J.ophthalmol.(Ukraine).2020;4:3-7.
|
http://doi.org/10.31288/oftalmolzh2020437 Received: 28 April 2020; Published on-line: 27 August 2020 Intraventricular hemorrhage as a risk factor for retinopathy of prematurity S.V. Katsan, A.O. Adakhovska, E.S. Budivska SI "The Filatov Institute of Eye Diseases and Tissue Therapy of the National Academy of Medical Sciences of Ukraine"; Odesa (Ukraine) E-mail: adakhovskayaa@gmail.com
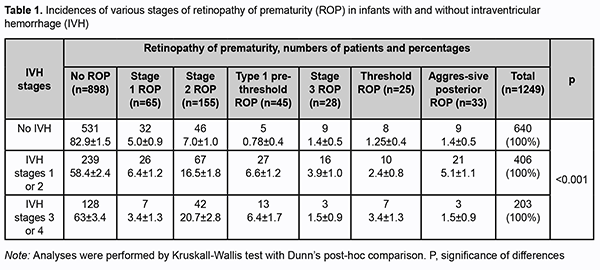
TO CITE THIS ARTICLE: Katsan SV, Adakhovska AO, Budivska ES. Intraventricular hemorrhage as a risk factor for retinopathy of prematurity. J.ophthalmol.(Ukraine).2020;4:3-7.http://doi.org/10.31288/oftalmolzh2020437 Background: Practically any body system in the premature infant is at risk of injuries, with the leading ones being perinatal central nervous system injury and visual system injury. Purpose: To investigate the incidence of retinopathy of prematurity (ROP) in infants with intraventricular hemorrhage (IVH). Material and Methods: Eye examination records and neurosonograms of 1249 preterm infants were reviewed. All these infants underwent ROP screening in due time. The fundus was assessed as per the 2005 International Classification of Retinopathy of Prematurity (ICROP). Neurosonograms were performed on days 1 to 4, 10 to 14, and weeks 4 to 8 of life to obtain data on the presence of IVH. Intracranial intraventricular hemorrhage was classified as per ICD-10. In particular, subependymal hemorrhage (without intraventricular extension) was classified as Grade 1, and subependymal hemorrhage with intraventricular extension (bleeding into ventricle) was classified as Grade 2. In addition, subependymal hemorrhage with intraventricular extension with enlargement of ventricle was classified as Grade 3, and subependymal hemorrhage with intracerebral extension was classified as Grade 4. Statistical analyses were performed using MedCalc v.17.4 (MedCalc Software bvba, 1993-2017). Results: ROP was found in 351 infants. Of these, 65 had stage 1 ROP, 155 had stage 2 ROP, 45 had type 1 pre-threshold ROP, 28 had stage 3 ROP, 25 had threshold ROP, and 33 had aggressive posterior ROP (APROP). No ROP was found in 898 infants. Of the 1249 preterm infants, 609 had neurosonographic findings of IVH, including 406 infants with grade 1 or 2 (i.e., low-grade) IVH and 203 infants with grade 3 or 4 (i.e., high-grade) IVH. No IVH was found in 640 infants. Of the 406 infants with low-grade IVH, 58.4% had no ROP, 6.4% had stage 1 ROP, 16.5% had stage 2 ROP, 6.6% had type 1 pre-threshold ROP, 3.9% had stage 3 ROP, 2.4% had threshold ROP and 5.1% had APROP. Of the 203 infants with high-grade IVH, 63% had no ROP, 3.4% had stage 1 ROP, 20.7% had stage 2 ROP, 6.4% had type 1 pre-threshold ROP, 1.5% had stage 3 ROP, 3.4% had threshold ROP and 1.5% had APROP. Conclusion: Of the 640 infants without IVH, 82.9% were found to have no ROP, whereas of the 406 infants with low-grade IVH and 203 infants with high-grade IVH, 58.4% and 63%, respectively, were found to have no ROP. Infants with IVH had higher chances for developing ROP (OR=3.2; 95% CI, 2.5-4.2; p < 0.001). Infants with high-grade IVH had higher chances for developing particular stages and forms of ROP (stage 2 and threshold ROP) (OR=2.4; 95% CI, 1.7-3.35; p < 0.05). IVH was found to be a risk factor for developing ROP. Keywords: retinopathy of prematurity, intraventricular hemorrhage, risk factors
Introduction Rates of preterm births in the world have risen substantially over recent decades. Practically any body system in the premature infant is at risk of injuries. Perinatal central nervous system (CNS) injury is a leading cause of early morbidity in and found in 60% to 80% of premature newborns [1]. Ocular disorders and congenital ocular malformations are found five to ten times more frequently in early-age children born prematurely than in their peers born at full term [2-3]. Retinopathy of prematurity (ROP) is the third most common cause both of functional disability and eye disease leading to blindness in children. Optic nerve atrophy (32%), congenital cataract (20%), degenerative myopia (18%) and congenital glaucoma (4%) are other causes of both functional disability and eye disease leading to blindness in children [3]. ROP is, however, a major cause of preventable blindness in children worldwide [3]. Because of a high prevalence of and high rates of disability due to the disease, studies on etiologic factors of ROP are still relevant. The currently recommended ROP screening criteria include such items as gestational age and birth weight, but postnatal factors are not taken into account [4]. Therefore, the search for potential risk factors is still underway. Previously, we have reported on our studies on some of these potential risk factors. However, the neurological status of a preterm infant with perinatal CNS injury combined with ROP is still to be clarified. Intraventricular hemorrhage (IVH) is the most common degenerative disease found in 60% to 90% of preterm infants. The lower gestational age and birth weight, the more severe is IVH [5]. Contradictory reports [6-10] on the relationship between ROP and IVH prompted the present study. The purpose of this study was to investigate the incidence of ROP in infants with IVH. Material and Methods Eye examination records and neurosonograms of 1249 preterm infants were reviewed. All these infants underwent ROP screening in due time. The fundus was assessed as per the 2005 International Classification of Retinopathy of Prematurity (ICROP) [11]. Infants with ROP stage 4 or 5 were excluded from the study. Indirect ophthalmoscopy was conducted using a binocular ophthalmoscope, 30 D-lens, eyelid speculum and scleral depressor after topical anesthetic (alkain) was instilled. A combination of eye drops, 0.5% tropicamidum and 0.2% irifrin, was used to achieve mydriasis. Neurosonograms were performed on days 1 to 4, 10 to 14, and weeks 4 to 8 of life to obtain data on the presence of IVH. Intracranial intraventricular hemorrhage was classified as per ICD-10. In particular, subependymal hemorrhage (without intraventricular extension) was classified as Grade 1, and subependymal hemorrhage with intraventricular extension (bleeding into ventricle) was classified as Grade 2. In addition, subependymal hemorrhage with intraventricular extension with enlargement of ventricle was classified as Grade 3, and subependymal hemorrhage with intracerebral extension was classified as Grade 4 [12]. Statistical analyses were performed using MedCalc v.17.4 (MedCalc Software bvba, 1993-2017). Incidences of ROP are presented as percentages of infants with and without neurosonographic findings of IVH. Odds ratios (OR) and confidence intervals (CI) were calculated. Analyses were performed by Kruskall-Wallis test with Dunn’s post-hoc comparison [13]. Results ROP was found in 351 infants. Of these, 65 had stage 1 ROP, 155 had stage 2 ROP, 45 had type 1 pre-threshold ROP, 28 had stage 3 ROP, 25 had threshold ROP, and 33 had aggressive posterior ROP (APROP). No ROP was found in 898 infants. Of the 1249 preterm infants, 609 had neurosonographic findings of IVH, including 406 infants with grade 1 or 2 (i.e., low-grade) IVH and 203 infants with grade 3 or 4 (i.e., high-grade) IVH. No IVH was found in 640 infants. An association was found between IVH severity and stage of ROP (p < 0.001; Kruskal-Wallis test). Of the 203 infants with high-grade IVH, 20.7%, 6.4% and 3.4% were found to have stage 2 ROP, type 1 pre-threshold ROP, and threshold ROP, respectively, and 63% had no ROP (p < 0.05; Dunn’s test), OR=2.4 (95% CI, 1.7-3.35). In addition, of the 406 infants with low-grade IVH, 6.6%, 3.9% and 5.1% were found to have type 1 pre-threshold ROP, stage 3 ROP, and APROP, respectively, and 58.4% had no ROP. It is noteworthy that, of the 640 infants without IVH, 82.9% were found to have no ROP (Table 1).
Infants with IVH had higher chances for developing ROP (OR=3.2; 95% CI, 2.5-4.2) (Table 1). Discussion ROP is a well-known complication of preterm birth; the disease is associated with various visual disorders including blindness. The incidence of ROP in Ukraine has increased with the increasing survival rates for the smallest premature infants. Some ophthalmologists describe this phenomenon as “the third epidemic of ROP” [11]. In spite of careful maintenance of oxygen level in the inhaled air mixture and blood of newborns, 2% to 11.5% of preterm infants with birth weight of < 1000 g and 0.3% to 1.2% of those with birth weight of 1000 g to 1,500 g become blind after active ROP. ROP accounts for 11% to 18% among visually disabled individuals and for 3.4% among deaf-and-blind individuals [3]. Predicting ROP in Ukraine is difficult because ROP screening results vary, depending on social and economic factors and uncontrolled or unselective use of oxygen in preterm infants. Irrespective of etiological factors leading to ROP, the sequelae of the disease include not only eye disorders. As early as 1998, a Swedish population study by Jacobson et al [14] reported on major neurological/neurodevelopmental impairments like infantile cerebral palsy, mental retardation, autism and seizures in 27 preterm infants with stage 5 ROP. By that time it became clear that such children should be carefully assessed for the development of the nervous system. IVH is one of the most common nervous system disorders among preterm infants. Intraventricular hemorrhage originates in the subependymal germinal matrix, an area of the developing brain, and may extend to the ventricles [15] commonly at the head or body of caudate nucleus [16, 17]. The subependymal germinal matrix layer gradually thins as the fetus grows and develops, and is practically absent in full-term infants [18, 19]. Intracranial hemorrhage in preterm infants has a multifactorial genesis involving, in particular, antenatal, intranatal and postnatal factors. The majority of prominent neonatology researchers (Volpe, Whitelaw, De Vries [16, 17]) believe that postnatal factors are more important than antenatal and intranatal factors in the pathogenesis of the condition, since in the vast majority of cases IVH is a postnatal phenomenon. An intrauterine infection (especially, an intrauterine viral infection) is the most important antenatal factor. Intranatal factors include detachment of the placenta, precipitated labor, disseminated intravascular coagulation syndrome in the mother, etc. Postnatal factors include artificial pulmonary ventilation with high positive inhalation pressure, massive intravenous infusions of hyperosmolar solutions, multiple invasive studies, and non-compliance with guidelines regarding temperature, humidity and protective measures. It is supposed that prematurity, intrauterine hypoxia and mechanical forces jointly impact the development of IVH when the fetus passes through the birth canal, although many researchers challenge the role of mechanical forces in the development [5]. Numerous studies demonstrated correlation of the development of IVH with ROP. Thus, Procianoy et al [20] reported on the statistically significant association between cicatricial ROP and IVH in very low birth infants. Hungerford and colleagues [21] found that ROP was strongly associated with evidence of brain damage, often consistent with hypoxic ischemic injury. Brown and co-authors [6] confirmed the strong association of ROP with bronchopulmonary dysplasia, low birth-weight, and IVH. Charles et al [22] reported that the presence of IVH, low birth weight, short gestation period, and extended supplemental oxygen administration period were significant factors in the development of ROP. O’Keefe et al. [9] documented ocular outcome in 68 premature infants with IVH. The incidence of ocular abnormalities was compared between low grade IVH (grade 1 and 2) and high grade IVH (grade 3 and 4). Of the 68 infants with IVH, ROP occurred in 33 infants (48.5%); 13 (43.3%) had low grade IVH; 20 (52.6%) had high grade IVH. Strabismus developed in 30 infants (44.1%); 14 (46.6%) had low grade IVH; 16 (42.1%) had high grade IVH. Infants with high grade IVH were at significant greater risk than infants with low grade IVH for the development of optic atrophy (31.5% v 16.6%) and hydrocephalus (57.8% v 10%). Possible mechanisms of optic atrophy associated with IVH are hypoxia or a direct pressure effect on the optic nerves [9]. However, some studies found no association between the presence of IVH and ROP. King and Cronin [7] and Amato et al [23] found no statistically significant association between the presence of IVH and ROP. The study by Phillips et al [24] found no association between threshold ROP and the presence of IVH in 38 surviving very low birth-weight infants. It is likely that vascular immaturity, hypoxic ischemic trauma and free oxygen radicals are factors shared for both conditions [25, 26]. We conducted the current study in a large sample of infants of our region to obtain the reliable data. A large sample (n=1249) of examined preterm infants allowed for obtaining statistically significant results. In addition, we investigated incidences of various forms and stages of ROP among infants with IVH. Therefore, the results of our study demonstrate not only a statistically significant association between ROP and IVH, but also an increase in incidences of developing more severe ROP stages with an increase in IVH (p < 0.001). To conclude, first, infants with IVH had higher chances for developing ROP (OR=3.2; 95% CI, 2.5-4.2; p < 0.001). Second, infants with high-grade IVH had higher chances for developing particular stages and forms of the disease (stage 2 and threshold ROP) (OR=2.4; 95% CI, 1.7-3.35; p < 0.05). Finally, IVH was found to be a risk factor for developing ROP. References 1.Makhalev EV. [Clinical and pathological aspects of purulent meningitis in premature newborns with hypoxic injury to the central nervous system]. [Dr Sc (Med) dissertation]. Tomsk (Russia): Siberian State Medical University; 2000. Russian. 2.Nikolaieva GV. [Prevention of retinopathy in premature infants]. [Cand Sc (Med) thesis]. Moscow (Russia): Russian State Medical University; 2000. Russian. 3.Revta AM. [Optimizing monitoring of diagnosis, treatment and outcomes of active retinopathy of prematurity]. [Cand Sc (Med) thesis]. Arkhangelsk (Russia): Northern State Medical University; 2004. Russian. 4.Fedotova S, Adakhovska AO, Zaichko K, Katsan S. [Risk factors for the development of ROP in premature infants]. Oftalmologicheskii zhurnal Kazakhstana. 2017;1-2:69–77. Russian. 5.Volodin NN, Gorelyshev SK, Popov VE, editors. [Intraventricular hemorrhages and posthemorrhagic hydrocephalus in newborns. Principles for providing medical care. Guidelines]. Moscow; 2008. Russian. 6.Brown DR, Giglan AW, Stretavsky MM. Retinopathy of prematurity: the relationship with intraventricular haemorrhage and bronchopulmonary dysplasia. J Pediatr Ophthalmol Strabismus. 1990 Sep-Oct;27(5):268-71. 7.King KM, Cronin CM. Ocular findings in premature infants with grade IV intraventricular hemorrhage. J Pediatric Ophthalmol Strabismus. 1993 Mar-Apr;30(2):84-7. 8.Leech RW, Kohnen P. Subependymal and intraventricular haemorrhages in the newborn. Am J Pathol. 1974;77:465-75. 9.O’Keefe M, Kafil-Hussain N, Flitcroft I, Lanigan B. Ocular significance of intraventricular haemorrhage in premature infants. Br J Ophthalmol. 2001 Mar;85(3):357-9. 10.Sang GK, Port AD, Ryan S, et al. Retinopathy of Prematurity: A Review of Risk Factors and their Clinical Significance. Surv Ophthalmol. Sep-Oct 2018;63(5):618-637. 11.An International Committee for the Classification of Retinopathy of Prematurity. The International Classification of Retinopathy of Prematurity Revisited. Arch Ophthalmol. 2005 Jul;123(7):991-9. 12.ICD-10. Chapter XVI. Certain conditions originating in the perinatal period. 13.Lyakh YuE, Guryanov VG, Khomenko VN, Panchenko OA. [Basics of Computer Biostatistics. Data Analysis in biology, medicine and pharmacy statistical using statistical software Med Stat]. Donetsk: Papakitsa EK; 2006. Russian. 14.Jacobson L, Fernell E, Broberger U, Ek U, Gillberg C. Children with blindness due to retinopathy of prematurity: a population based study. Perinatal data, neurological and ophthalmological outcome. Dev Med Child Neurol. 1998 Mar;40(3):155-9. 15.Levene MI. Cerebral ultrasound and neurological impairment: telling the future. Arch Dis Child. 1990 May;65(5):469–71. 16.Tarby TJ, Volpe JJ. Intraventricular hemorrhage in the premature infant. Pediatr Clin North Am. 1982 Oct;29(5):1077-1104. 17.Volpe JJ. Neurologic outcome of prematurity. Arch Neurol. Arch Neurol. 1998 Mar;55(3):297-300. 18.Burstein J, Papile L, Burstein R. Subependymal germinal matrix and intraventricular hemorrhage in premature infants: diagnosis by CT. Am J Roentgen. 1997;128:971-6. 19.Bolisetty S, Dhawan A, Abdel-Latif M, et al. Intraventricular Hemorrhage and Neurodevelopmental Outcomes in Extreme Preterm Infants. Pediatrics. 2014 Jan;133(1):55-62. 20.Procianoy RS, Garcia-Prats JA, Hittner HM. An association between retinopathy of prematurity and intraventricular haemorrhage in very low birth infants. Acta Paediatr Scand. 1981 Jul;70(4):473-7. 21.Hungerford J, Stewart A, Hope P. Ocular sequelae of preterm birth and their relation to ultrasound evidence of cerebral damage. Br J Ophthalmol. 1986 Jun;70(6):463-8. 22.Charles JB, Ganthier R Jr, Appiah AP. Incidence and characteristics of retinopathy of prematurity in low-income inner-city population. Ophthalmology. 1991 Jan;98(1):14-7. 23.Amato M, Pasquier S, Muralt G. Incidence of retinopathy of prematurity in low birth weight infants with peri-intraventricular haemorrhage. Neuropediatrics. 1986 Nov;17(4):191-2. 24.Phillips J, Christiansen SP, Ware G. Ocular morbidity in very low birth-weight infants with intraventricular haemorrhage. Am J Ophthalmol. Am J Ophthalmol. 1997 Feb;123(2):218-23. 25.Mylonas C, Kouretas D. Lipid peroxidation and tissue damage. In Vivo. 1999 May-Jun;13(3):295-309. 26.Beligere N, Perumalswamy V, Tandon M, et al. Retinopathy of prematurity and neurodevelopmental disabilities in premature infants. Semin Fetal Neonat Med. Oct;20(5):346-53. The authors certify that they have no conflicts of interest in the subject matter or materials discussed in this manuscript.
|