87 eyes; age, 52 to 77 years) with stage 1, 2 or 3 POAG were involved in the study. Choroidal thickness was measured with optical coherence tomography. Results: The foveal choroidal thickness and peripapillary choroidal thickness were thinner in progressive POAG versus stabilized glaucoma (184.2±20.6 µm vs 261.1±19.4 µm, p<0.05; and 184.2±20.6 µm vs 261.1±19.4 µm, p>0.05, respectively). Foveal choroidal thickness was directly correlated with ganglion cell complex thickness (r=0.5725, p < 0.05), and negatively correlated with progressive POAG (r=-0.4246, p < 0.05). Conclusion: In patients with POAG, foveal choroidal thickness is directly correlated with ganglion cell complex thickness and disease progression. The foveal choroidal thickness and peripapillary choroidal thickness were 31% and 23%, respectively, thinner in progressive POAG versus stabilized POAG. Keywords: progressive and stabilized POAG, choroidal thickness Introduction The role of choroidal changes in the pathogenesis of primary open-angle glaucoma (POAG) has not been fully established, and the data available on choroidal thickness in POAG are controversial. A decreased caliber of choroidal vessels has been demonstrated histologically in glaucoma [1], which is likely to evidence choroidal thinning in the disease, but other studies [2] reported opposite findings. In addition, optical coherence tomography (OCT) studies varied in the findings regarding the assessment of choroidal thickness in glaucoma. Thus, OCT studies by Hirooka K. et al. (2012) [3] and Usui S. et al. (2012) [4] found that, compared with eyes of normal subjects, the choroidal thickness was thinner in eyes with normal-tension glaucoma (NTG) at the fovea, 3 mm from the fovea [4] and at the peripapillary region [3]. OCT studies by Kurysheva et al [5, 6] found that, the foveal choroidal thickness and peripapillary choroidal thickness were thinner in perimetric POAG versus normal eyes and preperimetric POAG versus normal eyes, with the differences for the perimetric POAG, but not for the preperimetric POAG being statistically significant. Opposite results were reported by Cennamo G. et al. [7], who found that, compared to healthy eyes, the choroidal thickness was increased in eyes with POAG. No significant differences have been observed in (a) subfoveal choroidal thickness between eyes with NTG and normal eyes [8], (b) peripapillary choroidal thickness between POAG and suspect eyes [9, 10], and (c) both average choroidal thickness and foveal choroidal thickness between eyes with advanced POAG and fellow eyes with no glaucoma or with mild glaucoma [11]. Mwanza et al [12] found no significant differences in foveal, temporal, or nasal choroidal thickness between normal, NTG, and POAG subjects. Another point is that, we believe that it is important to understand whether there are correlations of choroidal thickness with other structural and functional indices in patients with glaucoma. Kurysheva et al [5] have found direct correlation between choroidal thickness and retinal peripapillary nerve fiber layer thickness, and negative correlation between choroidal thickness and ganglion cell complex (GCC) global loss volume (GLV) both for perimetric and preperimetric POAG. In addition, there was a significant direct correlation between choroidal thickness and average GCC thickness for perimetric POAG [5]. Others [9, 10], however, have found no correlation between choroidal thickness and retinal peripapillary nerve fiber layer thickness. Although a study by Hirooka et al [3] has reported a correlation between peripapillary choroidal thickness and perimetric index MD that characterizes a mean deviation of retinal light sensitivity from the norm, others [5, 10, 11] have failed to find any correlation between choroidal thickness and visual field indices, and this matter requires further research. To the best of our knowledge, no Ukrainian studies have reported on changes in, and correlation of, choroidal thickness and structural and functional indices for POAG. The purpose of the study was to investigate choroidal thickness in patients with progressive and stabilized POAG. Materials and Methods Forty-nine patients (87 eyes; 28 women and 21 men; age, 52 to 77 years; mean age, 59.3 years) with stage 1, 2 or 3 POAG and 20 healthy controls (40 eyes; mean age, 55.9 years) were involved in the study. Exclusion criteria were macular changes, high myopia or high hyperopia, history of uveitis or eye surgery, abnormal ocular circulation, systemic vascular disease affecting choroidal thickness or anterior chamber angle less than 25 degrees. In addition, patients receiving systemic beta or calcium channel blockers were excluded from the study. Patients had a routine eye examination for glaucoma, including measurement of the antero-posterior axis. Choroidal thickness measurements were performed using a TOPCON 3D OCT-1000 apparatus (Topcon Corporation, Tokyo, Japan) at the same time of the day. The choroidal thickness was measured from the hyperreflective line corresponding to the RPE to the continuous hyperreflective line corresponding to the inner aspect of the sclera (or lamina fusca). If lamina fusca was not clearly visible on OCT image, the inner border of the suprachoroidal space was defined as the boundary between the hyporeflective choroid (the outer border of the vessels) and hyporeflective sclera. The distance was measured along the vertical axis from the RPE to the above structures [5]. Ganglion cell complex (GCC) thickness was determined using the vertical scan mode. The changes in static perimetry indices within a period of at least 6 months immediately before the current study were used to determine whether the POAG was progressive or not [9]. Progressive POAG and stabilized POAG were found in 36 eyes and 51 eyes, respectively. Statistical analyses were conducted using Statistica 6.1 (StatSoft, Tulsa, OK, USA) software. Results and Discussion Foveal choroidal thickness and peripapillary (at 3mm nasal from the fovea) choroidal thickness in patients with POAG (223.1±19.9 µm and 98.1±19.2 µm, respectively) were significantly (p < 0.05) thinner than in healthy individuals (314.2±17.2 µm and 158.9±16.5 µm, respectively).
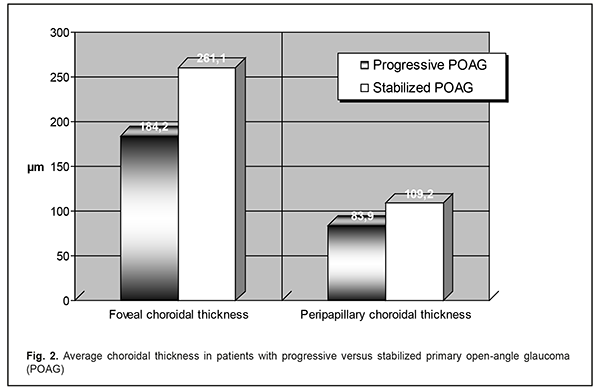
Average choroidal thickness in eyes with progressive versus stabilized glaucoma is shown in Fig. 2. The foveal choroidal thickness in eyes with progressive POAG was 31% thinner than in eyes with stabilized POAG, and the difference was statistically significant (184.2±20.6 µm vs 261.1±19.4 µm, respectively, p<0.05), whereas the peripapillary choroidal thickness in eyes with progressive POAG was 23% thinner than in eyes with stabilized POAG, but the difference was statistically not significant (184.2±20.6 µm vs 261.1±19.4 µm, respectively, p>0.05).
A moderate negative correlation was noted between foveal choroidal thickness and progressive POAG (r=-0.4246, p < 0.05). In addition, moderate direct correlations were found between average foveal choroidal thickness and GCC thickness (r=0.5725, p < 0.05) and inferior GCC thickness (r=0.5120, p < 0.05). Our findings of thinner foveal and peripapillary choroid in patients with POAG are in agreement with the findings of the study by Kurysheva et al [5, 6], but disagree with the findings of others who reported a thicker foveal and peripapillary choroid [7] or absence of statistically significant differences in foveal [11, 12] and peripapillary choroidal thickness in patients with POAG [12] compared with healthy individuals. In addition, our findings of direct correlations between average foveal choroidal thickness and GCC thickness (r=0.5725, p < 0.05) and inferior GCC thickness (r=0.5120, p < 0.05) are in line with the findings of (a) a negative correlation between choroidal thickness and GCC GLV for POAG and (b) a direct correlation between choroidal thickness and average GCC thickness [5]. Moreover, our findings of thinned foveal and peripapillaty choroidal in progressive POAG and a negative correlation between foveal choroidal thickness and progressive POAG might suggest a role of the choroid in the progression of glaucoma. Conclusion We found that, in patients with POAG, average foveal choroidal thickness was correlated both with progressive POAG and GCC thickness. Foveal choroidal thickness in eyes with progressive POAG was 31% thinner than in eyes with stabilized POAG (184.2±20.6 µm vs 261.1±19.4 µm, respectively, p<0.05), and peripapillary choroidal thickness in eyes with progressive POAG was 23% thinner than in eyes with stabilized POAG (184.2±20.6 µm vs 261.1±19.4 µm, respectively, p>0.05). These findings indicate that further research on the role of the choroid in POAG progression is warranted. References 1.Yin ZQ, Vaegan, Millar TJ, Beaumont P, Sarks S. Widespread choroidal insufficiency in primary open-angle glaucoma. J Glaucoma. 1997 Feb;6(1):23-32. 2.Spraul CW, Lang GE, Lang GK, Grossniklaus HE. Morphometric changes of the choriocapillaris and the choroidal vasculature in eyes with advanced glaucomatous changes. Vision Res. 2002 Mar;42(7):923-32. 3.Hirooka K, Fujiwara A, Shiragami C, et al. Relationship between progression of visual field damage and choroidal thickness in eyes with normal-tension glaucoma. Clin Exp Ophthalmol. 2012 Aug;40(6):576-82. 4.Usui S, Ikuno Y, Miki A, et al. Evaluation of the choroidal thickness using high-penetration optical coherence tomography with long wavelength in highly myopic normal-tension glaucoma. Am J Ophthalmol. 2012 Jan;153(1):10-6.e1. doi: 10.1016/j.ajo.2011.05.037. 5.Kurysheva NI, Ardzhevnishvili TD, Kiseleva TN, Fomin AV. [The choroid in glaucoma: the results of a study by optical coherence tomography]. Natsional’nyi zhurnal glaukoma. 2013;4:72-83. Russian. 6.Kurysheva NI, Boyarinceva MA, Fomin AV. [Choroidal thickness in primary angle-closure glaucoma: the results of Measurement by Means of Optical Coherence Tomography]. Ophthalmology in Russia. 2013; 10(4):26-31. Russian. https://doi.org/10.18008/1816-5095-2013-4-26-31 7.Cennamo G, Finelli M, Iaccarino G, de Crecchio G. Choroidal thickness in open-angle glaucoma measured by spectral-domain scanning laser ophthalmoscopy/optical coherence tomography. Ophthalmologica. 2012;228(1):47-52. doi: 10.1159/000336903. 8.Rhew JY, Kim YT, Choi KR.. Measurement of subfoveal choroidal thickness in normal-tension glaucoma in Korean patients. J Glaucoma. 2014 Jan;23(1):46-9. doi: 10.1097/IJG.0b013e31825af772. 9.Ehrlich JR, Peterson J, Parlitsis G, et al. Peripapillary choroidal thickness in glaucoma measured with optical coherence tomography. Exp Eye Res. 2011;92:189–94. 10.Maul EA, Friedman DS, Chang DS, et al. Choroidal thickness measured by spectral domain optical coherence tomography: factors affecting thickness in glaucoma patients. Ophthalmology. 2011 Aug;118(8):1571-9. doi: 10.1016/j.ophtha.2011.01.016. 11.Mwanza J-C, Sayyad FE, Budenz DL. Choroidal thickness in unilateral advanced glaucoma. Invest. Ophthalmol Vis Sci. 2012 Sep 28;53(10):6695-701. 12.Mwanza JC, Hochberg JT, Banitt MR, et al. Lack of association between glaucoma and macular choroidal thickness measured with enhanced depth-imaging optical coherence tomography. 2011 May 18;52(6):3430-5. doi: 10.1167/iovs.10-6600.
|