J.ophthalmol.(Ukraine).2021;5:47-55.
|
http://doi.org/10.31288/oftalmolzh202154755 Received: 15 July 2021; Published on-line: 23 October 2021 Effect of optical-reflection method of accommodative facility training on meridional acuity in astigmats with amblyopia V. A. Kolomiyets, O. V. Kachan SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine"; Odesa (Ukraine) E-mail: kolomiets.wa@gmail.com TO CITE THIS ARTICLE: Kolomiyets VA, Kachan OV. Effect of optical-reflection method of accommodative facility training on meridional acuity in astigmats with amblyopia. J.ophthalmol.(Ukraine).2021;5:47-55. http://doi.org/10.31288/oftalmolzh202154755
Background: The efficacy of accommodative facility training as a method of treatment for meridional amblyopia (MA) in astigmatic children with amblyopia was studied. MA manifests itself as selective alterations in visual acuity (VA), with substantial differences in the ability to resolve contours of different orientations, and may cause impairments in mechanisms of integrated processing of visual stimulus, development of cognitive abilities in children and visual performance. Purpose: To assess the effect of optical-reflection method of accommodative facility training on vernier acuity in meridians (MVA) in the treatment of astigmatic children with amblyopia. Material and Methods: Twenty seven children aged 5 to 12 years, with both refractive amblyopia and with-the-rule hyperopic astigmatism were included in the study, and underwent an examination. The spherical component of refraction ranged from +0.5D to +5.5D, and the cylindical component, from 0.5D to 4.5D. Best-corrected visual acuity (Sivtsev Chart) was assessed. Accommodative facility training was performed monocularly by image defocusing with lenses of a variable power. A +0.5-D sphere was placed just in front of the best correction for the study eye in order to blur this line. The +0.5-D sphere was replaced by a -0.5-D sphere after the optotypes became clearly visible. Thereafter, the training cycle was repeated using a ±0.75-D sphere and, subsequently, a ±1.0-D sphere. Lens power was gradually increased until it could be compensated by accommodation. The treatment course consisted of one training session a day for 10 days. Special computer software was used to determine corrected MVA. Linear objects were presented on the computer screen, and the smallest lateral displacement of one line from another that can be detected by the examinee will characterize the level of MVA. Results: A new algorithm was proposed for assessing the efficacy of treatment of MA in astigmats, with refractive asymmetries and meridional asymmetries in vernier acuity considered as vector quantities. It was demonstrated that a group of amblyops with the same type of astigmatism was not homogeneous. It was found possible to split such a group of patients into three clusters that differ in the type of variation in meridional acuity in the orthogonal meridians compared to refractive asymmetries. One cluster had equal vernier acuities in the vertical and horizontal meridians, the second had vernier acuity in the horizontal meridian better than in the vertical meridian, and the third had vernier acuity in the horizontal meridian worse than in the vertical meridian. MVA was greater in magnitude in one of the orthogonal meridians than in another in the dominant eyes in 37% of study patients, and in the fellow eyes in 50% of study patients. MVA values in the orthogonal meridians were similar in 56.6% of study patients. There was a 15.1-percent increase, from 56.6% to 71.1% in the number of eyes with a similar vernier acuity in the orthogonal meridians after treatment. A positive effect was achieved through elimination of meridional asymmetry in vernier acuity in a portion of patients from clusters that differ in the direction of meridional asymmetry in vernier acuity. In addition, the number of eyes in the category of patients with a visual acuity of 0.75-0.8 (as assessed with complex optotypes) increased by 11.35%. Conclusion: The efficacy of treatment for MA should be assessed in homogeneous clusters with similar direction of meridional asymmetry in visual acuity. Preliminary data on the efficacy of treatment of amblyopia by accommodative facility training allows considering this training as a method of treatment for meridional amblyopia. The method of determination of meridional acuity should be included in the standard examination of patients with amblyopia. Keywords: astigmatism, meridional amblyopia, meridional variations in visual acuity, amblyopia treatment
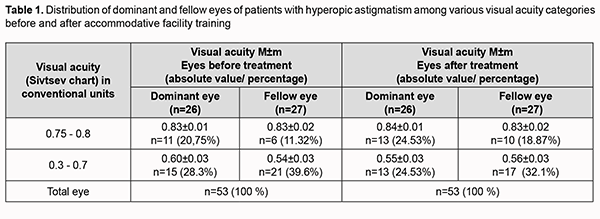
Introduction Refractive abnormalities are a major cause of impaired monocular and binocular function among children and adults. Patients with astigmatism are characterized by the most complex impairments in the mechanisms underlying binocular vision and visual perception. This is due to the fact that, in astigmatism, there is a difference in the degree of refraction in different meridia, and an eye has two focal points, with one or both of them failing to coincide with the retina. As a result, visual acuity (VA) in one meridian will be lower than in another. Astigmatism-associated refractive asymmetries may cause the development of a special form of amblyopia, the so-called meridional amblyopia (MA) [1-5]. MA manifests itself as selective alterations in visual acuity (VA), with substantial differences in the ability to resolve contours of different orientations [3]. It has been experimentally demonstrated that prolonged absence of normal monocular and binocular stimulation resulted in loss of cortical binocular neurons which are normally activated by binocular signals. These neurons are similar in the structure of connections with symmetrical sites the right and left retinae and provide the functional basis for the mechanisms of binocular and stereoscopic vision [3, 6]. Treatment of MA is important, because the disease can cause serious abnormalities in monocular and binocular mechanisms of integrated processing of visual stimulus, development of cognitive abilities in children and visual performance [7]. Study rationale The challenge of addressing amblyopia and binocular vision disorders persists although a lot of new methods for the treatment have become available. Various methods are used for the treatment of amblyopia in patients with ametropias and astigmatism. The major methods include optic correction, occlusion and various pleoptic methods. Modern pleoptic methods are based on stimulation of the central and peripheral retina using structured patterns that can be static or dynamic and achromatic or chromatic [8]. Physiotherapeutic adjuncts (transcutaneous electric or magnetic stimulation of the retina and optic nerve, vasolidator drug magnetophoresis or electrophoresis, stimulation of reflexogenic areas (reflexotherapy), acupressure, vibrostimulation, etc.) are used to improve the efficacy of treatment for amblyopia [8, 9]. Of note that, to the best of our knowledge, there have been no reports on the studies on the efficacy of common pleoptic methods in the treatment of MA. This is due to the fact that the visual system capacity for resolution of complex optotypes is assessed using the criterion of minimum cognoscible, the smallest familiar figure that the person being tested can recognize. This criterion is an integral characteristic of the cortical mechanisms for visual perception, and does not allow determining meridional acuity. In this connection, additional methods should be used for the assessment of meridional resolution. The characteristics most commonly determined for this purpose are vernier acuity and separable acuity. The basic publications on the treatment of MA are related to the determination of the efficacy of optical correction and occlusion [10-13]. It was noted that a stable outcome of treatment of amblyopia (a visual acuity of at least 0.5) was maintained at 3-year follow-up only in 54% of patients [10, 14, 15]. In recent decades, there have been several reports on the development of device-based treatments for MA which allow the activation of meridional retinocortical pathways by adequate structured stimuli [16-20]. There has been proposed a method of treating MA by selective stimulation of the retinal meridian receptive fields with low visual acuity by black-and-white stripe patterns with a rectangular luminance profile [20]. The patterns were oriented perpendicularly with respect to principal astigmatic refraction meridians. The outcomes of treatment of amblyopia associated with hypermetropic astigmatism demonstrated the potential for improvement of corrected visual acuity. A reduction in the magnitude of asymmetry between visual acuities in orthogonal meridians was determined on the basis of peak-to-peak amplitudes of the P100 wave of visual evoked potentials [20]. Special computer video games were designed for the treatment of mild MA in patients with astigmatism, with stimulation of the amblyopic meridian by objects of various colors and various contrasts. The direction of the meridian to be stimulated was determined using a special marker presented to the patient playing the game [19]. Treatment efficacy was assessed using only the criterion of minimum cognoscible. Full improvement of LogMAR visual acuity up to 0.0 was seen in 36/50 (72.0%) oblique astigmatism eyes. Deshpande and colleagues [19] concluded that satisfactory improvement in VA in eyes with residual MA provided preliminary data into the effectiveness of stimulation of the precise amblyopic axis by astigmatism axis video games in conjunction with spectacles and “minimal patching” regimen of 2 h/day, and further comparative study was warranted. It has been reported on the effect of modified computer games on meridional acuity in patients with astigmatism associated with amblyopia. A game was performed by the patient, while the foveal and macular region of his or her amblyopic eye was stimulated by the sinusoidal drifting grating pattern in the background of the computer screen. In another game performed by the patient, the grating pattern remained still with respect to the playing pattern [16-18]. It is noteworthy that these amblyopia treatment methods do not provide for selective stimulation of the amblyopic meridian. Method efficacy was assessed based on changes in meridional Landolt acuity (the criterion of minimum separable). There was an improvement in corrected meridional acuity after treatment with the game using the sinusoidal drifting grating pattern, with a more pronounced improvement of visual acuity noted in the meridian with maximum ametropia. No statistically significant improvement was observed after exercises with the stationary grating [18]. Because the authors of the above methods varied in the criteria used to assess outcomes of treatment of MA, it is rather difficult to determine the most effective method of treatment of MA. It may be, however, supposed that the use of selective meridional stimulation is not necessary for achieving a positive treatment outcome. Because there has been no study to assess in detail the efficacy of modern pleoptic methods in the treatment of MA, it is expected that an effective increase in meridional acuity can be achieved with the use of well-established pleoptic methods. The research in this area can only be successful if the method of determination of meridional acuity is included in the standard examination of patients. This approach will allow determining the most effective methods for the treatment of MA and justifying the need for developing methods involving application of selective light stimulation. It is noteworthy that the problem of selecting the optimum pleoptic method emerges not only with regard to the treatment of MA, but also with regard to the treatment of various forms of amblyopia. Some authors believe that the use of complex equipment and complex methods is not always justified, since comparable outcomes can be achieved with the use of readily available and rather simple devices [8, 9]. The purpose of the present study was to assess the effect of optical-reflection method of accommodative facility training on vernier acuity in meridians (MVA) in astigmats with amblyopia. Optical reflection methods are based on stimulation of the accommodation reflex by image defocusing either using optical lenses of a variable power or due to changing the distance between the object and the eye. Accommodation apparatus training is a pathogenetically relevant therapy and facilitates an improvement in VA in the amblyopic eye in 40%-76.9% of patients with hyperopic amblyopia [21, 22, 23]. The method is easy to use it at home, which is helpful in ensuring continuity of treatment and sustainability of treatment outcomes. We used vernier acuity to assess the effect of accommodation apparatus training on meridional acuity. Vernier acuity is a major criterion allowing to assess the visual system capacity to analyze complex patterns [3, 24]. Special attention should be paid to the principle of the formation of homogeneous groups in order to avoid errors while assessing the results of treatment of amblyopia associated with astigmatism. The selection procedures for the formation of homogeneous groups should take into consideration the interrelation of the magnitude and direction of astigmatism-associated refractive asymmetries with the magnitude and direction of meridional asymmetries of vernier acuity [25, 26]. Now we will consider in detail the reason for this requirement. It is known from physiological optics that, in direct astigmatism, vertical lines appear most clear, whereas in inverse astigmatism, horizontal lines appear most clear. Consequently, in direct astigmatism, visual acuity will be higher in the horizontal meridian, whereas in inverse astigmatism, visual acuity will be higher in the vertical meridian. However, this is not always true. In patients with amblyopia and similar type of astigmatism, the magnitude and direction of meridional asymmetries in vernier acuity (MVA) may differ from the magnitude and direction of refractive asymmetries [26]. It was found possible to split such a group of patients into clusters that differ in the direction of asymmetry in meridional visual acuity from the direction of refractive asymmetries. One cluster may have vernier acuity in the horizontal meridian better than in the vertical meridian, the second may have vernier acuity in the horizontal meridian worse than in the vertical meridian, and the third may have equal vernier acuities in the vertical and horizontal meridians. Variations in the directions of meridional asymmetries in vernier acuity are likely to be due to continuous changes in the type of refraction in the course of visual system development as well as changes in the conditions of sensor system adaptation to astigmatism. Therefore, an assessment of the efficacy of treatment of MA should be performed separately in homogeneous clusters. Failure to take this factor into account during statistical analysis of MVA for the main study sample will remove the asymmetries in visual acuity which differ from each other in direction, and the mean value will provide wrong evidence of the absence of meridional amblyopia. A change in the type of meridional asymmetries in vernier acuity as a result of treatment of astigmatism-related amblyopia is a potential marker of treatment efficacy. The purpose of the present study was to assess the effect of optical-reflection method of accommodation facility training on MVA in the treatment of astigmatic children with amblyopia. Material and Methods Twenty seven children aged 5 to 12 years, with both refractive amblyopia and with-the-rule hyperopic astigmatism were included in the study, and underwent examination. Simple hyperopic astigmatism was found in 27 eyes, and compound hyperopic astigmatism in 26 eyes. The spherical component of refraction ranged from 0.5D to 5.5D, and the cylindical component, from 0.5D to 4.5D. Best-corrected visual acuity (Sivtsev Chart) was assessed in relative terms. Worth’s four-dot test was used to determine the type of binocular vision. Refraction was assessed by a Topcon auto refractometer. Mild amblyopia was found in 48 eyes (91% of patients), and moderate amblyopia in 5 eyes (9% of patients). Before treatment, mean uncorrected visual acuity (UCVA) and mean best-corrected visual acuity (BCVA) as assessed by the Golovin-Sivtsev Chart were 0.48 ±0.02 and 0.65±0.02, respectively. Special computer software was used to determine corrected MVA in arc seconds at a distance of 5 m. Linear objects were oriented in the horizontal and vertical meridians and presented on the computer screen. One of linear objects could be displaced gradually with respect to another. Smallest lateral displacement of one line from another that can be detected by the examinee will characterize the level of MVA. The stimuli were presented monocularly on a 15-inch screen at a resolution of 1,600×1,200 pixels. At this resolution, the displacement per pixel was 0.12 arc sec. Because MVA is characterized by angular units (arc deg, arc min and arc sec), a decrease in absolute value corresponds to an increase in visual acuity, and vice versa. Vertically oriented linear tests are used to assess vernier acuity in the horizontal meridian, whereas horizontally oriented linear tests are used to assess vernier acuity in the vertical meridian. Accommodative facility training was performed monocularly by image defocusing with lenses of a variable power. A smallest resolvable line of optotypes of the distant chart was presented to the patient, and a +0.5-diopter sphere was placed just in front of the best correction for the study eye in order to blur this line. The +0.5-D sphere was replaced by a -0.5-D sphere after the optotypes became clearly visible. Each of the above-mentioned lenses was presented 10 times. Thereafter, the cycle was repeated using a ±0.75-D sphere and, subsequently, a ±1.0-D sphere. If the patient succeeded in fulfilling the task, lens power was gradually increased in increments of 0.25D or 0.5D until it could be compensated by accommodation. The treatment course consisted of 10 sessions. The study adhered to national bioethics regulations and the tenets of the Declaration of Helsinki of 1975 as revised in 2000. Informed consent of children as well as written informed consent of their parents was obtained. Statistical analyses were conducted using Statistica for Windows 7.0 (StatSoft, Tulsa, OK, USA) software. Mean values and standard deviation (σ) values were calculated. Student t test for dependent samples was used to determine the significance of difference between patient’s post-treatment and pretreatment data. The level of significance p ≤ 0.05 was assumed. The Mann-Whitney test was also used for statistical analysis. Results Table 1 shows the distribution of eyes of patients with hyperopic astigmatism among various visual acuity categories before and after accommodative facility training with the use of positive and negative spherical lenses. After treatment, the number of dominant eyes increased by 3.78%, and the number of fellow eyes, by 7.57%, for the category of patients with a visual acuity of 0.75-0.8 (as assessed by minimum cognoscible) (Table 1).
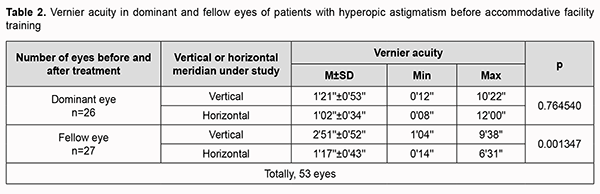
Table 2 presents values of MVA for patients with both refractive amblyopia and with-the-rule hyperopic astigmatism. Asymmetries between MVA in orthogonal retinal meridians can be a marker of MA. Mean MVA were practically similar in horizontal and vertical meridians (p=0.76) for the dominant eye, and significantly different for the fellow eye (p<0.0013). This makes one think that meridional amblyopia is present in the fellow eyes but not in the dominant eyes. However, a large range between maximum and minimum values for the dominant eyes suggests that meridional asymmetries in vernier acuity may be present not only in the fellow eyes but also in the dominant eyes. Meridional asymmetries in vernier acuity should be considered as vector quantities since there may be differences both in magnitude and direction.
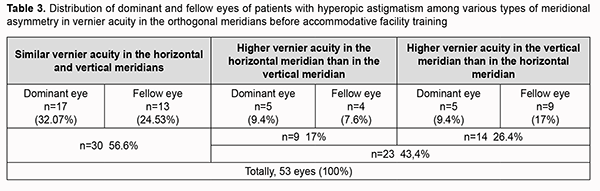
Table 3 shows the distribution of patients with with-the-rule hyperopic astigmatism depending on the type of meridional asymmetry in vernier acuity in the orthogonal meridians for the dominant and fellow eyes before treatment. The table demonstrates that the study sample was not homogeneous with regard to the types of meridional asymmetry in vernier acuity in the orthogonal meridians for the dominant and fellow eyes. MVA values in the orthogonal meridians were similar, showing no meridional amblyopia, in 56.6% of study patients. Meridional asymmetries in vernier acuity (i.e., meridional amblyopia) in the dominant eyes and fellow eyes were found in 43.4% of patients. This subgroup can be subdivided into two clusters which differ in both the magnitude and direction of meridional asymmetries in visual acuity. MVA was greater in magnitude in the horizontal meridian than in the vertical meridian in one of these clusters (17% of study eyes) and greater in magnitude in the vertical meridian than in the horizontal meridian in another cluster (26.4% of study eyes).
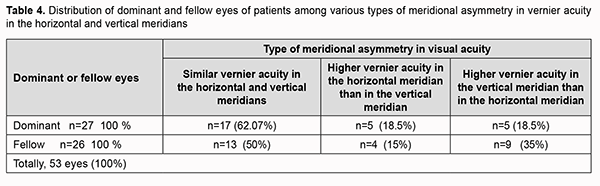
Table 4 demonstrates the results of a more detailed analysis of meridional asymmetries in vernier acuity which was performed separately for the dominant and fellow eyes. MVA values in the orthogonal meridians were similar in the dominant eyes in 62% of study patients, and in the fellow eyes in 50% of study patients (Table 4). In addition, MVA was greater in magnitude in one of the orthogonal meridians than in another in the dominant eyes in 37% of study patients, and in the fellow eyes in 50% of study patients. It is noteworthy that apparent meridional amblyopia was identified only in the fellow eyes, and latent meridional amblyopia, in the dominant eyes, when processing the data without taking the type of meridional asymmetry in vernier acuity into consideration (Table 2). Interestingly that visual acuity was greater in magnitude in the vertical meridian than in the horizontal meridian in the dominant eyes in 35% of study patients, and in the fellow eyes in 18% of study patients.
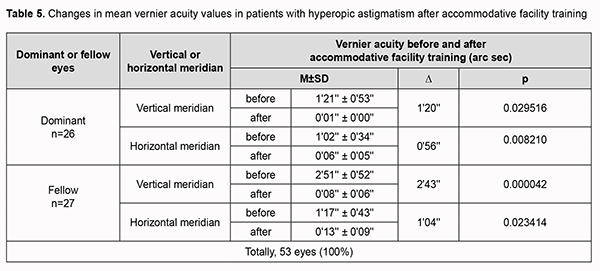
Table 5 presents the data on the influence of accommodation training on MVA values in patients with with-the-rule hyperopic astigmatism. Accommodation training was beneficial for MVA values in the orthogonal meridians both in the dominant and fellow eyes (Table 5). While treating for MA, attention should be paid not only to an increase in the magnitude of MVA, but also to changes in the type of asymmetry. Elimination as well as a change in the type of asymmetry in MVA is an important marker of treatment efficacy.
Table 6 shows changes in the type of asymmetry in MVA in the orthogonal meridians after accommodation training. There was a 15.1-percent increase in the number of eyes with similar vernier acuity in the orthogonal meridians after accommodation training (Table 6). This was achieved through elimination of meridional asymmetry in vernier acuity in a portion of patients from clusters with different directions of asymmetry in vernier acuity. There was a 9.4-percent decrease in the number of eyes with asymmetry for the cluster in which MVA was greater in magnitude in the vertical meridian than in the horizontal meridian. In addition, there was a 5.7-percent decrease in the number of eyes with asymmetry for the cluster in which MVA was greater in magnitude in the horizontal meridian than in the vertical meridian.
Discussion MA can cause serious abnormalities in monocular and binocular mechanisms of integrated processing of visual stimulus. Various methods have been proposed for the treatment of MA. Some of them used patterns for selective stimulation of the amblyotic meridian, and some others, the principle of simultaneous light stimulation of the foveal and macular regions. Although these methods vary in the methodology employed, they allowed improving meridional visual acuity. Because there has been no study to assess in detail the efficacy of modern pleoptic methods in the treatment of MA, it is expected that an effective improvement in meridional acuity can be achieved with the use of well-established pleoptic methods. The research in this area can only be successful if the method of determination of meridional acuity is included in the standard examination of patients with amblyopia. This approach will allow determining the most effective methods for the treatment of MA and justifying the need for developing methods involving application of selective light stimulation. The purpose of the present study was to assess the influence of optical-reflection method of accommodative facility training on MVA in patients with astigmatism associated with amblyopia. The method is easy to use it at home, which is helpful in ensuring continuity of treatment and sustainability of treatment outcomes. We employed a new algorithm of assessment of meridional asymmetry in vernier acuity before and after treatment in order to determine the efficacy of this method. The algorithm considers asymmetries in refraction and MVA in the orthogonal coordinates as vector quantities. This approach allowed demonstrating that a group of patients with the same type of astigmatism was not homogeneous in terms of the direction of meridional asymmetry in vernier acuity compared to refractive asymmetry [25, 26]. It was found possible to split such a group of patients into three clusters that differ in the type of variation in MVA in the orthogonal meridians. One cluster may have vernier acuity in the horizontal meridian better than in the vertical meridian, the second may have vernier acuity in the horizontal meridian worse than in the vertical meridian, and the third may have equal vernier acuities in the vertical and horizontal meridians. Analysis of meridional asymmetries in vernier acuity with consideration of their distribution in clusters provided principally new information on the features of adaptation of the sensory system to astigmatism. No MA was found in 50% of study patients. MVA values in the orthogonal meridians were similar in the dominant eyes in 62% of study patients, and in the fellow eyes in 50% of study patients. In addition, MVA was greater in magnitude in one of the orthogonal meridians than in another in the dominant eyes in 37% of study patients, and in the fellow eyes in 50% of study patients. It is noteworthy that apparent meridional amblyopia was identified only in the fellow eyes, and latent meridional amblyopia, in the dominant eyes, when processing the data without taking the type of meridional asymmetry in vernier acuity into consideration (Table 2). The presence of meridional asymmetries in vernier acuity in the dominant eyes and fellow eyes makes it possible to treat these asymmetries as a binocular disorder. An increase in MVA in the orthogonal meridians and a change in the type of meridional asymmetries in vernier acuity were used as criteria of the efficacy of treatment of MA in patients with astigmatism. Elimination of meridional asymmetry in vernier acuity is one of the most important criteria of the efficacy of treatment. Our treatment resulted in an improvement in MVA in all subgroups of study patients. Particularly, there was a 15.1-percent increase, from 56.6% to 71.1% in the number of eyes with similar vernier acuity in the orthogonal meridians after accommodation training. This was achieved through elimination of meridional asymmetry in vernier acuity in a portion of patients from clusters with different directions of asymmetry in vernier acuity. In addition, the number of eyes in the category of patients with a visual acuity of 0.75-0.8 (as assessed by Sivtsev Chart) increased by 11.35%. Conclusion An improvement in integral and selective visual acuity as a result of accommodation training treatment for amblyopia allows considering this training as a method of treatment for MA. In order to avoid errors while assessing the results of treatment of amblyopia associated with astigmatism, it should be taken in account that a group homogeneous with regard to the type of astigmatism will be not homogeneous with regard to the direction of meridional asymmetry in visual acuity. The method of determination of selective meridional acuity should be included in the standard examination of patients with amblyopia. The algorithm proposed for assessing meridional asymmetries in visual acuity will permit a more detailed assessment of the efficacy of well-established pleoptic methods in the treatment of MA in patients with astigmatism and provide justification for developing special methods.
References 1. Dobson V, Miller JM, Harvey EM, Mohan KM, et al. Amblyopia in astigmatic preschool children. Vis Res. 2003 Apr;43(9):1081–90. 2. Gwiazda J, Bauer J, Thorn F, Held R. Meridional amblyopia does result from astigmatism in early childhood. Clinical Vision Science. 1986;1:145–52. Hubel DH. Eye, brain, and vision New York: Scientific American Library;1988. 3.Freeman RD, Mitchell DE, Millodot M. A Neural Effect of Partial Visual Deprivation in Humans. Science. 1972 Mar 24;175(4028):1384-6. 4.Mitchell DE, Freeman M, Millodot M, Haegerstrom G. Meridional amblyopia: evidence for modification of the human visual system by early visual experience. Vision Res. 1973 Mar;13(3):535-8. 5.Vit VV. [The structure of the human visual system] Odessa: Astroprint; 2003. 6.Polat U, Bonneh Y, Ma-Naim T, et al. Spatial interactions in amblyopia: Effects of stimulus parameters and amblyopia type. Vision Res. 2005 May;45(11):1471-9. 7.Lavrent’ev BF, Rozhentsov VV. [Instrumental treatment of amblyopia]. Ophthalmology in Russia. 2016;13(3):144–50. doi: 10.18008/1816–5095–2016–3–144–150. Russian.Crossref 8. Botabekova TK, Kurgambekova NS.. [A comparative analysis of the efficiency of different methods in the treatment of amblyopia]. Vestn Oftalmol. 2004 Sep-Oct;120(5):40-1. Russian. 9.Abrahamsson M, Sjöstrand J. Astigmatic axis and amblyopia in childhood. Acta Ophthalmol Scand. 2003 Feb;81(1):33–7. 10. Harvey EM, Dobson V, Miller JM, Clifford-Donaldson CE. Amblyopia in astigmatic children: patterns of deficits. Vision Res . 2007; 47: 315–26. 11. Harvey EM. Development and Treatment of Astigmatism-Related Amblyopia. Optom Vis Sci. 2009 Jun;86(6):634-9. 12. Harvey EM, Dobson V, Clifford-Donaldson CE, Miller JM.Optical treatment of amblyopia in astigmatic children: the sensitive period for successful treatment. Ophthalmology. 2007 Dec;114(12):2293-301. 13. Flynn JT. Amblyopia: its treatment today and its portent for the future. Binocul Vis Strabismus Q. 2000;15(2):109. 14. Flynn JT, Cassady JC. Current trends in amblyopia therapy. Ophthalmology. 1978;85:428-50. 15. Kämpf U, Mascolus W, Muchamedjarow F, et al. Coherence induction via phase conjugate adaptive resonance coupling: Computer-generated sinusoidal grating patterns as a background stimulus in amblyopia treatment. J Psychophysiology. 2006; 20(2):149. 16. Kampf U, Shamshinova A, Kaschtschenko T, et al. Long-term application of computer-based pleoptics in home therapy: selected results of a prospective multicenter study. Strabismus. 2008;16(4):149-58. 17. Kempf W, Rychkova SI, Haim E, Mukhamedyarov F. [Comparative results of the application of moving and fixed sinusoidal framework in functional treatment of amblyopia]. Tochka zreniia. Vostok-Zapad. 2016;3:140-43. Russian. 18. Deshpande PG, Bhalchandra PC, Nalgirkar AR, Tathe SR. Improvement of visual acuity in residual meridional amblyopia by astigmatic axis video games. Indian J Ophthalmol. 2018 Aug; 66(8): 1156–60. 19. Аznaurjan IE, Gorlacheva LI. LASIK in complex treatment of meridional form of refractive amblyopia in children with astigmatism. Refractive Surgery Updates. Italy, Venice, June 2002. р.112-3. 20. Boubaker Hafedh ВA. [Significance of accommodation therapy in complex treatment of children with different kinds of hypermetropic amblyopia]. [Abstract of a Thesis for the Degree of Cand Sc (Med)]. Filatov Institute of Eye Diseases and Tissue Therapy. Odesa, Ukraine; 1998. Russian. 21. Stalnov VS. [Effect of different pleoptic treatments on accommodation in pediatric disbinocular amblyopia]. [Abstract of a Thesis for the Degree of Cand Sc (Med)]. Krasnoiarsk; 2006. Russian. 22. Serdiuchenko VI, Gilko OV. [Efficacy of accommodation facility training in children with mixed astigmatism] In: [Proceedings of the International Conference on Myopia and Errors of Refraction, Accommodation, and Ocular Motility]. Moscow;2001. p.236-7. Russian. 23. Shamshinova AM, Volkov VV. [Functional methods of research in ophthalmology]. Moscow: Meditsina; 1999. Russian. 24. Kolomiyets V, Bandura M, Kolomiyets N. [Meridional vernier visual acuity in children and adults with hypermetropic astigmatism]. Oftalmologiia. Vostochania Evropa. 2015; 3(26):27-34. Russian. 25. Kolomiyets V, Bandura M, Kolomiyets N. [Peculiarities of vernier monocular and binocular visual acuity in the retinal orthogonal meridians in patients with hypermetropic astigmatism]. ScienceRise. 2015; 6/4(11):38-44. Russian. Conflict of Interest: Authors declare that there are no conflicts of interest that might influence their opinion on the subject matter or materials described or discussed in this manuscript.
|