J.ophthalmol.(Ukraine).2022;5:71-74.
|
http://doi.org/10.31288/oftalmolzh202257174 Received: 18.02.2022; Accepted: 27.06.2022; Published on-line: 27.10.2022 Pathomorphological features of the necrotic orbital wall lesions and orbital soft-tissue lesions in COVID-19-associated cavernous sinus thrombosis: a case report O. I. Oripov 1, E. N. Bilalov 1, R. I. Israilov 1, R. Z. Umarov 2, B. E. Bilalov 1, G. U. Khudaibergenov 1 1 Tashkent Medical Academy 2 Center for the Development of Professional Qualifications of Medical Workers Tashkent (Uzbekistan) TO CITE THIS ARTICLE: Oripov OI, Bilalov EN, Israilov RI, Umarov RZ, Bilalov BE, Khudaibergenov GU. Pathomorphological features of the necrotic orbital wall lesions and orbital soft-tissue lesions in COVID-19-associated cavernous sinus thrombosis: a case report. J.ophthalmol.(Ukraine).2022;5:71-74. http://doi.org/10.31288/oftalmolzh202257174
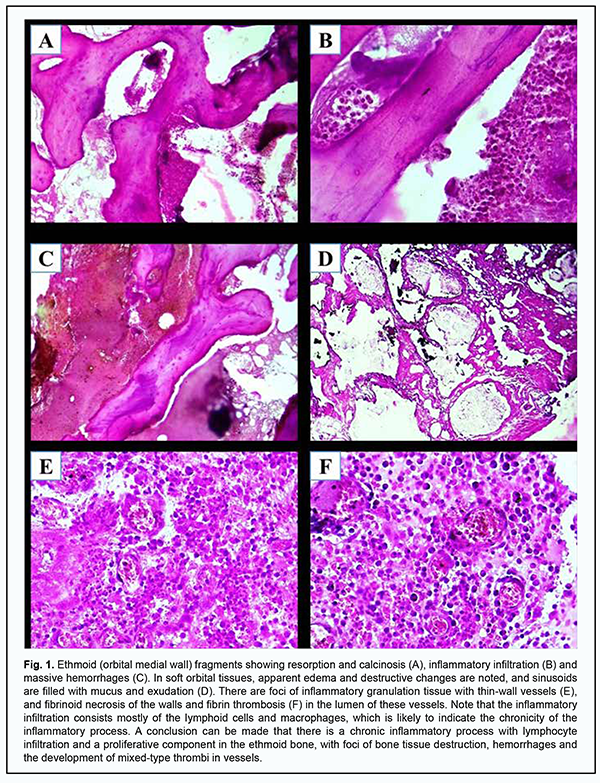
This paper describes a case of COVID-19-associated cavernous sinus thrombosis complicated by panophthalmitis, orbital cellulitis and necrotic purulent complications in other maxillofacial structures. In addition, we present the results of the pathomorphological study of orbital wall and orbital soft-tissue material excised during surgery. The pathomorphological findings in the orbital tissues included signs of a chronic inflammatory process with mostly lymphocyte infiltration, a proliferative component and development of mixed-type thrombi. Keywords: COVID-19, cavernous sinus thrombosis, orbital cellulitis, pathomorphological study
Introduction COVID-19-associated cavernous sinus thrombosis (CST) holds a special place among the eye diseases whose onset, course and outcome directly depend on COVID-19, since there is a significant increase in the prevalence of the COVID-19-associated CST in some global regions, which requires a comprehensive study of the disease to be conducted [1]. In addition, many questions regarding the pathogenesis of severe necrotic purulent lesions in the maxillofacial structures (e.g., the orbit) following the development of CST have not been answered yet. In this paper, we present the results of the pathomorpological study of the tissue obtained from a patient with COVID-19-associated CST complicated by the development of a severe necrotic purulent process in the orbit. The purpose of the study was to examine the pathomorpological features of the necrotic lesions in the orbital walls and soft tissues in COVID-19-associated CST. Case report A female patient, born in 1955, presented to the Department for the Treatment of COVID-19-associated Thrombovasculitis at the Multifield Clinic of Tashkent Medical Academy with complaints of severe pain in the right face, loss of sight in the right eye, blepharoptosis, apparent soft tissue edema in the right paraorbital area, general weakness, and elevated body temperature. Twenty-two days before presentation, she had been discharged from the hospital where she had been receiving specific therapy for severe COVID-19 and COVID-19-associated pneumonia with computer tomography (CT) evidence of the 2nd grade of lung involvement. She has type 2 diabetes of 12 years’ duration and receives insulin treatment. Right eye objective examination findings included apparent soft-tissue edema in the paraorbital region; chemosis; ptosis; 2nd grade exophthalmos; total ophthalmoplegia; decreased cutaneous sensation in the left paraorbital area; decreased corneal sensation; and anterior chamber hypopyon. In addition, ophthalmoscopy could not be accomplished due to hypopyon and vitritis. Multislice CT showed signs of right purulent pansinusitis with a lot of pus in the right maxillary sinus, destruction of the right ethmoid bone, and signs of the destruction of the right maxilla and hard palate. Magnetic resonance imaging (MRI; T2-TSE Dark Fluid protocol, 0.6-1.5-mm slices) findings included ophthalmic vein dilation; signs of parabulbar and retrobulbar fat edema and extraocular muscle edema; and expansion of the right cavernous sinus. Laboratory test results included: white blood cell count, 14.4 x 109/mm3; and erythrocyte sedimentation rate, 38 mm/h. Biochemical blood analyses included: C-reactive protein, 49 units; procalcitonin, 1.45 ng/ml; and ferritin, 650 µg/l. Blood coagulogram measurements included: activated partial thromboplastin time (APTT), 18 sec; fibrinogen, 580 g/l; and D-dimer, 1600 ng/ml. Based on the results of clinical and laboratory tests and imaging studies, the patient was clinically diagnosed with COVID-19-associated CST; panophthalmitis; periorbital cellulitis; right necrotic, purulent pansinusitis; and partial necrosis of the right maxilla and hard palate. The patient was administered preoperative conservative therapy to improve her clinical and laboratory parameters. This included continuous intravenous heparin infusion at a rate of 1500 IU/h every second day, with a target APTT value of ≥30 sec; Cefoperazone+Sulbactam 1.5 g, every other day; Metronidazole 100 ml intravenous infusion, twice a day; Fluconazole 100 ml intravenous infusion, every other day; Revmoxicam 2 ml intramuscularly, once a day; Neuromidin Revmoxicam 2 ml intramuscularly, once a day; Diacarb 200 mg, once a day; irrigation of the nasal cavity and paranasal sinuses with antiseptic solution, two to three times a day; Apdrops, two drops five times a day; and Nevanac, two drops three times a day. The therapy was given for 5 days. As a result, the stability of target parameter values was achieved, with a target APTT value of ≥30 sec, and twofold to threefold reduction in D-dimer, procalcitonin, and ferritin levels. It was decided to carry out a right orbital exenteration, right maxillary sinus surgery, and excision of the necrotic right hard palate and ethmoid bone. The conservative therapy was continued after surgery, and the patient stayed at the clinic, with daily irrigation of opened sinuses with antiseptic solution and application of a dressing for 12 days. An improvement in her condition was observed. The patient was discharged after stabilization of her general somatic status and relief of purulent inflammation. Further reconstructive surgical interventions were planned. Pathomorphological study The material (ethmoid and maxillary bone specimens and orbital soft tissue specimens) excised during surgery was sent for morphological examination. The material was fixed in 10% neutral buffer formaldehyde for 72 hours, rinsed with running water for at least two hours, dehydrated in ascending ethanol series and chloroform, and embedded in paraffine wax. The histological sections cut with a microtome were deparaffinized and dehydrated before staining them with hematoxylin and eosin. Results of Pathomorphological Study Specimens were analyzed for mucormycosis by microscopy using 10% potassium hydroxide (KOH) with Calcofluor white staining solution, and no rhizoid was found. Figure 1 shows photographs of the preparations and their descriptions.
Discussion Until now, only general predisposing factors (systemic coagulopathy and vasculitis) to COVID-19-associated CST thrombosis have been investigated sufficiently. It is still, however, unknown, what, aside of anatomic features of the sinus proper and veins in the maxillofacial area, is a specific local factor contributing to the development of CST [3, 4]. The medical community of India has grouped CST and other corona virus-associated necrotic purulent complications in the maxillifaceal, orbital and cerebral areas into a group of COVID-19-associated mucormycosis. This was caused by the fact that, in most cases, the relevant fungal infective agent has been identified as a major etiopathogenetic factor of the development of these complications based on the results of the relevant studies [5]. Mucormycosis studies in the Republic of Uzbekistan, however, have by far not always detected the agent in cases of the development of necrotic purulent process in CST [2]. In the case reported in this paper, we have also failed to detect mucormycosis by specific tissue staining, but our pathomorphological studies of the orbital soft-tissue structures detected foci of inflammatory granulation tissue with thin-wall vessels, signs of fibrinoid necrosis of the walls and fibrin thrombosis in the lumen of these vessels. It should be noted that the inflammatory infiltration at other sites of the maxillofacial area consisted mostly of the lymphoid cells and macrophages, which is likely to indicate the chronicity of the inflammatory process. In addition, the pathomorphological picture of orbital cellulitis was consistent with hard orbital cellulitis, with the development of a coagulative necrosis in unlysable and gradually rejected tissues. Considerable research is underway in the field of traumatology and orthopedics, focusing on coronavirus infection-associated aseptic femoral head necrosis. It should be noted that the pathomorphological studies have detected similar signs of specific viral lesions in bone tissues in cases of aseptic femoral head lesions [6]. Conclusion The development of necrotic process in the orbital structures in COVID-19-associated cavernous sinus thrombosis is characterized by a heterogenous pathomorphological picture, with sites of chronic inflammatory process with lymphocyte infiltration, sites with a proliferative component and development of mixed-type thrombi in vessels, which is likely to (1) be the sign of specific viral lesions and (2) indicate that the development of necrosis could be mediated by an autoimmune mechanism secondary to the action of the agent.
References 1.Sarker H. Cavernous Sinus Thrombosis after Recovery from COVID-19 – A Rare Case Report. Journal of Medical Science and Clinical Research. 2021;9. 2.Oripov OI, Bilalov EN. COVID-19-associated cavernous sinus thrombosis: a case report. J Ophthalmol (Ukraine). 2021;2:69-71. 3.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, et al. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;75:2950-73. 4.Klok FA, Kruip M, van der Meer NJM. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020; 191: 145-147. 5.Namiranian P, Razavi S, Karimi M, Ayati MH. Avascular Necrosis in Patients Recovering from COVID-19. Am J Med Sci. 2021; 362(3):331–2. 6.Veyre F, Poulain-Veyre C, Esparcieux A, Monsarrat N, Aouifi A, Lapeze J, Chatelard P. Femoral Arterial Thrombosis in a Young Adult after Nonsevere COVID-19. Ann Vasc Surg. 2020;69:85–88.
Disclosures Disclaimer: The opinions expressed in this article are the authors' own conclusions and the unofficial positions of the institution. Sources of Support: There are no additional sources of funding and support.
Conflict of Interest Statement: There is no conflict of interest.
|