J.ophthalmol.(Ukraine).2021;6:16-20.
|
http://doi.org/10.31288/oftalmolzh202161620 Received: 13 July 2021; Published on-line: 21 December 2021 Expression of lymphocyte activation markers CD 54 (ICAM-1), CD 5, CD 95 (FAS) and neutrophil activation marker CD15 in the peripheral blood of patients with intermediate uveitis and healthy individuals L. M. Velychko 1, O. V. Zborovska 1, N. B. Kuryltsiv 2, O. V. Bogdanova 1 1 SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the NAMS of Ukraine"; Odesa (Ukraine) 2 Danylo Halytsky Lviv National Medical University; Lviv (Ukraine) E-mail: kuryltsivnb@gmail.com TO CITE THIS ARTICLE: Velychko LM, Zborovska OV, Kuryltsiv NB, Bogdanova OV. Expression of lymphocyte activation markers CD 54 (ICAM-1), CD 5, CD 95 (FAS) and neutrophil activation marker CD15 in the peripheral blood of patients with intermediate uveitis and healthy individuals. J.ophthalmol.(Ukraine). 2021;6:16-20. http://doi.org/10.31288/oftalmolzh202161620
Background: Immunological abnormalities are implicated in the pathogenesis of inflammatory diseases of the uveal tract. Investigation of the molecular mechanisms of various forms of endogenous uveitis from the standpoint of current immunology seems to be relevant from the theoretical and practical standpoints. This will provide a direction for further research on the development of pathogenetically grounded methods of treatment of uveitis. Purpose: to assess the expression levels of lymphocyte activation markers, intercellular adhesion marker (ICAM)-1 CD54, СD95 (FAS), and СD5, and neutrophil activation marker CD15, in the peripheral blood of patients with intermediate uveitis and healthy individuals. Material and Methods: Blood samples were taken from 14 patients (mean age, 34.0 ± 11.0 years) with intermediate uveitis before treatment and 26 practically healthy individuals (mean age, 36.0 ± 10.0 years). An immunohistocytochemical study using monoclonal antibodies was employed to assess the expression. Results: Expression of cell surface molecular markers on peripheral blood lymphocytes was significantly higher in patients with intermediate uveitis compared with controls. Mean percentage and absolute values of СD54 (ICAM-1) expression were 29.6 ± 3.5% and 674.18 ± 63.4 cell/µL, respectively, for patients, versus 14.2 ± 3.1% and 674.18 ± 63.4 cell/µL, respectively, for controls; CD95 (FAS), 28.5 ± 4.9% and 534.2 ± 59.5 cell/µL, for patients, versus 18.9 ± 3.1% and 254.18 ± 42.1 cell/µL, respectively, for controls; CD5, 23.4 ± 4.1% and 622.8 ± 53.5 cell/µL, respectively, for patients, versus 10.3 ± 1.96% and 152.11 ± 10.13 cell/µL, respectively, for controls. CD15, a neutrophil activation marker, was significantly (Mann-Whitney test, p < 0.05) higher expressed in patients (mean percentage expression, 28.7 ± 5.8%; mean absolute expression, 980.19 ± 58.4 cell/µL), than in controls (mean percentage expression, 14.2 ± 3.1%; mean absolute expression, 165.5 ± 32.1 cell/µL). Increased expression of lymphocyte activation markers may indicate a failure of autotolerance mechanisms as well as excessive immune response leading to intraocular inflammation. In addition, increased expression of СD 54 (ICAM-1) and СD 95 (FAS) may be a prognostic sign for increased inflammation in the eye. Conclusion: Immunological status of patients with intermediate uveitis is characterized by significantly increased expression of molecular markers such as intercellular adhesion marker (ICAM)-1 CD54, apoptosis marker СD95 (FAS), lymphocyte autoactivation marker СD5, and neutrophil activation marker CD15. Further research of longitudinal changes in these characteristics may be important for predicting the course of inflammation over time and determining the therapy needed. Keywords: intermediate uveitis, lymphocyte activation markers, СD54 (ICAM-1), СD5, СD95 (FAS), СD15
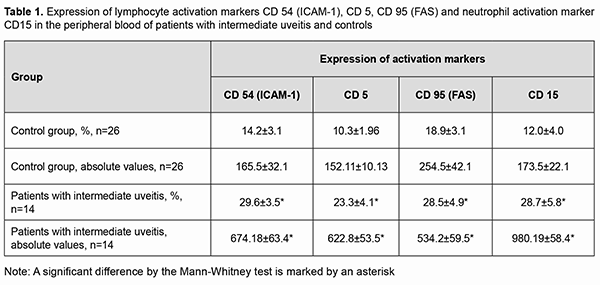
Introduction Intermediate uveitis is one of the most severe forms of ocular inflammatory disease and characterized by an intricate pathogenesis and a high rate of complications. Uveitis is the fifth leading cause of visual impairment in developed countries and responsible for about 20% of legal blindness [1]. The issue is socially important, because the disease affects working-age population, and its consequences cause limitations in subsequent professional activities and the potential for living an active life. Some authors believe that immunological abnormalities are implicated in the pathogenesis of a considerable range of inflammatory diseases of the uveal tract [1-3]. There is paucity of knowledge on the mechanisms of inflammatory process, features of the immunopathogenesis, character and type of immunological abnormalities, immunological criteria for predicting a chronic course and recurrence in intermediate uveitis. Uveitis runs a complicated course when there are abnormalities in cellular and humoral systemic immunity [2, 4]. Neutrophils and macrophages are known to migrate to the focus of inflammation when cellular immunity is activated. Activated cells produce cytokines which are implicated in systemic and local immune response. Studies on immune-mediated uveal inflammatory response are important. The purpose of the study was to assess the expression levels of lymphocyte activation markers, intercellular adhesion marker (ICAM)-1 CD54 and apoptosis (or programmed cell death) marker СD95 (FAS), and neutrophil activation marker CD15, in the peripheral blood of patients with intermediate uveitis and healthy individuals. Material and Methods An immunohistocytochemical study using monoclonal antibodies (the peroxidase anti-peroxidase method) was employed to assess the expression of lymphocyte and neutrophil activation markers in 14 patients (mean age, 34.0 ± 11.0 years) with intermediate uveitis and 26 practically healthy individuals (mean age, 36.0 ± 10.0 years) [5]. Blood was collected from the medial cubital vein using a disposable vacuum collection tube system. Clear lymphocyte and neutrophil suspensions were obtained and supplemented with monoclonal antibodies of various specificity levels [5]. The monoclonal antibody panel (MCAP) for immunophenotyping included antibodies reacting with СD5, СD54 (ICAM-1), СD95 (FAS), and СD15 antigens. Immunophenotyping was performed using immunohistochemistry; applying stains to cells that were fixed on a glass slide and then evaluating them under the microscope. CD54 (ICAM-1) is an important member of the immunoglobulin superfamily (IgSF) of proteins (molecular weight, 90-110 kDa). It is highly expressed on cell surface of leucocytes and activated endothelial cells, and regulates leucocyte migration to inflammatory sites. CD54 expression can be induced on leucocytes, neutrophils, macrophages, epithelial and endothelial cells and fibroblasts by stimulation with cytokines such as interleukin (IL)-1, tumor necrosis factor (TNF), and interferon (IFN)γ. Expression of these molecules can be either constant or inducible. СD95 (FAS) is the 45 kDa apoptosis antigen (or FAS antigen) that mediates apoptosis. FAS is a transmembrane molecule and a member of the TNF receptor superfamily, and is highly expressed on activated T cells and B cells. CD5 is a phenotypic lymphocyte marker in autoimmune disease, a 67-kDa transmembrane glycoprotein that is expressed on mature T cells and B cells and on most thymocytes. CD15 is a neutrophil activation marker and expressed on mature granulocytes, monocytes, and normal and leukemic myelomonocytes [6]. The study followed the ethical standards stated in the Declaration of Helsinki and relevant laws of Ukraine. Statistical analyses were conducted using Statistica 6.0 for Windows (StatSoft, Tulsa, OK, USA) software. Analysis of variance (ANOVA) was used and mean and standard error of mean were calculated. Mann Whitney U test was employed to investigate group differences. Results We assessed expression levels of lymphocyte activation markers СD5, СD54 (ICAM-1), and СD95 (FAS), and of neutrophil activation marker СD15, in patients with intermediate uveitis and healthy controls. СD54 (ICAM-1) was significantly (Mann-Whitney test, p < 0.05) higher expressed on lymphocytes of 14 patients with intermediate uveitis (mean percentage expression, 29.6 ± 3.5%; mean absolute expression, 674.18 ± 63.4 cell/µL), than on lymphocytes of 26 healthy individuals (mean percentage expression, 14.2 ± 3.1%; mean absolute expression, 674.18 ± 63.4 cell/µL). The results are presented in Table 1.
ICAM-1 is currently considered a functional biomarker of inflammation, with a main function of providing adhesion of neutrophils, monocytes and lymphocytes to activated vascular endothelium, with their subsequent migration to sites of inflammation; therefore, a significantly increased expression of this marker indicates intraocular inflammatory activity in the group of patients with intermediate uveitis. In addition, СD 95 (FAS), a molecular apoptosis marker, was significantly (Mann-Whitney test, p < 0.05) higher expressed on lymphocytes of 14 patients with intermediate uveitis (mean percentage expression, 28.5 ± 4.9%; mean absolute expression, 534.2 ± 59.5 cell/µL), than on lymphocytes of 26 healthy individuals (mean percentage expression, 18.9 ± 3.1%; mean absolute expression, 254.18 ± 42.1 cell/µL). Moreover, CD15, a neutrophil activation marker, was significantly (Mann-Whitney test, p < 0.05) higher expressed in 14 patients with intermediate uveitis (mean percentage expression, 28.7 ± 5.8%; mean absolute expression, 980.19 ± 58.4 cell/µL), than in 26 healthy individuals (mean percentage expression, 14.2 ± 3.1%; mean absolute expression, 165.5 ± 32.1 cell/µL). When the blood ocular barrier in the affected eye is disrupted, tissue-specific antigens enter the ocular circulation, and tissue-specific autoantibodies appear in blood [3]. CD5, an autoimmune activation marker, was significantly (Mann-Whitney test, p < 0.05) higher expressed in 14 patients with intermediate uveitis (mean percentage expression, 23.4 ± 4.1%; mean absolute expression, 622.8 ± 53.5 cell/µL), than in 26 healthy individuals (mean percentage expression, 10.3 ± 1.96%; mean absolute expression, 152.11 ± 10.13 cell/µL). The data obtained indicated that the autoimmune component is involved in inflammation in patients with the disease. Analysis of the number of cells expressing markers of early and late activation allows characterizing the type, power and nature of immune response in intermediate uveitis. Therefore, our study demonstrated significant increases in expression of CD5, a molecular marker of autoactivation of lymphocytes, CD54 (ICAM-1), intercellular lymphocyte adhesion molecule, СD 95 (FAS), a molecular apoptosis marker, and CD15, a neutrophil activation marker, in patients with intermediate uveitis compared to healthy controls. Discussion There is currently no doubt that the immune system has an important role in the onset and development of uveitis. In uveitis, the vascular coat of the eye may be a target for immune reactions [7]. It had been reported that memory T cells can stay in the vitreous, iris, ciliary body and choroid for long periods and participate in the development of recurrent intraocular inflammation. Increased permeability of capillaries and an increased number of neutrophils lead to increased vascular permeability and acute destructive process [8]. As immune dysfunction plays a role in the development of intraocular inflammation [9], the assessment of the activity of (a) molecular markers of cell surface expression of lymphocytes and (b) markers of the activity of neutrophils in peripheral blood seems important for further research on the pathogenesis as well as the development of effective means for immunocorrective therapy in uveitis. To the best of our knowledge, the literature is scant on this issue. It has been reported recently that high CD54 expression correlated with the presence of inflammation in autoimmune disease [3]. The pathogenetic mechanisms of uveitis involve an intricate complex of immune responses, with the immune system playing not necessarily a protective or limiting role. A hyperactive immune response implies the development of immunopathological reactions and destructive processes in ocular tissues with unfavorable prognosis. The results of our studies on the expression of molecular markers of lymphocyte activation in peripheral blood of patients with intermediate uveitis are in agreement with the results obtained in studies on patients with anterior uveitis [4]. CD54 (ICAM-1) and CD 95 (FAS) expression levels were higher in patients with chronic uveitis than in patients with unfavorable outcome of inflammatory process [4]. In the course of inflammation, substantial CD54 (ICAM-1) expression is observed not only on cells of the lymphatic system, but also on endothelial and tissue cells. The CD54 (ICAM-1) molecule is also involved in contact cell interactions of T cells with monocytes and of cytotoxic T cells with target cells in immune responses. CD54 (ICAM-1) is important for lymphocyte migration from the blood through the vascular endothelium to lymphatic nodes or inflamed tissues such as the ocular surface [3]. Activated lymphocytes involved in inflammatory immune responses subsequently undergo apoptosis through FAS receptor ligation. Apoptotic signaling is induced in cells on binding of Fas ligand to its receptor, Fas. A caspase cascade is initiated, leading to death of the Fas-expressing cell [10]. Studies on a pathogenetic role of failures in the molecular mechanisms of apoptosis in the development of various diseases have an important role in current experimental and clinical medicine [11]. It has been reported that there is an interrelationship between failures in the regulation of apoptosis and the development of cancer and inflammatory diseases accompanied by reduced efficacy of immune surveillance [12]. The literature is, however, scant on studies on apoptosis in intermediate uveitis. There is a need of increased knowledge of the pathogenesis of uveitis to reduce complication risks, disease recurrence rate, and the rate of visual disability caused by the disease. Improved understanding of the molecular pathogenesis of intermediate uveitis may be helpful in identification of new therapeutic targets for early treatment of uveitis. It has been reported that there was an increase in the number of cells with late CD95 (FAS) activation markers on their surface both in patients with uveitis of mixed etiologies and in those with monoviral uveitis. In addition, the severity of immunological lesions correlated with the severity of clinical findings [13]. The current study found that percentage and absolute values of expression of lymphocyte activation markers, intercellular adhesion marker (ICAM)-1 CD54, apoptosis (or programmed cell death) marker СD95 (FAS), and lymphocyte autoactivation marker СD5, and neutrophil activation marker CD15, in the peripheral blood were significantly higher than normal in patients with intermediate uveitis. Thus, these increases can be considered as an indicator of inflammatory process in uveitis inflammation. Further research on the expression of early and late lymphocyte and neutrophil activation and interaction markers would extend our knowledge of the pathogenesis and chronicity of uveitis. Conclusion Immunological abnormalities in intermediate uveitis are characterized by significantly increased expression of molecular markers such as intercellular adhesion marker (ICAM)-1 CD54, apoptosis (or programmed cell death) marker СD95 (FAS), lymphocyte autoactivation marker СD5, and neutrophil activation marker CD15. Further research of longitudinal changes in these characteristics may be important for predicting the course of inflammation over time and determining the therapy needed. Understanding the mechanisms of implementation and regulation of cell adhesion and apoptosis may be important for determining the treatment needed and predicting the course of intermediate uveitis. References 1.Khramenko NI, Konovalova NV. Findings of ocular and brain hemodynamics in patients with anterior uveitis complicated by macular edema. J Ophthalmol (Ukraine). 2020;4:14-22. Russian. 2.Kamilov KhM, Fayzieva DB. [On the specific and nonspecific immune responsiveness in patients with endogenous uveitis]. Ophthalmology in Russia. 2013;10(4):45-48. Russian. 3.Forrester JV, Kuffova L, Dick AD. Autoimmunity, autoinflammation, and infection in uveitis. Am J Ophthalmol. 2018 May;189:77-85. 4.Khramenko NI, Usov VY, Konovalova NV, Velychko LM, Bogdanova OV. Peculiarities of expression of the ICAM-1 intercellular adhesion molecule marker and CD-95 apoptosis marker in patients with uncomplicated anterior uveitis and complicated macular edema. DOG 2020. Poster 387. p. 163-4. 5.Gluzman DF, Skliarenko LM, Nadgornaia VA, Kriachok IA. [Immunocytochemistry in tumor diagnosis]. Kyiv: Morion; 2003. Russian. 6.Sidorenko SP. [Human cell surface antigens systematized by international workshops on human leucocyte differentiation antigens]. Imunologiia i alergologiia. 1998;3:16-38. Russian. 7.Rosenbaum JT, Kim HW. Innate immune signals in autoimmune and autoinflammatory uveitis. Int Rev Immunol. 2013 Feb;32(1):68-75. 8.Iuldasheva SA, Karim-Zade KhD, Satorov S. [Current view on the etiology, pathogenesis and prevalence of uveitis]. Vestnik Avitsenny. 2015;1:141-6. Russian. 9.Zemskov AM, Zemskov VM, Karaulov AV. [Clinical Immunology]. Moscow: GEOTAR-Media, 2008. Russian. 10.Filchenkov AA, Stepanov IuM, Lipkin VM. [Involvement of FAS/FASL system in homeostasis regulation and immune system cell function]. Alergologiia i imunologiia. 2002;3(1):24-35. Russian. 11.Velychko LN. [Expression of molecular markers of lymphocyte activation in peripheral blood of patients with uveal melanoma with various efficacy of organ-preserving treatment]. Oftalmol Zh. 2013;5:9-13. Russian. 12.Poliakova SI, Velychko LN, Bogdanova AV, at al. [Comparison of expression of molecular markers of lymphocyte activation in peripheral blood of patients with small T1 choroidal melanoma and healthy controls]. Oftalmol Zh. 2017;1:25-8. Russian. 13.Guliamova, Rizopulu AP, Kamilov HM, et al. [Immunological characterization of patients with chronic uveitis caused by herpetic vruses and/or cytomegalovirus]. Meditsinskaia immunologiia. 2005;7(5-6):543-50. Russian. Conflict of Interest: The authors declare no conflict of interest which could influence their opinions on the subject or the materials presented in the manuscript.
|