J.ophthalmol.(Ukraine).2021;2:36-39.
|
http://doi.org/10.31288/oftalmolzh202123639 Received: 20 March 2021; Published on-line: 19 April 2021 Optimizing the management of dry eye in corneal and conjunctival cicatrization secondary to severe burns to the eye S. A. Iakymenko, Amjad Albin SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine; Odesa (Ukraine) E-mail: magi20069@gmail.com TO CITE THIS ARTICLE: Iakymenko SA, Amjad Albin. Optimizing the management of dry eye in corneal and conjunctival cicatrization secondary to severe burns to the eye. J.ophthalmol.(Ukraine).2021;2:36-39. http://doi.org/10.31288/oftalmolzh202123639 Background: Investigation of the pathogenesis of dry eye disease (DED) in corneal and conjunctival cicatrization secondary to severe burns to the eye as well as optimization of the management of this condition is an important and relevant task of clinical ophthalmology. Purpose: To optimize the management of DED in corneal and conjunctival cicatrization secondary to severe burns to the eye on the basis of tear production studies. Material and Methods: Forty patients (60 eyes) with DED and corneal and conjunctival cicatrization secondary to severe burns to the eye and showing various reductions in Schirmer test 1 scores were included in the study. Tear substitutes (Tear Naturale; Alcon, Fort Worth, TX) or Vidisic® gel (Mann Pharma, Berlin, Germany) were administered four times a day for eyes with mild or moderate dry eye, and six times a day for eyes with severe dry eye, and tear production was assessed at 2 weeks and at 3 months. Results: At two weeks, among the eyes treated with Vidisic gel, Schirmer test score improved from 12 mm to 13 mm (p > 0.05) for eyes with mild dry eye, from 6.5 mm to 8.4 mm for eyes with moderate dry eye, and from 3.1 mm to 6.3 mm for eyes with severe dry eye. In addition, among the eyes treated with teas substitutes, Schirmer test score improved from 11 mm to 13 mm for eyes with mild dry eye, from 6.1 mm to 8.1 mm for eyes with moderate dry eye, and from 2.6 mm to 4.4 mm for eyes with severe dry eye (p < 0.05). At three months, patients who were taking their medication as per schedule had approximately the same scores as at two weeks, whereas those who discontinued taking their medication or were taking it irregularly had approximately the same scores as at baseline. Conclusion: Our findings highlight the necessity of continuous tear substitute treatment for patients with DED and corneal and conjunctival cicatrization secondary to severe burns to the eye. Keywords: burns to the eye, dry eye disease, tear production
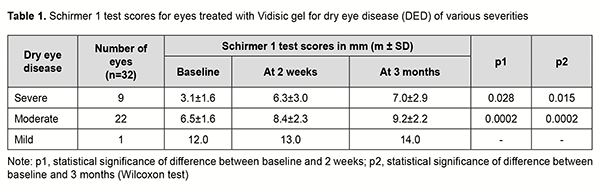
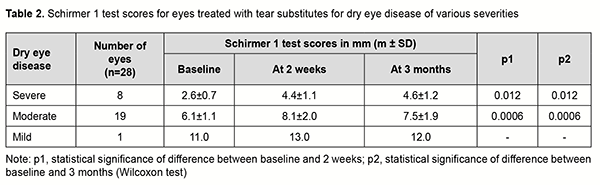
Introduction In recent years, there have been numerous studies on various aspects of dry eye disease (DED) [1-6]. However, no study has been conducted on the etiopathogenesis of DED associated with severe sequelae of burns to the eye. Therefore, investigation of the pathogenesis of DED in corneal and conjunctival cicatrization secondary to severe burns to the eye as well as optimization of the management of this condition is an important task of clinical ophthalmology. We conducted a study on the efficacy of tear substitutes and Vidisic® gel for patients with corneal and conjunctival cicatrization secondary to severe burns to the eye. The purpose of this work was to optimize the management of DED in corneal and conjunctival cicatrization secondary to severe burns to the eye on the basis of tear production studies. Material and Methods Forty patients (60 eyes) with DED and corneal and conjunctival cicatrization secondary to severe burns to the eye and showing various reductions in Schirmer test 1 scores were included in the study. Schirmer 1 test was used to assess tear production. At baseline, of the 60 eyes, 17 (28.3%) had severe dry eye (0 to 5 mm of wetting in 5 min), 41 (68.3%) moderate dry eye (6 to 10 mm of wetting in 5 min), and 2 (3.4%) mild dry eye (11 to 15 mm of wetting in 5 min). Tear substitutes (Tear Naturale; Alcon, Fort Worth, TX) or Vidisic® gel (Mann Pharma, Berlin, Germany) were administered four times a day for eyes with mild or moderate dry eye, and six times a day for eyes with severe dry eye, and tear production was assessed at 2 weeks and at 3 months. The control group involved 12 patients (15 eyes) with DED and corneal and conjunctival cicatrization secondary to severe burns to the eye who received topical normal saline. The study followed the ethical standards stated in the Declaration of Helsinki, the European Convention on Human Rights and Biomedicine and relevant laws of Ukraine. Statistical analyses were conducted using Statistica 8.0 (StatSoft, Tulsa, OK, USA) software. Quantitative data are presented as mean and standard deviation (SD). The Wilcoxon t-test was used for statistical analysis. The level of significance p ≤ 0.05 was assumed. Results The results of the study are presented in tables 1 and 2.
At two weeks, among the eyes treated with Vidisic gel, Schirmer test score improved from 12 mm to 13 mm (p > 0.05) for eyes with mild dry eye, from 6.5 mm to 8.4 mm for eyes with moderate dry eye, and from 3.1 mm to 6.3 mm for eyes with severe dry eye. In addition, among the eyes treated with teas substitutes, Schirmer test score improved from 11 mm to 13 mm for eyes with mild dry eye, from 6.1 mm to 8.1 mm for eyes with moderate dry eye, and from 2.6 mm to 4.4 mm for eyes with severe dry eye (p < 0.05). At three months, patients who were taking their medication as per schedule had approximately the same scores as at two weeks, whereas those who discontinued taking their medication or were taking it irregularly had approximately the same scores as at baseline. In the eyes of control group, the improved Schirmer test score was maintained for 30 to 60 minutes only after each treatment with normal saline. Therefore, both Vidisic and tear substitute improved Schirmer test scores. Particularly, among the eyes treated with Vidisic gel, the mean improvement in Schirmer test score was 3.1 mm (p = 0.034, Wilcoxon t-test) for eyes with severe dry eye and 2.1 mm (p = 0.038, Wilcoxon t-test) for eyes with moderate dry eye. In addition, among the eyes treated with tear substitute, the mean improvement in Schirmer test score was 2.2 mm (p = 0.059, Wilcoxon t-test) for eyes with severe dry eye and 1.6 mm (p = 0.086, Wilcoxon t-test) for eyes with moderate dry eye. However, among the eyes treated with normal saline, the mean improvement in Schirmer test score was 0.9 mm for eyes with severe dry eye and 0.8 mm for eyes with moderate dry eye. Moreover, the study showed improved subjective symptoms of DED in 28 (87.5%) of the 32 eyes treated with Vidisic, and 20 (71.4%) of the 28 eyes treated with tear substitute. These findings highlight the necessity of continuous tear substitute treatment for patients with DED and corneal and conjunctival cicatrization secondary to severe burns to the eye. Discussion We have demonstrated previously [7] a significantly decreased tear production (i.e., severe or very severe dry eye) in patients with DED and corneal and conjunctival cicatrization secondary to severe burns to the eye. We have also found [8] that the severity of DED in patients with DED and corneal and conjunctival cicatrization secondary to severe burns to the eye increased with an increase in either the area of symblepharon or the area of labial mucosal flap used after symblepharon excision. Our biochemical studies of tear fluid [9-11] demonstrated significant alteration in lipid peroxidation in the presence of reduced antioxidant activity (superoxide dismutase, catalase and glutathione peroxidase) in patients with DED secondary to burns to the eye. In addition, in patients with DED and corneal and conjunctival cicatrization secondary to severe burns to the eye, we found not only a reduction in tear production, but also qualitative changes in the major tear fluid components (total protein, lipids and mucin), impaired dehydrogenase and acid phosphatase activity, reduced thiol levels and increased disulfide levels, which indicated severe pathochemical changes in tear composition and quality. In general, our data indicated a significant impairment in the structure and function of tear proteins and integrity of cellular and subcellular membrane structures in corneal and conjunctival tissues in patients with DED secondary to burns to the eye. Moreover, a deficiency of mucin in the tear film may indicate a significantly impaired mucin production by goblet cells, whereas a deficiency of lipids in the tear film may indicate meibomian gland dysfunction in these patients. It has been histologically demonstrated [12] that reduced tear fluid production induced by goblet cell death and chronic conjunctival inflammation and fibrosis were the causes of DED in eyes with cicatrization secondary to severe burns to the eye. Our histomorphological studies have found that DED in conjunctival scarring in secondary to severe burns to the eye or to symblepharon repair with placement of the labial mucosa flap was caused by scarring of the mucus-producing conjunctival goblet cells and chronic conjunctival stromal inflammation and fibrosis, which necessitated systemic and topical treatments targeting the pathogenesis of the condition. Therefore, there is a body of clinical, biochemical and histomorphological evidence on the presence of conjunctival and corneal xerosis in the most severe forms of DED. On the basis of our studies, we suggested a comprehensive treatment for DED in eyes with cicatrization secondary to severe burns to the eye which included continuous treatment with tear substitutes and the agents capable of compensating for deficiencies in and stimulating the production of tear fluid and tear film components. Particularly, this treatment included the agents containing hyaluronidase and trehalose, a bioprotectant and osmoprotectant that normalizes corneal metabolism and improves corneal re-epithelization and ocular surface protection and regeneration. Our comprehensive treatment targeting the pathogenesis of DED in patients with corneal and conjunctival cicatrization secondary to severe burns to the eye and involving tear substitutes and anti-inflammatory, immune-enhancing, corneal protective and antioxidative agents was shown to substantially improve tear production in this severe eye disorder.
References 1.Brzheskii VV, Somov EE. [Dry eye syndrome]. St. Petersburg: Apollon; 1998. Russian. 2.Brzheskii VV, Somov EE. [Dry eye syndrome]. 2nd ed., revised and expanded. St. Petersburg: Levsha; 2003. Russian. 3.Brzheskii VV. [Tactics of medicamental treatment of patients with various clinical forms of dry eye syndrome]. Klinicheskaia oftalmologiia. 2008;9(1):4-6. Russian. 4.Drozhzhyna GI. [Inflammatory disorders of eyelids]. Odesa: Astroprint; 2011. Russian. 5.Drozhzhyna GI. [Current methods of treatment for dry eye disease]. Oftalmol Zh. 2013;5:3-9. Russian. 6.Zhaboiedov GD, Kireiev VV. [Dry eye syndrome: current state of the problem]. Oftalmol Zh. 2005;5:4-14. Ukrainian. 7.Iakimenko SA, Amjad Albin. [Tear production in patients with corneal and conjunctival cicatrization secondary to severe burns to the eye]. Oftalmol Zh. 2015;1:5-9. Russian. 8.Iakimenko SA, Amjad Albin. [Tear production in conjunctival and corneal xerosis and opportunities for its treatment]. Oftalmol Zh. 2015;2:16-21. Russian. 9.Iakimenko SA, Amjad Albin, Kolomiichuk SG. [Determination of the level of the protective components in the tear fluid in patients with scarring consequences of the eye burns]. Oftalmol Zh. 2014;3:19-24. Russian. 10.Iakimenko SA, Amzhad Albin, Parkhomenko TV. [Study of lipid peroxidation products in tear fluid of patients with corneal and conjunctival cicatrization secondary to burns to the eye]. Oftalmol Zh. 2014;4:14-9. Russian. 11.Iakimenko SA, Amjad Albin, Kolomiichuk SG. [Investigating the antioxidative potential of tear fluid in patients with cicatrization secondary to burns to the eye complicated by dry eye disease and opportunities for correcting this condition]. Oftalmologiia. Vostochnaia Evropa. 2014;3:19-24. Russian. 12.Iakimenko SA, Artiomov AV, Amjad Albin. [Morphological characteristics of the conjunctiva and labial mucosa in patients with cicatrization secondary to burns to the eye after reconstructive and plastic surgeries]. Oftalmologiia. Vostochnaia Evropa. 2015;1(24):30-7. Russian. Conflict of interest: No conflict of interest to declare
|