J.ophthalmol.(Ukraine).2021;2:55-60.
|
http://doi.org/10.31288/oftalmolzh202125560 Received: 09 November 2020; Published on-line: 19 April 2021 Reconstructive duet in a pole-to-pole surgery for ocular trauma: a pediatric case study N. F. Bobrova, M. M. Umanets, G. M. Dembovetska, A. Iu. Bratishko SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine"; Odesa (Ukraine) E-mail: filatov.detskoe7@gmail.com TO CITE THIS ARTICLE: Bobrova NF, Umanets MM, Dembovetskaia AN, Bratishko OYu. Reconstructive duet in a pole-to-pole surgery for ocular trauma: a pediatric case study. J.ophthalmol.(Ukraine).2021;2:55-60. http://doi.org/10.31288/oftalmolzh202125560 Background: As ocular trauma is a common type of pediatric trauma, can present with a variety of clinical manifestations, potentially leading to visual impairment and blindness, there is a need for novel methods of reconstructive surgery for severe sequelae of globe injury. Purpose: To analyze the course and outcome of pole-to-pole surgery performed by two teams of surgeons to relieve the sequelae of a severe penetrating globe injury in a child. Material and Methods: The data on the clinical state of the eye after a severe penetrating corneoscleral laceration with contusion component, examination results and pole-to-pole surgery outcomes were reported. Results: Because the state of the affected eye was very poor, the amount of reconstructive surgery was increased. Particularly, in the anterior segment, subluxated capsular bag was secured to the sclera, capsular ring was implanted and open and closed iridoplasties were performed, whereas, in the posterior segment, not only fibrous vitreous and the posterior hyaloid were removed as completely as possible, but also vitreous strands and adhesions that caused retinal tractions were trimmed, epiretinal membranes removed, and circular retinotomy and subsequent endolaser coagulation performed, thereby enabling unfolding the retina. Conclusion: First, in a severe post-traumatic injury to the pediatric eye, a pole-to-pole surgery can be performed with a good outcome. Second, the use of cutting edge technologies with advanced microsurgical tools and support in pediatric patients allows preserving a severely traumatized eye, arresting the inflammatory process, and avoiding subatrophy progression. Keywords: ocular trauma, penetrating injury, pole to pole surgery
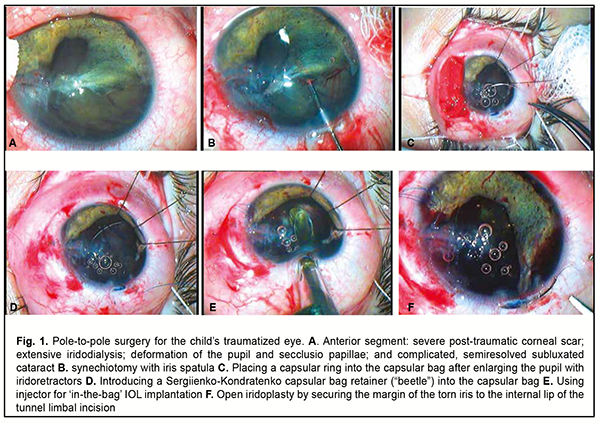
As ocular trauma is a common type of pediatric trauma, can present with a variety of clinical manifestations, potentially leading to visual impairment and blindness, there is a need for novel methods of reconstructive surgery for severe sequelae of globe injury. As early as 1978, Maryshev and Peets [1] classified a large cohort of children with eye injury into the three severity groups (mild, moderate and severe). The third group included cases of severe anterior globe injury with retinal detachment, reduced axial length, phthisis bulbi, and signs of sympathetic inflammation. Those authors suggested either conservative therapy to save the eye or enucleation as a treatment for the condition. The purpose of this paper is to discuss the course and outcome of surgery performed by two teams of surgeons to relieve the sequelae of a severe penetrating globe injury in a child. Material and Methods A nine-year girl received a penetrating injury to the right eye caused by a metal wire on August 6, 2020. A primary surgical repair of the corneoscleral laceration with surgical repositioning of the injured eye was performed at the local clinic. One and a half month after the traumatic event, the patient was diagnosed at the Department of Pediatric Eye Disorders, the Filatov institute, with adherent posttraumatic corneoscleral scar with sutures, semiresolved subluxated cataract, complete coloboma, iridodialysis, deformation and rupture of the pupil, retinal detachment (based on OCT), and initial subatrophy resulting from a severe penetrating corneoscleral laceration qith contusion component (Fig. 1A) in the righ eye.
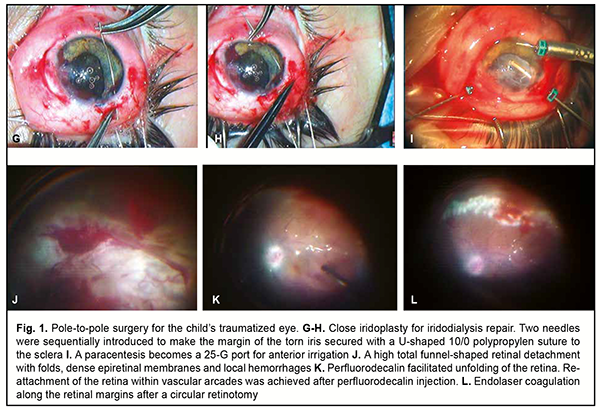
On examination, visual acuity was inaccurate projection of light OD and 1.2 OS (the left eye was healthy). Intraocular pressure (IOP) was 12.0 mmHg OD and 16 mmHg OS. Keratometry was 37.75 D OD and 43.5 D OS. Ultrasound biometry showed axial length of 19.91 mm OD and 23.35 mm OS. Intraocular lens (IOL) power calculation for Acrysof SN60WF: OD = 35.0 D; OS = 21.2D. The ultrasound scan findings OD included a shallow (1.1 mm) and irregular anterior chamber; iridodialysis extending from 9 o’clock to 12 o’clock position; an anterior chamber angle of about 40° for other directions; and a 3.9-mm thick and acoustically non-homogeneous crystalline lens displaced temporally. There was narrow funnel-shaped total retinal detachment, but no ciliary body detachment. Given the clinical state of the right eye, it was decided to conduct a combined anterior/posterior surgery in an effort to save the eye. Preoperatively, disinfectants were administered topically, dexamethason injections, parabulbarly, and dicynone and vikasol injections, intramuscularly, daily for 6 days. A combined anterior/posterior surgery was conducted on September 29, 2020. The primary purpose of the anterior segment reconstruction was to restore ocular media transparency and topographic and anatomic relationships of the traumatized tissues of the anterior segment by synechiotomy with iridoplasty, phacoaspiration of the opacified lens, and management of the subluxated lens capsule, capsular bag centration, and endocapsular IOL implantation. The patient was position on the operating bed, and given a 1.0 mL sub-Tenon injection of kenalog. Corneal and limbal sutures were removed. After mesaton 1% was introduced into the anterior chamber through the paracentesis at the 2 o'clock position, the pupil became only slightly larger. The conjunctiva was locally separated from the limbus, and a 1.75-mm limbal tunnel incision was made superiorly at the 12 o’clock position. Viscoat (a dispersive viscoelastic agent) was introduced into the anterior chamber. In order to perform synechiotomy, adhesions of the iris to the corneal scar were cut with scissors, and it was difficult to separate adhesions of the iris flap from the anterior capsule of the lens at the site of the pupil and at the site of iridodialysis with the help of the spatula (Fig. 1B). Additional paracenteses were made at the 6, 8 and 11 o'clock positions, and iris retractors were placed to provide a “stenting” of the iris to the limbus, and thus enable better visualization of the subluxated edge of an opacified lens, because lens zonules were absent in the area of lens coloboma. After the anterior capsule was stained with trypan blue, an anterior capsulorhexis not larger than 4-5 mm was performed with difficulty due to fibrosis of the anterior capsule. Angulated phacoemulsification tip was used to extract the lens in aspiration-irrigation mode. The lens was unevenly opaque and had viscous and partially resolved masses which were adhered to the posterior capsule. After removal of these masses, the remaining intact inferior zonules were very strained with a risk of zonular rupture, and, at the area of zonule deficiency, the whole capsular bag was ‘bent’ because of low aspiration levels. The posterior capsule was found to be translucent and exhibited sites of traumatic degeneration. Given that it was planned to perform retinal detachment surgery as the second stage of the operation, we decided to preserve the posterior capsule. A 10-mm diameter capsular ring (Fig. 1C) was implanted, and a Sergiienko-Kondratenko capsular bag retainer (“beetle”) (Fig. 1D) was secured to the sclera by a 10/0 polypropylene suture, resulting in expansion and centration of the bag. After filling the capsular bag with viscoelastic material, an Acrysof SN60WF25 lens was implanted at the 2 o’clock-8 o’clock position (Fig. 1E). Then, the iris retractors were removed, the edge of the iris flap was sutured to the internal lip of the tunnel limbal incision at the 12 o’clock position by a 10/0 nylon suture, resulting in expansion and straightening of the profile of a narrow, atrophic and torn iris flap (Fig. 1F). In addition, the middle portion of the flap at the area of iridodialysis was secured with a U-shaped 10/0 polypropylen suture to the sclera (Fig. 1G, H), resulting in repair of iridodialysis. It was impossible to cover the wound site underlying the corneal scar with the iris tissue due to complete loss of this tissue (it is likely that this tissue had been cut off during primary surgical repair performed at the local clinic), and thus total iris coloboma extending from 12 o’clock to 3 o’clock was not repaired. Vitrectomy for repair of a total funnel-shaped retinal detachment was the next stage of surgery. Pars plana vitrectomy was performed using the Alcon Constellation 25-G vitrectomy machine (Alcon Laboratories, Inc., Fort Worth, TX, USA) and OMS-800 OFFISS microscope (Topcon, Tokyo, Japan) featuring the Optical Fiber Free Intravitreal Surgery System (OFFISS). The purpose of vitrectomy was to remove the changed vitreous, vitreous adhesions and strands, and epiretinal membranes, and to perform silicone oil tamponade of the vitreous cavity to repair a total funnel-shaped retinal detachment. Irrigation was performed from the anterior chamber (by introducing a cannula through the 8-o’clock paracentesis made by the anterior eye surgeon (Fig. 1I)), given the height of retinal detachment, the impossibility to visualize the trocar and confirm its presence in the vitreal cavity, and the potential risk of instrument getting into the subretinal space leading to the danger of choroidal detachment and hypotony. Anterior infusion allowed for (1) adequate control of IOP, which decreased the risk of corneal opacification and retinal incarceration during instrument removal, and (2) maintaining a deep anterior chamber. Another advantage of the above way of installing an infusion cannula was maintaining the integrity of the scleral site, given implantation of a Sergiienko-Kondratenko capsular bag retainer (“beetle”) at the proper region. Standard pars plana ports for vitreous removal using the vitrectomy cutter and illumination of the posterior segment were created at the 2 o’clock and 10 o’clock positions. The vitreous contaminated with blood was removed at vacuum rate not exceeding 100 mmHg and cut rate of 5000 cpm. Therefore, the risk of iatrogenic retinal breaks was minimized due to low suction and high cut rates. Once the vitreous cavity became transparent again, a total T-shaped or closed funnel-shaped total retinal detachment became visible (Fig. 1J). A dense epiretinal membrane was grasped with forceps and peeled from the retinal surface to unfold the retina, allowing visualization of a closed funnel of the detached retina. Subsequently, perfluorodecalin, a liquid of a low viscosity and high specific gravity, was injected into the vitreous cavity to unfold the central retina and make the optic disk and macula easily visible (Fig. 1K). Unfortunately, due to apparent intraretinal fibrosis and retinal loss, the retina did not become completely unfolded even after the epiretinal membranes were removed as much as possible. Therefore, a 360 degree relaxing retinotomy was performed. Complete retinal re-attachment was achieved after repeat injection of perfluorodecalin. Once the contact between the retina and choroid was achieved, endolaser coagulation consisting of a triple or quadruple row of confluent laser burns was done along the retinotomy margins (Fig. 1L). Fluid-gas exchange was then done, and silicone oil (B&L Oxane 5700) tamponade of the vitreous cavity was performed. A dispersive viscoelastic agent was injected into the anterior chamber to protect the corneal endothelium and prevent silicone oil migration and as a measure of prophylaxis against subatrophy. Each sclerotomy was closed with a single biodegradable stitch using a 7-0 polyglactin suture. During vitrectomy, infusion flow was sufficient for maintenance of adequate intraocular pressure. In addition, no intraoperative or postoperative complications were observed. Total anesthesia duration was 100 minutes, which corresponded well to total surgery duration, given the severe extent of ocular injury and each of the two teams of surgeons working in its dedicated operating room. Results Mild ocular hypertension and a large silicone oil droplet entering the anterior chamber through the unrepaired iris coloboma in the superior inner quadrant were noted within a few postoperative days. After ocular hypotensive drug treatment, the IOP of the affected eye normalized, and the oil droplet moved to the posterior segment and did not appear in the anterior chamber any more. Anti-inflammatory and hemostatic medications were administered. The clinical state of the right eye improved after surgery. At discharge, the eye was almost calm (Fig. 2). The cornea was transparent, and the site of the original injury was represented by an almost horizontal posttraumatic scar, extending from the center to the posterior peripheral cornea and sclera. The anterior chamber was of moderate depth, the aqueous humor was transparent, and no silicone oil drops were seen. A 4-mm diameter pupil with extensive superior posttraumatic iris coloboma was seen. A pseudofacic eye had an in-the-bag implanted Acrysof SN60WF IOL, which had slight temporal decentration. The fundus reflex was evenly pink. Fundus examination of the right eye showed a pale pink optic disc with clear margins and individual macular hemorrhages. The relative caliber of the retinal arteries and veins (the A/V ratio) was 2:3. Laser coagulation spots were seen along the margins of an extensive 360-degree midperipheral retinotomy. Mild preretinal hemorrhages were seen along the retinotomy margins and the retina appeared re-attached.
The patient’s IOP OD increased to 16.0 mmHg, and, taking in account the presence of silicone oil in the vitreous cavity, axial length OD increased to 22.13 mm. The patient regained pattern vision OD. We hope for positive late treatment outcome.
Discussion Major anterior segment reconstruction in children with severe posttraumatic ocular disorders involves an early choice between a single-stage or multiple-stage strategy, but today, there is no general agreement among ophthalmologists on this choice. Vasil’eva [2] and Gerban [3], experienced pediatric eye surgeons, believed, that multiple-stage strategy would be more effective even in anterior segment reconstruction in children with combined injury to the cornea, iris and lens, because of concerns of apparent inflammatory response of traumatized tissue and the increased tendency of the pediatric eye to develop exudates and scars. The use of advanced surgical technologies made it possible to refute that opinion. Numerous works by Bobrova [4-8] have proved that, in children with severe posttraumatic ocular disorders, a more effective option is a comprehensive optic reconstruction procedure aiming to restore ocular media transparency and topographic and normal anatomic relationships of the traumatized tissues of the anterior segment by a single-stage surgery for all these traumatized structures. It is, however, still being discussed whether it is possible and reasonable to perform a one-stage combined anterior and posterior segment surgery in pediatric injury to the whole globe, especially if retinal detachment develops in the traumatized eye. It is necessary to recognize that such cases are uncommon. The leading foreign ocular trauma surgeons like Zakharov [9], Forlini [10-12], Kuhn [13] and others believe that a single-stage strategy is required to arrest the development of subatrophy in the traumatized eye. It is still being debated at which time point after a traumatic event and primary surgical repair a single-stage procedure should be performed, and whether two teams of eye surgeons (an anterior segment team and a posterior segment team) or only one surgeon should be involved in performing this procedure. Forlini [12] was a pioneer of “pole to pole surgery” for posttraumatic reconstruction of the eye. He believed that posterior segment surgery was more important than anterior segment surgery in posttraumatic reconstruction of the eye, because the late treatment outcome, including optic outcome will depend on the state of the traumatized retina. In our opinion, reconstruction of the anterior eye is not less important than that of the posterior eye, because it enables the work of posterior segment surgeons and is essential for subsequent normal course of the reparative process in the affected eye. In addition, the iris-lens diaphragm divides the eye into the anterior and posterior segments, and reconstruction of the diaphragm is of special importance in a single-stage reconstructive procedure for the two segments. Both the iris restored by open and closed iridoplasty and the implanted IOL act as a border between the two segments in the traumatized eye [8]. The ideal place for an IOL is typically in the capsular bag, especially in pediatric cases, and even in cases in which there are capsular bag defects, if the surgeon succeeds in restoring the position of the bag, straightening it with the help of viscoelastic, and performing in-the-bag implantation of various rings and retainers. The restored iris-capsule diaphragm allows the vitreous surgeon to apply various techniques for unfolding the retina, with the use of heavy liquids (like perfluorodecalin) and tamponade agents like silicone oil which does not migrate into the anterior segment subsequently. It has been reported [13-20] that, while performing vitrectomy after anterior segment reconstruction it is beneficial to use a translimbal approach to infusion cannula installation. This approach provides for a controllable IOP, prevents infusion into the subretinal or subchoroidal spaces, and allows minimizing trauma to the sclera, which, taken together, facilitates safe, effective and complete vitrectomy. The cutting edge high-technology comprehensive surgical procedures have been not completely adopted in the clinical practice of adult ocular trauma, when it comes to a completely mature organ. These procedures in the management of pediatric ocular trauma are even more controversial, given the specificity of responses of immature child eye and body. Some attempts, however, have been made to perform these procedures in children. Thus, Bobrova [8] reported a case of a nine-year-old child who sustained a severe penetrating globe injury from a knife, with the development corneal scar, traumatic cataract, deformation of the pupil, total funnel-shaped retinal detachment and initial subatrophy. The child received two surgical procedures. The first procedure included synechiotomy, phacoaspiration of the traumatic cataract, and intracapsular IOL implantation, and the second procedure was performed two weeks thereafter, and included a total vitrectomy with removal of the posterior hyaloid and epiretinal membrane, 180 degree retinotomy, and silicone oil tamponade of the vitreous cavity. Although exudative response developed postoperatively, this treatment has managed to halt the progression of subatrophy, and the globe was preserved [5]. Compared with the above case, the clinical state of the traumatized eye at presentation in the case reported in this paper was even worse, and the amount of reconstructive surgery was increased. Particularly, in the anterior segment, subluxated capsular bag was secured to the sclera, and open and closed iridoplasties were performed, whereas, in the posterior segment, not only fibrous vitreous and the posterior hyaloid were removed as completely as possible, but also vitreous strands and adhesions that caused retinal tractions were trimmed, epiretinal membranes removed, and circular retinotomy and subsequent endolaser coagulation performed, thereby enabling unfolding the retina. Silicone oil of the highest viscosity (5700 cst) was used to perform a permanent tamponade, given apparent ocular hypotony at presentation and an axial length which was 3 mm shorter than normal. The injection of a dispersive viscoelastic into the anterior chamber allowed preventing silicone oil migration to the anterior chamber, increasing IOP and removing subatrophy. In our opinion, in the case reported here, marked exudative response of pediatric ocular coats was avoided due to such features as (a) an injection of long acting sub-Tenon’s corticosteroid performed on the operating table prior to anterior segment surgery, and (b) a pole-to-pole approach to surgery. Clinical practice demonstrated that pole-to-pole surgery was better tolerated by a pediatric eye compared to multi-stage surgery (even with a short stage-to-stage time), and a response to pole-to-pole surgery in general was less intensive than to multi-stage surgery. Therefore, in a severe post-traumatic penetrating injury to the pediatric eye, a pole-to-pole surgery can be performed with a good outcome. The use of cutting edge technologies with advanced microsurgical tools and support in pediatric patients allows preserving a severely traumatized eye, arresting the inflammatory process, and avoiding subatrophy progression. References 1.Maryshev YuA, Peets SA. [Microsurgical interventions in comprehensive therapy for consequences of pediatric penetrating globe injuries]. In: [Ocular trauma]. Moscow; 1978. Russian. p.198-200. 2.Vasil’eva SF. [Traumatic eye lesions in childhood and the principles of their surgical treatment]. Oftalmol Zh. 1980;35(3):137-41. Russian. 3.Gorban’ AM. [Features of pediatric eye surgery]. In: [Proceedings of the 7th Congress of Ophthalmologists of the Ukrainian SSR]. Odessa; 1984. p.160-1. Russian. 4.Bobrova NF. [Viscoelastics in reconstructive microsurgery of the anterior segment in pediatric eyes]. In: [Proceedings of the Conference on Current Issues in Pediatric Ophthalmology]. Moscow; 1997. p.107-8. Russian. 5.Bobrova NF. [Classification and tactics of surgical treatment for anterior segment trauma in children]. Oftalmol Zh. 1992;2:91-5. Russian. 6.Bobrova NF. [Primary reconstruction for severe ocular trauma in children and its efficacy]. In: [Proceedings of the 10th International Ophthalmological Odessa-Genoa Symposium]. Odessa; 1991. p.107-8. Russian. 7.Bobrova NF. [Ocular trauma in children: a monograph]. Moscow: Meditsina; 2003. Russian. 8.Bobrova NF. [Reconstructive surgery for pediatric ocular injuries]. Odessa: Feniks; 2013. Russian. 9.Zakharov VD. [Vitreoretinal Surgery: a monograph]. Moscow: Meditsina; 2003. Russian. 10.Forlini C, Lavorato P, Ambesi-Impiombato M, et al.Traumatic cataract: which IOL implantation? In: Proceedings of the 5th Congress of the Black Sea Ophthalmological Society. Odessa, Ukraine. 24-26 May 2007. 11.Forlini C, Bratu A, Forlini M, et al. Mini-Invasive surgery: No limits. Gold standard in complex traumas. In: Proceedings of the 8th Symposium of International Society of Ocular Trauma. 19-22 June 2008. Wurtsburg, 2008. p.13. 12.Forlini C, Forlini M, Bratu A, Rossini P. Pole to pole surgery in severe post-traumatic PVR. The role of temporaly keratoprosthesis and open sky surgery. In: Proceedings of the 11th EVRS Meeting. 1-4 October, 2011. Valeta, Malta. p. 155. 13.Kuhn F. Ocular traumatology. Berlin, Heidelberg: Springer-Verlag; 2008. 14.John JS, Zloty P, Franklin AJ. Combined Anterior and Posterior Segment Surgery is Safe and Effective for a Broad Range of Pathologies in a Private Practice Setting. ARVO Annual Meeting Abstract. September 2016;57(12). Seattle, Wash. May 1-5, 2016. 15.Xu K, Chin EK, Almeida DR. Five-Port Combined Limbal and Pars Plana Vitrectomy for Infectious Endophthalmitis. Case Rep Ophthalmol. 2016 Dec 13;7(3):289-1. 16.Gan NY, Lam WC. Special considerations for pediatric vitreoretinal surgery. Taiwan J Ophthalmol. Oct-Dec 2018;8(4):237-42. 17.Lin P. Pars Plana Anterior Vitrectomy. Peer review. Cataract & Refractive Surgery Today. 2005;6. 18.Narang P, Agarwal A. Clinical outcomes of pars plicata anterior vitrectomy: 2-year results. Indian J Ophthalmol. 2015 Sep;63(9):699-703. 19.Schmidt JC, Meyer CH, Mennel S. [Pars-plana vitrectomy with anterior chamber infusion via a paracentesis in pseudophakic eyes]. Ophthalmologe. 2007 Mar;104(3):222-5. German. 20.Mahajan VB. Limbus-based vitrectomy offers safe alternative in pediatric cases. Retina Today. 2012 April;7:67–8.
The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
|