J.ophthalmol.(Ukraine).2020;2:12-16.
|
http://doi.org/10.31288/oftalmolzh202021216 Received: 27 January 2020; Published on-line: 30 April 2020 Influence of persistently recurring pterygium on the optical interface of the cornea E.N. Bilalov1, Dr Sc (Med), Prof.; A.F. Yusupov2, Dr Sc (Med); A.E. Nozimov2; O.I. Oripov1, Assistant of Ophthalmology Department 1 Tashkent Medical Academy; Tashkent (Uzbekistan) 2 Eye Microsurgery, Specialized Republican Science and Practical Medical Center; Tashkent (Uzbekistan) E-mail: dr.ben58@mail.ru TO CITE THIS ARTICLE: Bilalov EN, Yusupov AF, Nozimov AE, Oripov OI. Influence of persistently recurring pterygium on the optical interface of the cornea. J.ophthalmol.(Ukraine).2020;2:12-16. http://doi.org/10.31288/oftalmolzh202021216
Background: Pterigiym is a proliferative, degenerative and inflammatory disease developing due to pathological hyperplasia, vascularization of the epithelium and migration of abnormal limbal stem cells to the central cornea, and accompanied by profound changes in the structure of underlying tissue. Purpose: To assess the influence of persistently recurring pterygium on the optical interface of the cornea using refractometry and corneal topography. Material and Methods: Sixty patients (67 eyes) with persistently recurring pterygium were included in this study. Patients were divided in four groups based on the number of recurrences. They underwent visual acuity assessment, refractometry and computerized corneal topography to assess the optical interface of the cornea. Results: We found significant differences in visual acuity, refractive errors and corneal topography indices among patients with persistently recurring pterygium with various numbers of recurrences. Our case follow-up demonstrated that permanent changes in the optical interface of the cornea developed with an increase in recurrences and persistence of growth of wing-shaped conjunctiva onto the cornea; these changes manifested as residual corneal astigmatism. Conclusion: An increase in pterygium recurrences results in permanent impairments of the optic interface of the cornea; this requires developing advanced surgical techniques capable of preventing recurrence of pterygium. Keywords: pterygium, recurrent pterygium, cornea, corneal topography
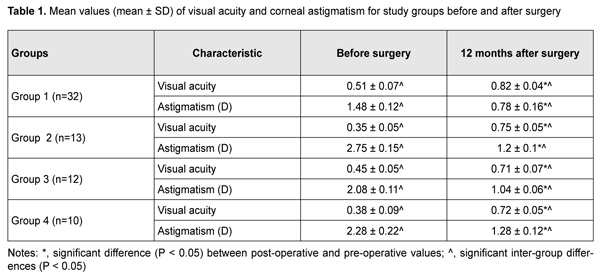
Introduction The term “persistently recurring pterygium” was coined by Iakimenko [1] and Legeza and collegues [2]. A pterygium is an ophthalmoheliosis characterized by a wing-shaped proliferation of the vascularized conjunctiva that encroaches onto the cornea [3-5]. It represents a proliferative, degenerative and inflammatory disease developing due to pathological hyperplasia and vascularization of the epithelium and migration of abnormal limbal stem cells to the central cornea, and accompanied by profound changes in the structure of underlying tissue, including destruction of the Bowman membrane [6-10]. Visual acuity drops sharply due to growth of wing-shaped conjunctiva onto the cornea, resulting in incapacity for work, professional impropriety, and, consequently, disability, in individuals of the working age [4, 11]. The corneal changes developing in the course of pterygium and after pterygiumectomy are rather difficult to analyze using conventional diagnostic techniques. Corneal topography is a promising modality, and enables an assessment of some objective and quantitative parameters of the cornea [12, 13]. The purpose of the study was to assess the influence of persistently recurring pterygium on the optical interface of the cornea using refractometry and corneal topography. Material and Methods Sixty patients (67 eyes) with persistently recurring pterygium who were treated at the Eye Disease Department of Multifield Clinic of Tashkent Medical Academy during 2013 to 2019 were included in this study. Of these, 46 (76.7%) and 14 (23.3%) lived in rural and urban areas, respectively. Patient age varied from 20 years to 65 years, and most of patients were from the age groups of 31-50 years (41.7%) and 51-65 years, that is, working-age and socially active groups of the population. Disease duration was < 2 years in two patients, 2 to 5 years in 18 (30%) and > 5 years in 36 (60%) patients. Each patient had had a history of pterygium surgery and at least one pterygium re-surgery, but patients varied in pterygiumectomy they had had received. Patients were divided in four groups based on the number of recurrences: Group 1 included 32 (47.7%) eyes with one recurrence, Group 2, 13 (19.4%) eyes with two recurrences, Group 3, 12 (17.9%) eyes with three recurrences, and Group 4, 10 (14.9%) eyes with four recurrences. Biomicroscopy studies found that there was a difference in clinical manifestations between eyes with persistently recurring pterygium and eyes with primary pterygium. In all cases, pterygium was seen along the limbus, corresponding to a sector of 1/2 to 1/3 of the circumference of the limbus. Inflammatory manifestations in the conjunctiva were more apparent and were revealed in 56 (83.5%) eyes. In these eyes, pterygium tissue was commonly scarred, dense, and immobile, and lost elasticity. Pterygium vessels were located atypically and were convoluted. The head of the pterygium was dense, had a chondroid consistency, and was fused with the cornea. Five (7.4%) eyes showed two to four pterygium heads, evidencing a severe course of the disease. In 51 (76.2%) eyes, infiltrates were present in the corneal tissue anterior to the head, and Fuchs islets were seen in the superficial layers. Twenty-four (35.8%) eyes demonstrated deformation of the semilunar fold due to cicatricial changes in the conjunctiva. The lacrimal caruncle was deformed, with a varying loss of outward mobility of the globe, in 9 (13.4%) eyes. Cicatricial strabismus was seen in 3 (4.5%) eyes. Six (8.9%) eyes exhibited short fornices, and 3 (4.4%) eyes, marked symblepharon. In addition, 14 (20.8%) eyes showed mild corneal scars due to history of pterygium surgery. All patients underwent combination pterygium excision with conjunctival autografting modified by us [14] for persistently recurring pterygium. Visual acuity assessment, refractometry with auto ref/ keratometer HRK-9000A (Huvitz, South Korea) and computerized corneal topography with computerized videokeratograph TMS-2N (Tomey Corporation 2-11-33; 451-0081, Japan) were used to assess the optical interface of the cornea. Studies were performed before and 3, 6 and 12 months after surgery. Corneal topograms were presented in three major formats (topographic, digital and 3D formats). Klyce corneal statistics software was used. Klyce corneal statistics involves Corneal Statistics Tables with Simulated Keratometry Readings (SimK), Surface Asymmetry Index (SAI), Surface Regularity Index (SRI) – Potential Visual Acuity (PVA), and Average Keratometry (Avek) indices [15]. Results Records of patients who exhibited no recurrence within 12 months after surgery were included in the analysis. Indices (including, in particular, visual acuity and corneal astigmatism) taken before surgery and 12 months after surgery were assessed. Table 1 presents values of uncorrected visual acuity (UCVA) and corneal astigmatism for patients of the four study groups. In patients of Group 1, mean UCVA significantly increased from 0.51 ± 0.07 at baseline to 0.82±0.04 at 12 months after re-surgery, and mean corneal astigmatism significantly decreased from 1.48 ± 0.12 D at baseline to 0.78 ± 0.16 D at 12 months after re-surgery. Compared to patients of Group 1, patients of Group 2 (with a history of two recurrences) had significantly decreased mean UCVA (0.35 ± 0.05) and significantly increased mean corneal astigmatism (2.75 ± 0.15 D) values before surgery. After surgery, mean UCVA and mean corneal astigmatism in patients of Group 2 improved to 0.75 ± 0.05 and 1.2 ± 0.1 D, respectively; these values, however, were subnormal. There were significant differences between postoperative and preoperative UCVA and corneal astigmatism for patients of Group 2 (Table 1). There was a similar tendency regarding mean UCVA and mean corneal astigmatism in patients of Groups 3 and 4. Thus, in patients of Group 3, mean UCVA increased from 0.45 ± 0.05 at baseline to 0.71±0.07 at 12 months after re-surgery, and mean corneal astigmatism decreased from 2.08 ± 0.11 D at baseline to 1.04 ± 0.06 D at 12 months after re-surgery. In patients of Group 4, mean UCVA increased from 0.38 ± 0.09 at baseline to 0.72±0.05 at 12 months after re-surgery, and mean corneal astigmatism decreased from 2.28 ± 0.22 D at baseline to 1.28 ± 0.06 D at 12 months after re-surgery.
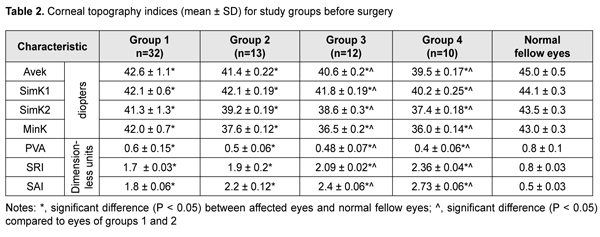
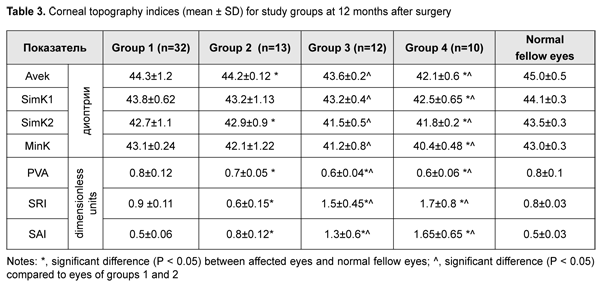
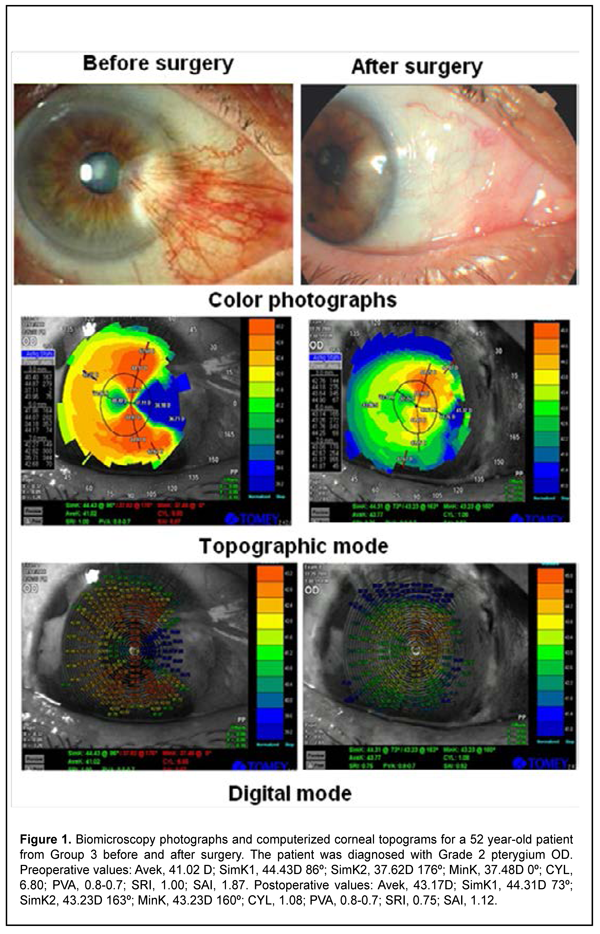
Tables 2 and 4 present corneal topography data before and after pterygium excision. Preoperatively, Avek, SimK1, SimK2 and MinK values were significantly lower than normal for all patients. In addition, mean Avek values for Groups 1 and 2 (42.6 ± 1.1 D and 41.4 ± 0.22 D, respectively) were significantly higher than for Groups 3 and 4 (40.6 ± 0.2 D and 39.5 ± 0.17 D, respectively). Moreover, major corneal topography indices, PVA, SRI and SAI, for all groups (more apparently, for Groups 3 and 4) were significantly lower than normal. Postoperatively, all patients exhibited improvements in all examined corneal topography indices. However, values of mean corneal topography indices were close to normal only for patients of Group 1. In other groups of the study, postoperatively, mean keratometry indices, Avek, SimK1, SimK2 and MinK, were significantly lower than normal, whereas mean corneal topography indices, PVA, SRI and SAI, were significantly higher than normal. In addition, the indices still tended to worsen with an increase in the number of recurrences and associated previous surgeries. In particular, mean postoperative SAI in patients of Group 4 was 1.65 ± 0.65, which was substantially higher than normal, evidencing severe defects in the optic zone. Figure 1 presents the case of a patient who had received surgery after three pterygium recurrences, and specifies preoperative and postoperative corneal topography indices for this patient.
Discussion A wing-shaped proliferation of the vascularized conjunctiva onto the cornea may result in corneal flattening, leading to changes in refractive error and visual acuity in the eye, which was confirmed by visual acuity and refractometry data. These findings are in agreement with those reported by Aliiev [1, 2], who also confirmed an increase in corneal aberrations with an increase in severity of pterygium. In the current study, there was a correlation between the severity of impairment in the optical interface of the cornea and the number of recurrences and associated previous surgeries. There was an increase in corneal astigmatism and decrease in visual acuity with an increase in pterygium recurrences. In addition, there was an increase in residual corneal astigmatism with an increase in recurrences, which was apparently demonstrated in patients of Group 4. Therefore, recurrence of wing-shaped growth of the conjunctiva onto the cornea and corneal flattening result in permanent deformation of the optical zone of the cornea, which leads to the development of permanent corneal astigmatism after surgery requiring additional correction. Our computerized corneal topography studies demonstrated that, postoperatively, in patients with several pterygium recurrences, there was statistically significant decrease in average keratometry index and significant increase in surface asymmetry index. The presence of above changes in these indices after surgery provided evidence that these changes had a permanent nature, and patients had persistent astigmatism that is very difficult to correct. In particular, efficacy of excimer laser processing of the corneal bed after pterygium surgery for correction of corneal aberrations has been assessed [1]. Therefore, we found significant differences in visual acuity, refractive errors and corneal topography indices among patients with persistently recurring pterygium with various numbers of recurrences. Our case follow-up demonstrated that permanent changes in the optical interface of the cornea developed with an increase in recurrences and persistence of growth of wing-shaped conjunctiva onto the cornea; these changes manifested as residual corneal astigmatism. Conclusion First, based on postoperative changes in visual acuity and refractive errors, in was demonstrated that permanent postoperative astigmatism developed in patients with persistently recurring pterygium. Second, based on postoperative changes in corneal topography indices, average keratometry and surface asymmetry indices, it was showed that severe deformations of the optical zone of the cornea developed due to repeated surgical interventions in persistently recurring pterygium. Finally, an increase in pterygium recurrences results in permanent impairments of the optic interface of the cornea; this requires developing advanced surgical techniques capable of preventing recurrence of pterygium.
References 1.Iakimenko SA. [Surgical treatment of persistently recurring pterygium] Zdravookhranenie Turkmenistana. 1983;11:41-4. Russian. 2.Legeza GV, Iakimenko SA, Manuh VF. [Surgical treatment of persistently recurring pterygium]. Oftalmol Zh. 1983; 4; 246-7. Russian. 3.Venger GE, Ulyanova NA, Gorianova IS. [Clinical and morphological features of various type of pterygium]. In: [Current aspects of clinical picture, diagnosis and treatment of eye disease. Proceedings of the Conference commemorating the 100th anniversary of the birth of N.A. Puchkovskaia]. Odesa; 2008. p. 27-8. Russian. 4.Petraevskii AV, Trishkin KS. [Pterygium: Etiopathogenesis, clinical picture and treatment]. Volgograd: Panorama; 2018. Russian. 5.Semenova EN, Gaisina GF, Suhov NA, Abdullin LL. [Outcomes of complex treatment for recurrent pterygium]. In: [Current problems of ophthalmology. Proceedings of the conference commemorating the 70th anniversary of the birth of Acad. M.T. Aznabaev]. Ufa; 2009; p. 543-5. Russian. 6.Trishkin KS. [Clinical and cytological types of pterygium]. In: [Current problems of experimental and clinical medicine. Proceedings of science and practical conference of young scientists and students]. Volgograd; 2012. p.120-1. Russian. 7.Usov VIa, Mal'cev EV, Kricun NIu. [ Clinical efficacy of surgical treatment of pterygium using high-frequency electrowelding of biological tissues for fixation of free limbal-conjunctival autograft]. Oftalmol Zh. 2015; 6; 6-12. Ukrainian. 8.Chan C, Liu YP, Tan D. Ocular surface changes in pterygium. Cornea. 2002; 21:38-42. 9.Kodavoor SK, Tiwari NN, Ramamurthy D. Long-term analysis of an unconventional way of doing double-head pterygium excision. Oman J Ophthalmol. 2019 Oct 11; 12(3):166-70. 10.Zhang LM, Lu Y, Gong L. Pterygium Is Related to Short Axial Length. Cornea. 2020; 39(2):140-5. 11.Drozhzhina GI, Troichenko LF, Ostashevskii VL, Kogan BM, Gaidamaka TB, Ivanovskaia EV. [Mistakes in the treatment of pterygium]. J of Ophthalmology (Ukraine). 2019;4;18-22. Russian. 12.Aliev A. [Features of corneal aberrations in pterygium]. Thesis for the degree of Cand Sc (Med). Moscow, 2008. Russian. 13.Aliev AGD, Ismailov MI. [Studying the effect of surgical treatment for pterygium on topography of the anterior corneal surface and refractive structure of the eye]. In: [Novel technologies of eye microsurgery]. Orenburg; 2000. p.142-2. Russian. 14.Nozimov AE. [Efficacy of combination surgery for persistently recurring pterygium]. Vestnik Bashkirskogo Gosudatstvennogo meditsinskogo instituta. 2016; 2;118-21. Russian. 15.Balashevich LI, Kachanov AB. [Clinical corneal topography and aberrometry]. Moscow: MNTK; 2008. Russian. The authors declare no conflict of interest.
|