J.ophthalmol.(Ukraine).2019;4:38-42.
|
http://doi.org/10.31288/oftalmolzh201943842 The immune status of patients with frontal bone trauma with implant SYNTEKIST used in surgical treatment О.D.Bondarchuk1,2, V.V. Kishchuk1, О.F. Melnykov3, М.D. Tymchenko3, N.D. Didyk2 1 Mykola Pyrohov Vinnytsia National Medical University; Vinnytsia (Ukraine) 2 Mykola Pyrohov Vinnytsia Regional Hospital; Vinnytsia (Ukraine) 3 Prof. O.S. Kolomiychenko Otolaryngology Institute of NAMS; Kyiv (Ukraine) E-mail: eskulap20009@gmail.com TO CITE THIS ARTICLE: Bondarchuk ОD, Kishchuk VV, Melnykov ОF, Tymchenko МD, Didyk ND. The immune status of patients with frontal bone trauma with implant SYNTEKIST used in surgical treatment. J.ophthalmol.(Ukraine).2019;4:38-42. http://doi.org/10.31288/oftalmolzh201943842
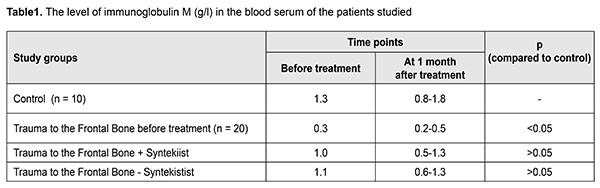
Aim. To determine the influence of a biocomposite on the state of the immune system of patients with trauma to the frontal bone at 1 month after surgical treatment. Materials and Methods. 20 patients with frontal bone fracture treated surgically with and without a SYNEKIST biocomposite were examined; 10 patients served as control. Immunoglobulins M, G, A, and E were determined in the blood serum using enzyme-linked immunosorbent assay. We also determined the content of prodefensin (lactoferrin, an indicator of the acute phase of inflammation), interleukins IL-1?, and interleukin-10. Results. On presentation and during the first days, the patients with trauma to the frontal bone had a decreased level of IgM which, however, reached the control level and was practically the same in both groups. There were no changes in other immunoglobulins in a month. The level of pro-inflammatory Il-a was increased on admission with a significant decrease within the first month in both treatment approaches. The on-admission level of pro-inflammatory cytokines did not differ significantly from the control while its level increased in the patients undergone the surgical treatment using a biocomposite material. The level of lactoferrin decreased to normal ranges in both treatment approaches. Conclusions. The advantage of the surgical treatment using a biocomposite material lies in the restoration of the IgM level and activation of anti-inflammatory mechanisms, Il-10, in particular, in 1 month. Keywords: trauma to the frontal bone, immunoglobulins, interleukins, biocomposite SYNTEKIST Introduction Every year brings dramatic statistic demonstrating increased rates of patients with severe multisystem and concomitant injuries, which is associated with growing technical facilities and intensive production, increasing transport speed, and a worsening of crime situation [1, 6, 7,]. A significant proportion in polytraumatism is presented by craniocerebral and maxillofacial injuries. Among maxillofacial traumas, the most common are lower jaw injuries followed by zygomatic fractures, comprising 72 to 92% and 3.1-24%, respectively. Traumatic injuries to the face can be work-related and non-work related. Non-work related traumas include household, transport, street, and sports ones and comprise up to 90%. The proportion of patients with trauma to the face ranges between 21 to 38% in the structure of dental inpatients. In peacetime, a rate of facial fractures ranges from 3.2 to 3.8% of all skeletal bone fractures. A high rate of such injuries, comprising 34% of all combined neurotraumas and reaching 59% in car accident-related injuries, is conditioned by anatomical proximity of the cerebral and visceral cranium [2]. Herewith, despite the constant improvement and implementation of new diagnostic methods and treatments, a proportion of early and late trauma-related complications requiring additional complex treatment and a degree of disability in working-age people after combined craniofacial traumas are persistently high [1, 5, 7]. The presence of posttraumatic defects in skull bones is one of the most common sequelae of traumatic brain injury [1-3]. Furthermore, combined frontal and orbital defects in the calvaria and base of the skull, according to various authors, comprise 1.2 to 30% of all defects of the skull [1, 4, 5]. A significant difference in the incidence of frontal and orbital defects, according to the literature, is associated with difficulties in performing reconstructive surgeries in this part of the skull and with the fact that this patient population is concentrated in large neurosurgical centers [1-3]. Anatomic and topographic features of the fronto-orbital region, which involves a great number of structures (frontal cortex, eyeballs, extraocular muscles, tear gland, neurovascular bundles, and others) located in a small space with complex spatial configuration, require using the up-to-date highly-informative neuroimaging techniques in diagnosis of bone defects the fronto-orbital region [6-9, 10-11]. A key factor which determines surgical tactics for a frontal bone fracture is damage to walls of the frontal cavity (FC) which is variable in size and shape. The front wall of the FC forms simultaneously the brow ridge and the glabella and the back wall of the FC is a part of the anterior cranial fossa. The bottom FC wall serves as medial portions in the roof of the orbit. In the posterior and inferior medial portions of the FC there is a frontonasal duct, which is hourglass-shaped with a diameter of 3-4 mm in the narrowest part, through which drainage into the middle nasal passage is conducted [13-14]. The main purposes of surgical treatment for frontal bone fractures which are extended to the walls of the frontal cavity are i) to protect intracranial structures and to seal the cavities of the skull; ii) to avoid early and late purulent and inflammatory complications; iii) to correct esthetically significant deformation and to reconstruct a shape of the frontal region. In recent years, synthetic compositions based on hydroxyapatite (SYNTEKIST) are used in the surgical treatment since they are able to accelerate osteogenesis and prevent the development of post-traumatic complications (V.V. Kishchuk, O.D. Bondarchuk, 2007, 2013). It is reasonable to study the effect of implantation of biocomposites in the surgical treatment of patients with trauma to the frontal bone and the role of immune mechanisms in the realization of a positive effect of a biocomposite material to create effective schemes of post-traumatic rehabilitation [2, 4, 5, 6]. This paper presents the results of the immunological examination in patients with trauma to the frontal bone at 1 month after trauma and implantation of a biocomposite material SYNTEKIST. Material and Methods Synthetic bioactive inorganic materials, called bioactive ceramic composites, SYNTEKIST, have been developed for bone plasty [15]. They are similar to natural bone mineral in composition and designed for solving different problems of surgical bone healing in traumatic injuries, tumors, and bone tissue diseases. These synthetic materials have undergone all technical and clinical trials and been included in The State Register of Medicinal Products of Ukraine (A bioactive ceramic composite SYNTEKIST for bone repair. Certificate of State Registration No3653/2005, issued to “Promtekhreserv, Ltd” according to Order of The State Register of Medicinal Products of Ukraine dated January 28, 2005). The speciality of materials of a SYNTEKIST biocomposite group is that they are bioactive multiphase inorganic composite materials which contain a superposition of virtually all phase and chemical components available in domestic and foreign materials of similar purpose which, in contrast, contain only one or two components each. In addition, they contain some new phase and chemical components and their combinations. This makes it possible to plan rather accurately the interaction of these materials with body tissues and to predict, for instance, the formation of pores in the material after implantation or a type of implant biodegradation, to adjust the strength, osteoconductive properties, and the rate of absorption of the material or its individual components, and to improve mechanic properties of implants and regulate the change in these properties [14]. Since the number of individual components can be changed within a wide range, certain variants of the SYNEKIST biocomposite, in fact, coincide with all known bioactive inorganic materials, the properties of a SYNEKIST biocomposite can be reasonably changed desirably towards the famous analogues. Some synergistic patterns, which are combinations of individual components enhancing the effect of the latter, have been found. In this regard, SYNEKIST biocomposites are the combination of bioactive inorganic materials well-proven in world practice, which contributes to identifying the best properties and compensating for the disadvantages of each component. The bioactivity of composites appears in osteointegration, a formation of direct biochemical bonds with adjacent bone tissue (with surrounding soft tissues for some biocomposite variants) through collagen molecules and fibers which attach to the SYNEKIST biocomposite and the bone structure so that the strength of this bond far exceeds that of the individual collagen fibers. In addition, due to osteoconductivity and osteostimulation properties, they serve as a conductor and a stimulator for the formation of new bone tissue on the surface and the pore spaces of the biocomposite and become a carcass of the newly formed bone. Twenty patients with trauma to the frontal bone in the acute period were examined on presentation at Mykola Pyrohov Vinnytsia Regional Hospital. The follow-up examinations were made at 1 month after surgical treatment using a biocomposite. A part of the patients was treated surgically without a SYNTEKIST biocomposite. Besides, 10 persons comparable in age served as control. Blood was collected from the elbow vein to prepare serum. Enzyme-immunoassay (reactive agents by Khema Medika, Russian Federation; readers by Lab Line, Austria) was used to test the blood in order to determine the levels of immunoglobulins M, G, A, E. Furthermore, we determined levels of prodefensin, lactoferrin which is an indicator of the acute phase of any inflammation (Belamy E.A., 1989), and anti-inflammatory cytokine interleukin-10 (reactive agents by Tsytokon and Vektor-Best, Russian Federation). The data were processed statistically by Statistica-6 using the nonparametric one-sided test (the Wilcoxon test) and the t-Student test as recommended by E.V. Gubler (1990). Results and Discussion On presentation and during the first days, the patients with trauma to the frontal bone had a decreased level of IgM which, however, reached the control level and was practically the same in both groups (Table 1).
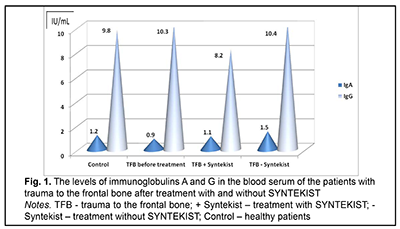
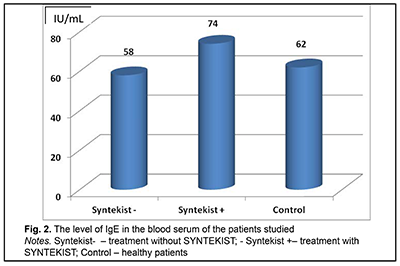
The IgA and IgG levels and the IgE level of in the blood serum at 1 month after surgery are demonstrated in Figure 1 and Figure 2, respectively, indicating that using a SYNEKIST biocomposite material did not influence the levels of immunoglobulins.
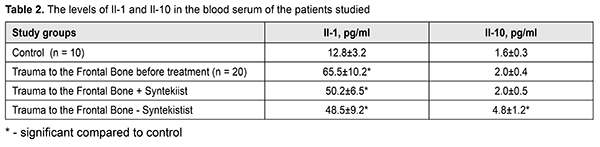
Table 2 demonstrates the results of studying pro- and anti-inflammatory cytokines in the blood of the patients with trauma to the frontal bone on presentation and at 1 month after treatment. Thus, the level of pro-inflammatory Il-a was increased on admission with a significant decrease within the first month in both treatment approaches. At the same time, the on-admission level of pro-inflammatory cytokines did not differ significantly from the control while its level increased in the patients undergone the surgical treatment using a biocomposite material, reaching 4.8 pg/ml versus 1.6 pg/ml in the control and 2.0 pg/ml in the patients with trauma to the frontal bone before treatment.
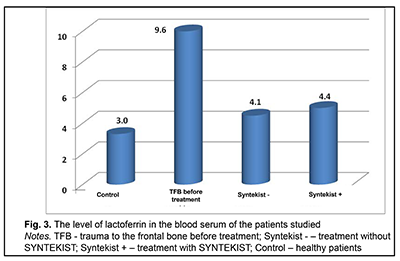
Figure 3 demonstrates the data on the level of lactoferrin in the blood of the study groups. Thus, both treatment approaches contributed to a decrease in the lactoferrin level to normal ranges as early as 1 month after treatment.
It can be concluded, based on the data analysis, that the advantage of the surgical treatment using a biocomposite material lies in the restoration of the IgM level and activation of anti-inflammatory mechanisms, Il-10, in particular, in 1 month.
References: 1.Gubler ЕV. [Informatics in pathology, clinical medicine and pediatrics]. L.: Medtsyna; 1990. 176 p. In Russian 2.Drannik GN. [Clinical immunology and allergology]. Kiev: Astra Print Ltd; 2006. 480 p. In Ukrainian. 3.Kishchuk VV, Bondarchuk OD. [Using biocomposites „Syntekist” to liquidate bone defects of ENT-organs]. Zhurnal vushnykh, nosovykh i horlovykh khvorob. 2007;5c:43-4. In Ukrainian. 4.Lysianyi NI, Pedachenko EG. [The peculiarities of autoimmune reactions’ development during recurring TBI]. Imunologiia ta alergologiia. 2006;3:53-6. In Russian. 5.J?ger C, Welzel T, Meyer-Zaika W, Epple M. A solid-state NMR investigation of the structure of nanocrystalline hydroxyapatite. Magn. Reson. Chem. 2006 Jun;44(6):573–80. 6.Jager L. Clinical immunology and allergology. М: Medicine. 1986;3:344-64. 7.Wu Y, Ackerman JL, Kim HM, Rey C, Barroug A, Glimcher MJ. Nuclear magnetic resonance spin-spin relaxation of the crystals of bone, dental enamel, and synthetic hydroxyapatites. J Bone Miner Res. 2002 Mar;17(3):472-80 p. 8.Avtandilov GG. [Basics of quantitative pathological anatomy]. M.: Meditsyna; 2006. 240 p. In Russian 9.Anikin IA, Bykova VP, Patjakina OK, Portenko EG. [Сondition of the lining in trepanation cavity after radical surgery on the middle ear according to histological research. Vestnik otorinolaringologii]. 1998;1:10–4. In Russian. 10.Dydenko VY, Kokorkyn DN, Husakova AA. [Autotransplantation of spongy autologous bone with marrow during reconstructive-plastic surgery of postoperative cavities in the temporal bone. Surgical technique of autograft collection and his preparation for autotransplantation]. Zhurnal vushnykh, nosovykh i horlovykh khvorob. 2007;6: 57–8. In Ukrainian. 11.Nikolaev NP, Mihajlenko NJu, Stroganova EE, Purjasev AS. Biocitalls as new materials for implantology in otorhinolaryngology. Rossijskaja otorinolaringologija. 2005;5:139–42. In Russian 12.Porushnyk YeP, Ivanchenko AA, Brusko AT. [Biocompatibility with bone tissue and osteotropy of composite materials based on biologic hydroxyapatite]. Problemy osteolohii. 2000; 3(4):89. In Ukrainian. 13.Kim HM, Himeno T, Kokubo T, Nakamura T. [Process and kinetics of bone like apatite formation on sintered hydroxyapatite in a simulated body fluid]. Biomaterials. 2005;26(2):4366–73. 14.Voloshina IA, Hamzalieva RB. [Mortality rate with othogenic and rhinogenic intracranial complications]. Vestnik otorinolaringologii. 2009;1:23–5. In Russian. 15.Semenov FV, Gorbonosoe IV, Starikov AV, Rianenko VA. [The use of glass-ceramic granules biosite-elkor to reduce the volume of trepanation cavity during operations on the middle ear]. Vestnik otorinolaringologii. 2005;1:32–5. In Russian. 16.Zabolotnyi DI, Kishchuk VV, Bondarchuk OD, Dmytrenko IV. Method of surgical treatment in patients with acute period of craniocerebral trauma of front-basal localization. Zhurnal vushnykh, nosovykh i horlovykh khvorob. 2013;6:80-3. In Ukrainian. The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|